Corrective Osteotomy After Damage of the Distal Radial Physis in Children: Surgical Technique and Results
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Volume 15, Issue 1, January-April
Volume 15, Issue 1, January-April Osteochondral lesions of the talus in adults J. Batista, G. Joannas, L. Casola, L. Logioco, G. Arrondo 1A Traumatic lesion with isolated cartilage injury (flap) Tx: arthroscopy, curettage, and microfractures. 1B Traumatic lesion (cartilage and subchondral bone injury) 1B.1 Lesion <10mm in diameter and <5mm of depth (superficial lesion) Tx: arthroscopy, curettage, and microfractures. 1B.2 Lesion >10mm in diameter and >5mm in depth Tx: fragment fixation with osteosynthesis, open surgery, osteochondral graft, or mosaicoplasty. 2A Non-traumatic isolated bone injury, subchondral cyst. Tx: retrograde drilling. 2B Non-traumatic open subchondral bone cyst with articular connection (progression of type 2A). 2B.1 Lesion measuring <10mm in diameter and <5mm in depth (superficial lesion). Tx: arthroscopy, curettage, and microfractures. 2B.2 Lesion measuring >10mm in diameter and >5mm in depth. Tx: open surgery, osteochondral graft, or mosaicoplasty. 3 Type 1 or 2 lesions associated with lateral instability of the ankle Tx: ligament repair. 4 With limb deformities 4A Types 1 or 2 lesions with hindfoot deformity = varus or valgus calcaneus Tx: varus or valgus calcaneal osteotomy. 4B Type 1 or 2 lesion with supramalleolar deformity of distal tibia (varus or valgus) Tx: varus or valgus supramalleolar osteotomy. Tx: treatment. Volume 15, Issue 1, January-April The Journal of the Foot & Ankle (eISSN 2675-2980) is published quarterly in April, August, and December, with the purpose of disseminating papers on themes of Foot and Ankle Medicine and Surgery and related areas. The Journal offers free and open access to your content on our website. All papers are already published with active DOIs. -

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -

The Use of Bone Age in Clinical Practice – Part 2
Mini Review HORMONE Horm Res Paediatr 2011;76:10–16 Received: March 25, 2011 RESEARCH IN DOI: 10.1159/000329374 Accepted: May 16, 2011 PÆDIATRIC S Published online: June 21, 2011 The Use of Bone Age in Clinical Practice – Part 2 a d f e b David D. Martin Jan M. Wit Ze’ev Hochberg Rick R. van Rijn Oliver Fricke g h j c George Werther Noël Cameron Thomas Hertel Stefan A. Wudy i k a a Gary Butler Hans Henrik Thodberg Gerhard Binder Michael B. Ranke a b Pediatric Endocrinology and Diabetology, University Children’s Hospital, Tübingen , Children’s Hospital, c University of Cologne, Cologne , and Paediatric Endocrinology and Diabetology, Justus Liebig University, Giessen , d e Germany; Department of Pediatrics, Leiden University Medical Center, Leiden , and Department of Radiology, f Emma Children’s Hospital/Academic Medical Center Amsterdam, Amsterdam , The Netherlands; Meyer Children’s g Hospital, Rambam Medical Center, Haifa , Israel; Department of Endocrinology, Royal Children’s Hospital h Parkville, Parkville, Vic. , Australia; Centre for Global Health and Human Development, Loughborough University, i Loughborough , and Institute of Child Health, University College London and University College London Hospital, j k London , UK; H.C. Andersen Children’s Hospital, Odense University Hospital, Odense , and Visiana, Holte , Denmark Key Words ness and cortical thickness should always be evaluated in -Skeletal maturity ؒ Bone age ؒ Tall stature ؒ relation to a child’s height and BA, especially around puber Precocious puberty ؒ Congenital adrenal hyperplasia ؒ ty. The use of skeletal maturity, assessed on a radiograph Bone mineral density alone to estimate chronological age for immigration author- ities or criminal courts is not recommended. -
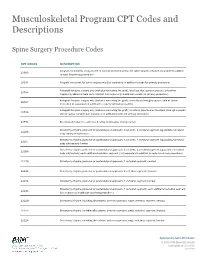
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Osteotomy Around the Knee: Evolution, Principles and Results
Knee Surg Sports Traumatol Arthrosc DOI 10.1007/s00167-012-2206-0 KNEE Osteotomy around the knee: evolution, principles and results J. O. Smith • A. J. Wilson • N. P. Thomas Received: 8 June 2012 / Accepted: 3 September 2012 Ó Springer-Verlag 2012 Abstract to other complex joint surface and meniscal cartilage Purpose This article summarises the history and evolu- surgery. tion of osteotomy around the knee, examining the changes Level of evidence V. in principles, operative technique and results over three distinct periods: Historical (pre 1940), Modern Early Years Keywords Tibia Osteotomy Knee Evolution Á Á Á Á (1940–2000) and Modern Later Years (2000–Present). We History Results Principles Á Á aim to place the technique in historical context and to demonstrate its evolution into a validated procedure with beneficial outcomes whose use can be justified for specific Introduction indications. Materials and methods A thorough literature review was The concept of osteotomy for the treatment of limb defor- performed to identify the important steps in the develop- mity has been in existence for more than 2,000 years, and ment of osteotomy around the knee. more recently pain has become an additional indication. Results The indications and surgical technique for knee The basic principle of osteotomy (osteo = bone, tomy = osteotomy have never been standardised, and historically, cut) is to induce a surgical transection of a bone to allow the results were unpredictable and at times poor. These realignment and a consequent transfer of weight bearing factors, combined with the success of knee arthroplasty from a damaged area to an undamaged area of joint surface. -

