A Review on Variations in Lingual Foramina of the Mandible Midline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessment of Position of Mandibular and Genial Foramen in North Indian
Rathi S et al. Position of Mandibular and Genial Foramen. Journal of Advanced Medical and Dental Sciences Research @Society of Scientific Research and Studies Journal home page: www.jamdsr.comdoi: 10.21276/jamdsr (e) ISSN Online: 2321-9599; (p) ISSN Print: 2348-6805 Original Article Assessment of Position of Mandibu lar and Genial Foramen in North Indian Human Mandibles Sunita Rathi, Kumar Vaibhaw 1Assistant Professor, Department Of Anatomy, 2Assistant Professor, Department Of Pathology, Rama Medical College Hospital & Research Centre, Hapur, U.P. ABSTRACT: Introduction: The mandibular foramen is a prominent foramen and its knowledge is of paramount importance during dental procedures of lower jaw. Most common of the accessory foramina are the foramina present on the internal aspect of the bone. They are named as lingual foramina if the foramina are present in the midline, superior, or within the genial tubercle. The present study was undertaken to examine the incidence of the Mandibular Foramen and lingual (genial) foramen and their morphological variants by examining adult north Indian human mandibles from anthropology museum. Material and Methods: The present study was carried on 500 adult north Indian human mandibles from anthropology museum,. They were carefully examined and the incidence of the Mandibular Foramen and lingual (genial) foramen and their morphological variants was observed and noted after visual examination. Data obtained was studied and tabulated. Results: The position of mandibular foramen was more common below the midpoint, 451 cases (90.2%) while it was less common at the midpoint, 49 (9.8%) cases. In none of the mandibles examined, the position of the mandibular foramen was found above the midpoint. -

The Appearance of Foramen in the Internal Aspect of the Mental
Okajimas Folia Anat. Jpn., 82(3): 83–88, November, 2005 The Appearance of Foramen in the Internal Aspect of the Mental Region of Mandible from Japanese Cadavers and Dry Skulls Under Macroscopic Observation and Three-dimensional CT Images By Shunji YOSHIDA1),TaisukeKAWAI2),KoichiroOKUTSU2), Takashi YOSUE2), Hitoshi TAKAMORI3), Masataka SUNOHARA and Iwao SATO1) 1Department of Anatomy, 2Department of Oral and Maxillofacial Radiology School of Dentistry at Tokyo, 3Oral Implant Clinic, Nippon Dental University at Tokyo, Tokyo, Japan – Received for Publication, June 28, 2005 – Key Words: Lingual foramen, CT, Mandible Summary: The lingual canal with foramen displays different appearances on the internal surfaces of mandible as con- firmed by macroscopic observation and computerized tomography (CT). The lingual canal was observed in the inside of mental region run to the outside of lingual foramen, which is extend internally from mandibular canal in right and left sides of the mandible in cadavers (13 sides out of 88 sides) and in dry skulls (43 out of 94 sides) examined. The spinal foramen connected with mental canal occurred at the midline of mandible in 6 cases (6 out of 47 cases) in dry skulls. In this small foramen, the inferior alveolar artery give some branches to the inside of mental region at the anterior man- dible and which may be run pass through the lingual canal to the lingual foramen, where they emerge to enter the mylohyoid or anterior belly of digastric muscles. The observations of these are important considerations for surgical placement of dental implants in the region in the mandible. The anatomical location, course and arrange- treatments. -

Mechanics in the Production of Mandibular Technique. I
Mechanics in the Production of Mandibular Fractures: A Study with the "Stresscoat' Technique. I. Symphyseal Impacts DONALD F. HUELKE Department of Anatomy, University of Michigan Medical School Ann Arbor, Michigan A recent study of 319 case histories of mandibular fractures by Hagan and Huelke' has shown that certain areas of the jaw are fractured more often than others and that the incidence of certain mandibular fractures is greater when the blow is directed to specific regions of the jaw. Relatively little is known about the response of the mandi- ble to impact, except that, when the magnitude of a blow is sufficient, the bone will break. How does the mandible fracture, and what are the mechanisms involved? These questions have not been answered because of the lack of experimental data. Obtaining these data is an engineering problem involving stresses, strains, impacts, energies, and forces, and thus engineering techniques must be used. This report, the first of a series of studies on the mechanism of mandibular frac- tures, presents data on forces and impacts applied to the chin point of the mandible and the resultant deformations of the bone. The results of these tests are correlated with certain clinical findings. Terminology.-Throughout this report certain terminology generally used in engi- neering will be employed. Some of these terms need to be defined. The term force is defined as a push or pull. The various types of force are illustrated in Figure 1. Ten- sile forces (tension) tend to pull an object apart; compressive forces (compression) push the particles forming an object together, while shearing forces make one part of an object slide over another part of the same object. -

