Identification and Validation of a Six Immune-Related Gene Signature For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modes of Interaction of KMT2 Histone H3 Lysine 4 Methyltransferase/COMPASS Complexes with Chromatin
cells Review Modes of Interaction of KMT2 Histone H3 Lysine 4 Methyltransferase/COMPASS Complexes with Chromatin Agnieszka Bochy ´nska,Juliane Lüscher-Firzlaff and Bernhard Lüscher * ID Institute of Biochemistry and Molecular Biology, Medical School, RWTH Aachen University, Pauwelsstrasse 30, 52057 Aachen, Germany; [email protected] (A.B.); jluescher-fi[email protected] (J.L.-F.) * Correspondence: [email protected]; Tel.: +49-241-8088850; Fax: +49-241-8082427 Received: 18 January 2018; Accepted: 27 February 2018; Published: 2 March 2018 Abstract: Regulation of gene expression is achieved by sequence-specific transcriptional regulators, which convey the information that is contained in the sequence of DNA into RNA polymerase activity. This is achieved by the recruitment of transcriptional co-factors. One of the consequences of co-factor recruitment is the control of specific properties of nucleosomes, the basic units of chromatin, and their protein components, the core histones. The main principles are to regulate the position and the characteristics of nucleosomes. The latter includes modulating the composition of core histones and their variants that are integrated into nucleosomes, and the post-translational modification of these histones referred to as histone marks. One of these marks is the methylation of lysine 4 of the core histone H3 (H3K4). While mono-methylation of H3K4 (H3K4me1) is located preferentially at active enhancers, tri-methylation (H3K4me3) is a mark found at open and potentially active promoters. Thus, H3K4 methylation is typically associated with gene transcription. The class 2 lysine methyltransferases (KMTs) are the main enzymes that methylate H3K4. KMT2 enzymes function in complexes that contain a necessary core complex composed of WDR5, RBBP5, ASH2L, and DPY30, the so-called WRAD complex. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Early Regionalization of the Otic Placode and Its Regulation by the Notch Signaling Pathway
Mechanisms of Development 124 (2007) 631–645 www.elsevier.com/locate/modo Early regionalization of the otic placode and its regulation by the Notch signaling pathway Gina Abello´, Safia Khatri, Fernando Gira´ldez, Berta Alsina * DCEXS-Universitat Pompeu Fabra, C/Dr. Aiguader 88, 08003 Barcelona, Spain Received 18 December 2006; received in revised form 11 April 2007; accepted 13 April 2007 Available online 20 April 2007 Abstract Otic neuronal precursors are the first cells to be specified and do so in the anterior domain of the otic placode, the proneural domain. In the present study, we have explored the early events of otic proneural regionalization in relation to the activity of the Notch signaling pathway. The proneural domain was characterized by the expression of Sox3, Fgf10 and members of the Notch pathway such as Delta1, Hes5 and Lunatic Fringe. The complementary non-neural domain expressed two patterning genes, Lmx1b and Iroquois1, and the mem- bers of the Notch pathway, Serrate1 and Hairy1. Fate map studies and double injections with DiI/DiO showed that labeled cells remained confined to anterior or posterior territories with limited cell intermingling. To explore whether Notch signaling pathway plays a role in the initial regionalization of the otic placode, Notch activity was blocked by a c-secretase inhibitor (DAPT). Notch blockade induced the expansion of non-neural genes, Lmx1 and Iroquois1, into the proneural domain. Combined gene expression and DiI exper- iments showed that these effects were not due to migration of non-neural cells into the proneural domain, suggesting that Notch activity regulates the expression of non-neural genes. -