Viewed at a Minimum Follow-Up of 2 Years (Maximum of 3 Years and 9 Months)
J Orthopaed Traumatol (2012) 13 (Suppl 1):S57–S89 DOI 10.1007/s10195-012-0210-2 12 NOVEMBER 2012 In-Depth Oral Presentations and Oral Communications IN-DEPTH ORAL PRESENTATIONS achieve a stable synthesis and an early mobilization of the MP and IP joints. However, if a malunion is present, it has to be corrected sur- gically as soon as possible. AT05–HAND AND WRIST Radio-distal epiphysis fractures: treatment with angular stability Treatment of malunion of the proximal phalangeal fractures plate of latest generation of the hand R. Di Virgilio*, E. Coppari, E. Condarelli, M. Rendine V. Potenza*, S. Bisicchia, R. Caterini, A. Fichera, P. Farsetti, E. Ippolito (Rome, IT) Universita` di Roma Tor Vergata (Rome, IT) Introduction Distal radius fractures are the most common fractures of the upper limb and coincide with 17 % of all fractures treated in Introduction It is difficult to treat fractures of the phalanges of the emergency rooms. The incidence of these fractures is greater in hand because they can cause complications such as deformity and patients aged 6 to 10 years, and in those between 60 and 70 years. joint limitation with a reduction in the grasping function. The most In older patients the incidence is higher in females. In the articular frequent complications are malunion of the fracture and joint limi- fractures, displaced, dislocated and highly unstable is indicated tation. The greatest incidence of complications can be found in open internal fixation (ORIF) to restore the congruity of the joint transverse fractures of the base of the proximal phalanx, in articular surface, to restore the correct length of the radius, its inclination fractures, comminuted fractures, and in those associated with lesions and palmar tilt. -
Knee Surgery-Arthroscopic and Open Procedures Version 1.0 Effective February 14, 2020
CLINICAL GUIDELINES CMM-312: Knee Surgery-Arthroscopic and Open Procedures Version 1.0 Effective February 14, 2020 Clinical guidelines for medical necessity review of Comprehensive Musculoskeletal Management Services. © 2019 eviCore healthcare. All rights reserved. Comprehensive Musculoskeletal Management Guidelines V1.0 CMM-312: Knee Surgery-Arthroscopic and Open Procedures CMM-312.1: Definitions 3 CMM-312.2: General Guidelines 5 CMM-312.3: Indications and Non-Indications 5 CMM-312.4: Experimental, Investigational, or Unproven 15 CMM-312.5: Procedure (CPT®) Codes 16 CMM-312.6: Procedure (HCPCS) Codes 19 CMM-312.7: References 20 ______________________________________________________________________________________________________ ©2020 eviCore healthcare. All Rights Reserved. Page 2 of 25 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Comprehensive Musculoskeletal Management Guidelines V1.0 CMM -312.1: Definitions The Modified Outerbridge Classification is a system that has been developed for judging articular cartilage injury to the knee. This system allows delineation of varying areas of chondral pathology, based on the qualitative appearance of the cartilage surface, and can assist in identifying those injuries that are suitable for repair techniques. The characterization of cartilage in this system is as follows: Grade I – Softening with swelling Grade II – Fragmentation and fissuring less than one square centimeter (1 cm2) Grade III – Fragmentation and fissuring greater than one square centimeter -