Download The
Review of the arterial anatomy in the anterior mandible Review of the arterial vascular anatomy for implant placement in the anterior mandible Abstract Objective José Carlos Balaguer Marti,* Juan Guarinos,† The placement of implants in the anterior region of the mandible is not Pedro Serrano Sánchez,† Amparo Ruiz Torner,* free of risk and can even sometimes be life-threatening. The aim of this * * David Peñarrocha Oltra & Miguel Peñarrocha Diago article is to review the anatomy of the anterior mandible regarding the *Department of Stomatology, Faculty of Medicine and placement of implants in this region. Odontology, University of Valencia, Valencia, Spain † Department of Anatomy, Faculty of Medicine and Materials and methods Odontology, University of Valencia, Valencia, Spain An anatomical study was conducted in cadavers to analyze the various Corresponding author: anatomical structures of the anterior region of the mandible. A literature review was also undertaken. Dr. David Peñarrocha Oltra Clínicas odontológicas Gascó Oliag, 1 46021 Valencia Results Spain The sublingual and submental arteries are the main supply of the sublin- T & F +34 963 86 4139 [email protected] gual region. These arteries are usually located at a safe distance from the alveolar ridge, but in cases of severe atrophy or anatomical variations, there may be an increased risk of damage during the placement of dental How to cite this article: implants and serious complications may arise. Balaguer Marti JC, Guarinos J, Serrano Sánchez P, Ruiz Torner A, Peñarrocha Oltra D, Peñarrocha Diago M. Conclusion Review of the arterial vascular anatomy for implant placement in the anterior mandible. The injury of the vessels in the floor of the mouth could lead to severe complications. -

Download Download
1 Contribution of dental private practitioners to 2 publications on anatomical variations using 3 cone beam computed tomography. 4 5 Authors: 6 Hebda A1,*MS, 7 Theys S2 DDS, 8 De Roissart J3 MD, 9 Perez E4 DDS, 10 Olszewski R1,3 DDS,MD,PhD,DrSc 11 Affiliations: 12 1 Oral and maxillofacial surgery research Lab, NMSK, IREC, SSS, UCLouvain, 13 Brussels, Belgium 14 2 Department of pediatric dentistry and special care, Cliniques universitaires saint 15 Luc, UCLouvain, Brussels, Belgium 16 3 Department of oral and maxillofacial surgery, Cliniques universitaires saint Luc, 17 UCLouvain, Brussels, Belgium 18 4 Department of orthodontics, Cliniques universitaires saint Luc, UCLouvain, 19 Brussels, Belgium 20 *Corresponding author: Hebda A, Oral and maxillofacial surgery research Lab, 21 NMSK, IREC, SSS, UCLouvain, Brussels, Belgium, ORCID Id 0000-0001-5111- 22 0021 1 2 [Nemesis] Titre de l’article (PUL - En- tête paire) 23 Disclaimer: the views expressed in the submitted article are our own and not an 24 official position of the institution or funder. 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 [Nemesis] Titre de l’article (PUL - En- tête impaire) 3 61 Abstract 62 Objective: To investigate the participation of citizens-dental private practitioner in 63 scientific articles about anatomical variations on dentomaxillofacial CBCT. Our null 64 hypothesis was that private practice practitioners are not involved in publications on 65 anatomical variations using cone beam computed tomography. -

Chapter 2 Implants and Oral Anatomy
Chapter 2 Implants and oral anatomy Associate Professor of Maxillofacial Anatomy Section, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University Tatsuo Terashima In recent years, the development of new materials and improvements in the operative methods used for implants have led to remarkable progress in the field of dental surgery. These methods have been applied widely in clinical practice. The development of computerized medical imaging technologies such as X-ray computed tomography have allowed detailed 3D-analysis of medical conditions, resulting in a dramatic improvement in the success rates of operative intervention. For treatment with a dental implant to be successful, it is however critical to have full knowledge and understanding of the fundamental anatomical structures of the oral and maxillofacial regions. In addition, it is necessary to understand variations in the topographic and anatomical structures among individuals, with age, and with pathological conditions. This chapter will discuss the basic structure of the oral cavity in relation to implant treatment. I. Osteology of the oral area The oral cavity is composed of the maxilla that is in contact with the cranial bone, palatine bone, the mobile mandible, and the hyoid bone. The maxilla and the palatine bones articulate with the cranial bone. The mandible articulates with the temporal bone through the temporomandibular joint (TMJ). The hyoid bone is suspended from the cranium and the mandible by the suprahyoid and infrahyoid muscles. The formation of the basis of the oral cavity by these bones and the associated muscles makes it possible for the oral cavity to perform its various functions. -