Implications for 22Q11 Deletion Syndrome
Tbx1 haploinsufficiency is linked to behavioral disorders in mice and humans: Implications for 22q11 deletion syndrome Richard Paylora,b, Beate Glaserc,d, Annalisa Mupod,e,f,g, Paris Ataliotisd,h, Corinne Spencera,b, Angela Sobotkae, Chelsey Sparkse, Chul-Hee Choii, John Oghalaii, Sarah Curranj, Kieran C. Murphyk, Stephen Monksk, Nigel Williamsc, Michael C. O’Donovanc, Michael J. Owenc,l, Peter J. Scamblerh, and Elizabeth Lindsaye,f,m Departments of aMolecular and Human Genetics, bNeuroscience, ePediatrics (Cardiology), and iOtolaryngology, Baylor College of Medicine, Houston, TX 77030; cDepartment of Psychological Medicine, Cardiff University, Cardiff CF14 4XN, United Kingdom; fCEINGE Biotecnologie Avanzate and gEuropean School of Molecular Medicine (SEMM), 80145 Naples, Italy; hMolecular Medicine Unit, Institute of Child Health, 30 Guilford Street, London WC1N 1EH, United Kingdom; kDepartment of Psychiatry, Royal College of Surgeons in Ireland, Dublin 9, Ireland; and jDepartment of Psychological Medicine, Institute of Psychiatry, London SE4 8AF, United Kingdom Edited by Edward M. Scolnick, The Broad Institute, Cambridge, MA, and approved March 10, 2006 (received for review January 9, 2006) About 35% of patients with 22q11 deletion syndrome (22q11DS), which includes DiGeorge and velocardiofacial syndromes, devel- ops psychiatric disorders, mainly schizophrenia and bipolar disor- der. We previously reported that mice carrying a multigene dele- tion (Df1) that models 22q11DS have reduced prepulse inhibition (PPI), a behavioral abnormality and schizophrenia endophenotype. Impaired PPI is associated with several psychiatric disorders, in- cluding those that occur in 22q11DS, and recently, reduced PPI was reported in children with 22q11DS. Here, we have mapped PPI deficits in a panel of mouse mutants that carry deletions that partially overlap with Df1 and have defined a PPI critical region encompassing four genes. -

NICU Gene List Generator.Xlsx
Neonatal Crisis Sequencing Panel Gene List Genes: A2ML1 - B3GLCT A2ML1 ADAMTS9 ALG1 ARHGEF15 AAAS ADAMTSL2 ALG11 ARHGEF9 AARS1 ADAR ALG12 ARID1A AARS2 ADARB1 ALG13 ARID1B ABAT ADCY6 ALG14 ARID2 ABCA12 ADD3 ALG2 ARL13B ABCA3 ADGRG1 ALG3 ARL6 ABCA4 ADGRV1 ALG6 ARMC9 ABCB11 ADK ALG8 ARPC1B ABCB4 ADNP ALG9 ARSA ABCC6 ADPRS ALK ARSL ABCC8 ADSL ALMS1 ARX ABCC9 AEBP1 ALOX12B ASAH1 ABCD1 AFF3 ALOXE3 ASCC1 ABCD3 AFF4 ALPK3 ASH1L ABCD4 AFG3L2 ALPL ASL ABHD5 AGA ALS2 ASNS ACAD8 AGK ALX3 ASPA ACAD9 AGL ALX4 ASPM ACADM AGPS AMELX ASS1 ACADS AGRN AMER1 ASXL1 ACADSB AGT AMH ASXL3 ACADVL AGTPBP1 AMHR2 ATAD1 ACAN AGTR1 AMN ATL1 ACAT1 AGXT AMPD2 ATM ACE AHCY AMT ATP1A1 ACO2 AHDC1 ANK1 ATP1A2 ACOX1 AHI1 ANK2 ATP1A3 ACP5 AIFM1 ANKH ATP2A1 ACSF3 AIMP1 ANKLE2 ATP5F1A ACTA1 AIMP2 ANKRD11 ATP5F1D ACTA2 AIRE ANKRD26 ATP5F1E ACTB AKAP9 ANTXR2 ATP6V0A2 ACTC1 AKR1D1 AP1S2 ATP6V1B1 ACTG1 AKT2 AP2S1 ATP7A ACTG2 AKT3 