Periacetabular Osteotomy (PAO) of the Hip
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines For Periacetabular Osteotomy (PAO) Of The Hip The hip joint is composed of the femur (the thigh bone) and the Lunate surface of acetabulum acetabulum (the socket formed Articular cartilage by the three pelvic bones). The Anterior superior iliac spine hip joint is a ball and socket joint Head of femur Anterior inferior iliac spine that not only allows flexion and extension, but also rotation of the Iliopubic eminence Acetabular labrum thigh and leg (Fig 1). The head of Greater trochanter (fibrocartilainous) the femur is encased by the bony Fat in acetabular fossa socket in addition to a strong, (covered by synovial) Neck of femur non-compliant joint capsule, Obturator artery making the hip an extremely Anterior branch of stable joint. Because the hip is Intertrochanteric line obturator artery responsible for transmitting the Posterior branch of weight of the upper body to the obturator artery lower extremities and the forces of Obturator membrane Ischial tuberosity weight bearing from the foot back Round ligament Acetabular artery up through the pelvis, the joint (ligamentum capitis) Lesser trochanter Transverse is subjected to substantial forces acetabular ligament (Fig 2). Walking transmits 1.3 to Figure 1 Hip joint (opened) lateral view 5.8 times body weight through the joint and running and jumping can generate forces across the joint fully form, the result can be hip that is shared by the whole hip, equal to 6 to 8 times body weight. dysplasia. This causes the hip joint including joint surfaces and the to experience load that is poorly previously-mentioned acetabular The labrum is a circular, tolerated over time, resulting in labrum. -

Pediatric Ankle Fractures
CHAPTER 26 PEDIATRIC ANKLE FRACTURES Sofi e Pinney, DPM, MS INTRODUCTION stronger than both the physis and bone. As a result, there is a greater capacity for plastic deformation and less chance of The purpose of this review is to examine the current intra-articular fractures, joint dislocation, and ligamentous literature on pediatric ankle fractures. I will discuss the disruptions. However, ligamentous injury may be more anatomic considerations of a pediatric patient, how to common than originally believed (1). A case-control study evaluate and manage these fractures, and when to surgically by Zonfrillo et al found an association between an increased repair them. Surgical techniques and complications will be risk of athletic injury in obese children, and concluded a briefl y reviewed. higher body mass index risk factor for ankle sprains (4). Ankle fractures are the third most common fractures in Secondary ossifi cation centers are located in the children, after the fi nger and distal radial physeal fracture. epiphysis. The distal tibial ossifi cation center appears at 6-24 Approximately 20-30% of all pediatric fractures are ankle months of age and closes asymmetrically over an 18-month fractures. Most ankle fractures occur at 8-15 years old. The period fi rst central, then medial and posterior, with the peak injury age is 11-12 years, and is relatively uncommon anterolateral portion closing last at 15 and 17 years of age for under the age 5. This injury is more common in boys. females and males, respectively. The distal fi bula ossifi cation The most common cause of pediatric ankle fractures is a center appears at 9-24 months of age and closes 1-2 years rotational force, and is often seen in sports injuries associated after the distal tibial. -

What Is the Impact of a Previous Femoral Osteotomy on THA?
Clin Orthop Relat Res (2019) 477:1176-1187 DOI 10.1097/CORR.0000000000000659 2018 Bernese Hip Symposium What Is the Impact of a Previous Femoral Osteotomy on THA? A Systematic Review Enrico Gallazzi MD, Ilaria Morelli MD, Giuseppe Peretti MD, Luigi Zagra MD 02/11/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= by https://journals.lww.com/clinorthop from Downloaded Downloaded from Received: 10 August 2018 / Accepted: 8 January 2019 / Published online: 17 April 2019 https://journals.lww.com/clinorthop Copyright © 2019 by the Association of Bone and Joint Surgeons Abstract by Background Femoral osteotomies have been widely used Questions/purposes In this systematic review, we asked: BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= to treat a wide range of developmental and degenerative hip (1) What are the most common complications after THA in diseases. For this purpose, different types of proximal fe- patients who have undergone femoral osteotomy, and how mur osteotomies were developed: at the neck as well as at frequently do those complications occur? (2) What is the the trochanteric, intertrochanteric, or subtrochanteric lev- survival of THA after previous femoral osteotomy? (3) Is els. Few studies have evaluated the impact of a previous the timing of hardware removal associated with THA femoral osteotomy on a THA; thus, whether and how a complications and survivorship? previous femoral osteotomy affects the -

Commercial Musculoskeletal Codes
Updated January 2018 Commercial Musculoskeletal Codes Investigational or Non-Covered Spine Surgery Pain Management Joint Surgery Codes associated with an Arthrogram CPT Description Commercial Notes Partial excision of posterior vertebral component (eg, spinous 22100 process, lamina or facet) for intrinsic bony lesion, single vertebral segment; cervical 22101 Partial excision of posterior vertebral component (eg, spinous process, lamina or facet) for intrinsic bony lesion, single vertebral segment; thoracic 22102 Partial excision of posterior vertebral component (eg, spinous process, lamina or facet) for intrinsic bony lesion, single vertebral segment; lumbar Partial excision of posterior vertebral component (eg, spinous process, 22103 lamina or facet) for intrinsic bony lesion, single vertebral segment; each additional segment (List separately in addition to code for primary procedure) Partial excision of vertebral body, for intrinsic bony lesion, without 22110 decompression of spinal cord or nerve root(s), single vertebral segment;cervical Partial excision of vertebral body, for intrinsic bony lesion, without 22112 decompression of spinal cord or nerve root(s), single vertebral segment; thoracic Partial excision of vertebral body, for intrinsic bony lesion, without 22114 decompression of spinal cord or nerve root(s), single vertebral segment; lumbar each additional vertebral segment (list separately in addition to code 22116 for primary procedure) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 22206 1 vertebral -

Ankle Injuries
Pediatric Fractures of the Ankle Nicholas Frane DO Zucker/Hofstra School of Medicine Northwell Health Core Curriculum V5 Disclosure • Radiographic Images Courtesy of: Dr. Jon-Paul Dimauro M.D or Christopher D Souder, MD, unless otherwise specified Core Curriculum V5 Outline • Epidemiology • Anatomy • Classification • Assessment • Treatment • Outcomes Core Curriculum V5 Epidemiology • Distal tibial & fibular physeal injuries 25%-38% of all physeal fractures • Ankle is the 2nd most common site of physeal Injury in children • Most common mechanism of injury Sports • 58% of physeal ankle fractures occur during sports activities • M>F • Commonly seen in 8-15y/o Hynes D, O'Brien T. Growth disturbance lines after injury of the distal tibial physis. Their significance in prognosis. J Bone Joint Surg Br. 1988;70:231–233 Zaricznyj B, Shattuck LJ, Mast TA, et al. Sports-related injuries in school-aged children. Am J Sports Med. 1980;8:318–324. Core Curriculum V5 Epidemiology Parikh SN, Mehlman CT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Ankle Fracture Pearls and Pitfalls. J Orthop Trauma. 2017;31 Suppl 6:S27-S31. doi:10.1097/BOT.0000000000001014 Spiegel P, et al. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am. 1978;60(8):1046-50. Core Curriculum V5 Anatomy • Ligamentous structures attach distal to the physis • Growth plate injury more likely than ligament failure secondary to tensile weakness in physis • Syndesmosis • Anterior Tibio-fibular ligament (AITFL) • Posterior Inferior Tibio-fibular