AP3B1 ATP8A2 ACTL6B ALAS2 AP3B2 ATP8B1 ACTN1 ALB AP4B1 ATPAF2 ACTN2 ALDH18A1 AP4M1 ATR ACTN4 ALDH1A3 AP4S1 ATRX ACVR1 ALDH3A2 APC AUH ACVRL1 ALDH4A1 APTX AVPR2 ACY1 ALDH5A1 AR B3GALNT2 ADA ALDH6A1 ARFGEF2 B3GALT6 ADAMTS13 ALDH7A1 ARG1 B3GAT3 ADAMTS2 ALDOB ARHGAP31 B3GLCT Updated: 03/15/2021; v.3.6 1 Neonatal Crisis Sequencing Panel Gene List Genes: B4GALT1 - COL11A2 B4GALT1 C1QBP CD3G CHKB B4GALT7 C3 CD40LG CHMP1A B4GAT1 CA2 CD59 CHRNA1 B9D1 CA5A CD70 CHRNB1 B9D2 CACNA1A CD96 CHRND BAAT CACNA1C CDAN1 CHRNE BBIP1 CACNA1D CDC42 CHRNG BBS1 CACNA1E CDH1 CHST14 BBS10 CACNA1F CDH2 CHST3 BBS12 CACNA1G CDK10 CHUK BBS2 CACNA2D2 CDK13 CILK1 BBS4 CACNB2 CDK5RAP2 -

Whole Embryo Culture, Transcriptomics and RNA Interference Identify
Whole embryo culture, transcriptomics and RNA interference identify TBX1 and FGF11 as novel regulators of limb development in the mouse Gautier Tejedor, Béryl Laplace-Builhé, Patricia Luz-Crawford, Said Assou, Audrey Barthelaix, Marc Mathieu, Karima Kissa, Christian Jorgensen, Jérôme Collignon, Paul Chuchana, et al. To cite this version: Gautier Tejedor, Béryl Laplace-Builhé, Patricia Luz-Crawford, Said Assou, Audrey Barthelaix, et al.. Whole embryo culture, transcriptomics and RNA interference identify TBX1 and FGF11 as novel regulators of limb development in the mouse. Scientific Reports, Nature Publishing Group, 2020, 10 (1), pp.3597. 10.1038/s41598-020-60217-w. inserm-02498306 HAL Id: inserm-02498306 https://www.hal.inserm.fr/inserm-02498306 Submitted on 4 Mar 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. www.nature.com/scientificreports OPEN Whole embryo culture, transcriptomics and RNA interference identify TBX1 and FGF11 as novel regulators of limb development in the mouse Gautier Tejedor1,6, Béryl Laplace-Builhé1,6, Patricia Luz-Crawford3, Said Assou 1, Audrey Barthelaix1, Marc Mathieu1, Karima Kissa 4, Christian Jorgensen1,2, Jérôme Collignon 5,7, Paul Chuchana1,7 & Farida Djouad1,7* Identifying genes involved in vertebrate developmental processes and characterizing this involvement are daunting tasks, especially in the mouse where viviparity complicates investigations. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

Digeorge Subtypes of Nonsyndromic Conotruncal Defects: Evidence Against a Major Role of TBX1 Gene
European Journal of Human Genetics (2003) 11, 349–351 & 2003 Nature Publishing Group All rights reserved 1018-4813/03 $25.00 www.nature.com/ejhg SHORT REPORT DiGeorge subtypes of nonsyndromic conotruncal defects: evidence against a major role of TBX1 Gene Emanuela Conti1, Nicoletta Grifone1, Anna Sarkozy1,2, Caterina Tandoi1,2, Bruno Marino3, Maria Cristina Digilio4, Rita Mingarelli1, Antonio Pizzuti1,2 and Bruno Dallapiccola1,2 1CSS Hospital, IRCCS, San Giovanni Rotondo, Italy, and CSS-Mendel Institute, Rome, Italy; 2Section of Medical Genetics, Department of Experimental Medicine and Pathology, University ‘La Sapienza’, Rome, Italy; 3Section of Pediatric Cardiology, Institute of Pediatrics, University ‘La Sapienza’, Rome, Italy; 4Division of Medical Genetics, Bambino Gesu` Hospital, IRCCS, Rome, Italy The role of the 22q11 region genes, and among them TBX1, in nonsyndromic conotruncal defects (CTDs) is still unclear. Mice hemizygous at the Tbx1 locus show a remarkable incidence of heart outflow tract anomalies, of the same type commonly found in DiGeorge/Velo-cardio-facial syndrome (DGS/VCFS). Mutation analysis of the TBX1 gene in isolated, nonsyndromic CTDs has not demonstrated any functional pathogenetic variation so far. We screened the TBX1 gene in 41 patients affected by nonsyndromic CTDs of the DGS/VCFS subtype, principally ‘atypical’ tetralogy of Fallot. Besides a few polymorphisms, we did not find any pathogenetic variation. These results do not support a major role of the TBX1 gene as responsible for human nonsyndromic CTDs. European Journal of Human Genetics (2003) 11, 349–351. doi:10.1038/sj.ejhg.5200956 Keywords: TBX1; conotruncal heart defects; DiGeorge/Velo-cardio-facial syndrome Introduction modify the recurrence risk in isolated non-syndromic Conotruncal defects (CTDs) represent an important class of CTDs.7 All the evidences, therefore, agree with the multi- congenital heart diseases. -

Posterior Patterning of Esophagus Striated Muscle
RESEARCH ARTICLE A distinct cardiopharyngeal mesoderm genetic hierarchy establishes antero- posterior patterning of esophagus striated muscle Glenda Comai1,2†, Eglantine Heude1,2,3†, Sebastian Mella1,2, Sylvain Paisant1,2, Francesca Pala1,2,4, Mirialys Gallardo5, Francina Langa6, Gabrielle Kardon5, Swetha Gopalakrishnan1,2,7, Shahragim Tajbakhsh1,2* 1Department of Developmental and Stem Cell Biology, Institut Pasteur, Paris, France; 2CNRS UMR 3738, Paris, France; 3Department Adaptation du Vivant, CNRS/ MNHN UMR 7221, Muse´um national d’Histoire naturelle, Paris, France; 4Laboratory of Clinical Immunology and Microbiology (LCIM), National Institutes of Health, Bethesda, United States; 5Department of Human Genetics, University of Utah, Salt Lake City, United States; 6Mouse Genetics Engineering Center, Institut Pasteur, Paris, France; 7Institute of Biotechnology, HiLIFE, University of Helsinki, Helsinki, Finland Abstract In most vertebrates, the upper digestive tract is composed of muscularized jaws linked to the esophagus that permits food ingestion and swallowing. Masticatory and esophagus striated muscles (ESM) share a common cardiopharyngeal mesoderm (CPM) origin, however ESM are unusual among striated muscles as they are established in the absence of a primary skeletal muscle scaffold. Using mouse chimeras, we show that the transcription factors Tbx1 and Isl1 are required *For correspondence: cell-autonomously for myogenic specification of ESM progenitors. Further, genetic loss-of-function [email protected] and pharmacological studies point to MET/HGF signaling for antero-posterior migration of †These authors contributed esophagus muscle progenitors, where Hgf ligand is expressed in adjacent smooth muscle cells. equally to this work These observations highlight the functional relevance of a smooth and striated muscle progenitor dialogue for ESM patterning. -
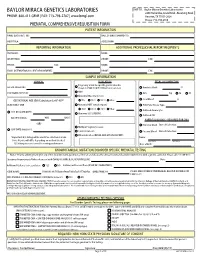
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Grimme, Acadia.Pdf
MECHANISM OF ACTION OF HISTONE DEACETYLASE INHIBITORS ON SURVIVAL MOTOR NEURON 2 PROMOTER by Acadia L. Grimme A thesis submitted to the Faculty of the University of Delaware in partial fulfillment of the requirements for the degree of Bachelors of Science in Biological Sciences with Distinction Spring 2018 © 2018 Acadia Grimme All Rights Reserved MECHANISM OF ACTION OF HISTONE DEACETYLASE INHIBITORS ON SURVIVAL MOTOR NEURON 2 PROMOTER by Acadia L. Grimme Approved: __________________________________________________________ Matthew E. R. Butchbach, Ph.D. Professor in charge of thesis on behalf of the Advisory Committee Approved: __________________________________________________________ Deni S. Galileo, Ph.D. Professor in charge of thesis on behalf of the Advisory Committee Approved: __________________________________________________________ Carlton R. Cooper, Ph.D. Committee member from the Department of Biological Sciences Approved: __________________________________________________________ Gary H. Laverty, Ph.D. Committee member from the Board of Senior Thesis Readers Approved: __________________________________________________________ Michael Chajes, Ph.D. Chair of the University Committee on Student and Faculty Honors ACKNOWLEDGMENTS I would like to acknowledge my thesis director Dr. Butchbach for his wonderful guidance and patience as I worked through my project. He has been an excellent research mentor over the last two years and I am forever thankful that he welcomed me into his lab. His dedication to his work inspires me as an aspiring research scientist. His lessons will carry on with me as I pursue future research in graduate school and beyond. I would like to thank both current and former members of the Motor Neuron Disease Laboratory: Sambee Kanda, Kyle Hinkle, and Andrew Connell. Sambee and Andrew patiently taught me many of the techniques I utilized in my project, and without them it would not be what it is today. -

T-Cell Lymphoma: Recent Advances in Characterization and New Opportunities for Treatment Carla Casulo, Owen O’Connor, Andrei Shustov, Michelle Fanale, Jonathan W
JNCI J Natl Cancer Inst (2017) 109(2): djw248 doi: 10.1093/jnci/djw248 First published online December 31, 2016 Review REVIEW T-Cell Lymphoma: Recent Advances in Characterization and New Opportunities for Treatment Carla Casulo, Owen O’Connor, Andrei Shustov, Michelle Fanale, Jonathan W. Friedberg, John P. Leonard, Brad S. Kahl, Richard F. Little, Lauren Pinter-Brown, Ranjani Advani, Steven Horwitz Affiliations of authors: Wilmot Cancer Center, University of Rochester, Rochester, NY (CC, JWF); Columbia University Medical Center, New York, NY (OO); Seattle Cancer Care Alliance, Seattle, WA (AS); University of Texas MD Anderson Cancer Center, Houston, TX (MF); Department of Medicine, Weil Cornell University, New York, NY (JPL); Oncology Division, Washington University, St. Louis, MO (BSK); Division of Cancer Treatment and Diagnosis, National Cancer Institute, Bethesda, MD (RFL); University of California-Irvine Chao Family Comprehensive Cancer Center in Orange, CA (LPB); Stanford Cancer Institute, Stanford University, Stanford, CA (RA); Memorial Sloan-Kettering Cancer Center, New York, NY (SH). Correspondence to: Carla Casulo, MD, Lymphoma Program, Wilmot Cancer Institute, University of Rochester, 601 Elmwood Avenue, Box 704, Rochester, NY 14642 (e-mail: [email protected]). REVIEW Abstract Peripheral T-cell lymphomas (PTCLs) are uncommon, heterogeneous, and aggressive non-Hodgkin’s lymphomas. Despite progress in the last several years resulting in a deeper understanding of PTCL biology and pathogenesis, there is currently no accepted single standard of care for newly diagnosed patients, and for those with relapsed or refractory disease, prognosis is dismal. The National Cancer Institute convened a Clinical Trials Planning Meeting to advance the national clinical trial agenda in lymphoma.