Evaluation of Mandibular Lingual Foramina Related to Dental Implant Treatment with Computerized Tomography: a Multicenter Clinical Study
IMPLANT DENTISTRY / V OLUME 23, NUMBER 1 2014 57 Evaluation of Mandibular Lingual Foramina Related to Dental Implant Treatment With Computerized Tomography: A Multicenter Clinical Study Yagmur D. Yildirim, DDS, PhD,* Güliz N. Güncü, DDS, PhD, † Pablo Galindo-Moreno, DDS, PhD,‡ Miguel Velasco-Torres, DDS, PhD,§ Gintaras Juodzbalys, DDS, PhD, k Marius Kubilius, DDS,¶ Albinas Gervickas, DDS, PhD,# Khalid Al-Hezaimi, DDS, MS,** Ra ’ed Al-Sadhan, DDS, MS, †† Hasan Güney Yilmaz, DDS, PhD, ‡‡ Neset Volkan Asar, DDS, PhD,§§ Erdem Karabulut, PhD, kk Hom-Lay Wang, DDS, MS, PhD,¶¶ and Tolga F. Tözüm, DDS, PhD## ental implant placement is Background: Bleeding can be larger measurements. The mean a routine and predictable tech- one of the severe complications diameter of lingual foramina was D nique for the replacement of during implant placement or other 0.89 6 0.40 mm; 76.8% canal type missing teeth. Interforaminal region surgeries. Presurgical assessment was mono; 51.8% patients presented is a good choice for the implant place- fi of the area should be performed with median lingual canal-foramen ment to support xed partial dentures precisely. Thus, we examined lin- (MLC) and 21.1% with lateral lin- or overdentures. Symphysis is one of the autologous donor graft area in the gual vascular canals of the mandi- gual foramen. Diameter of MLC ble using dental computerized was statistically larger. tomography (CT); de fine the ana- Conclusions: With a large sam- *Clinical Instructor, Department of Periodontology, Faculty of Dentistry, Hacettepe University, Ankara, Turkey. tomical characteristics of canals ple group, results represented that †Associate Professor, Department of Periodontology, Faculty of Dentistry, Hacettepe University, Ankara, Turkey. -
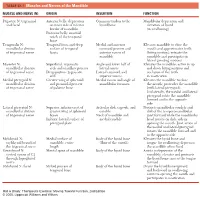
1 TABLE 23-1 Muscles and Nerves of the Mandible
0350 ch 23-Tab 10/12/04 12:19 PM Page 1 Chapter 23: The Temporomandibular Joint 1 TABLE 23-1 Muscles and Nerves of the Mandible MUSCLE AND NERVE (N) ORIGIN INSERTION FUNCTION Digastric N: trigeminal Anterior belly: depression Common tendon to the Mandibular depression and and facial on inner side of inferior hyoid bone elevation of hyoid border of mandible (in swallowing) Posterior belly: mastoid notch of the temporal bone Temporalis N: Temporal fossa and deep Medial and anterior Elevates mandible to close the mandibular division surface of temporal coronoid process and mouth and approximates teeth of trigeminal nerve fascia anterior ramus of (biting motion); retracts the mandible mandible and participates in lateral grinding motions Masseter N: Superficial: zygomatic Angle and lower half of Elevates the mandible; active in up mandibular division arch and maxillary process lateral ramus and down biting motions and of trigeminal nerve Deep portion: zygomatic Lateral coronoid and occlusion of the teeth arch superior ramus in mastication Medial pterygoid N: Greater wing of sphenoid Medial ramus and angle of Elevates the mandible to close mandibular division and pyramidal process mandibular foramen the mouth; protrudes the mandible of trigeminal nerve of palatine bone (with lateral pterygoid). Unilaterally, the medial and lateral pterygoid rotate the mandible forward and to the opposite side Lateral pterygoid N: Superior: inferior crest of Articular disk, capsule, and Protracts mandibular condyle and mandibular division greater wing of sphenoid condyle disk of the temporomandibular of trigeminal nerve bones Neck of mandible and joint forward while the mandibular Inferior: lateral surface of medial condyle head rotates on disk; aids in pterygoid plate opening the mouth. -

Evaluation of Medial Lingual Foramen with Cone-Beam Computed Tomography in a Turkish Adult Population
Original Article Evaluation of medial lingual foramen with cone-beam computed tomography in a Turkish adult population Nihat Laçin1 , Birkan Tatar1 , İlknur Veli2 , Artemisa Adıgüzel3 1 İzmir Katip Çelebi University, Faculty of Dentistry, Department of Oral and Maxillofacial Surgery, İzmir, Turkey 2 İzmir Katip Çelebi University, Faculty of Dentistry, Department of Orthodontics, İzmir, Turkey 3 Health Sciences University, Faculty of Dentistry, Department of Orthodontics, Istanbul, Turkey Abstract Aim: The aim of this study is to characterize the anatomical findings of the MLF in a Turkish population, using cone-beam computed tomography (CBCT). Methodology: The CBCT images of 350 untreated patients (164 male, 186 female ranging in age between 18 and 65) were included in this study. The distribution of MLFs were determined in axial, sagittal, and coronal planes by considering gender and side. For statistical evaluation, a chi- square test was used to analyze independent samples. P<0.05 was considered statistically significant. Correspondence: Results: At least 1 canal was observed in all subjects (n = 350). The most Dr. Nihat LAÇİN common result was a single canal. Among the 164 male patients (46.86%), İzmir Katip Çelebi University, Faculty of 98 had 1 canal (59.75%); 59 had 2 canals (35.97%); and 7 had 3 canals Dentistry, Department of Oral and (4.26%). Among the 186 female patients (53.14%), 134 (72.04%) had 1 Maxillofacial Surgery, İzmir, Turkey. conduit or canal; 49 (26.34%) had 2 canals; and only 3 case (1.61%) E-mail:[email protected] presented with 3 canals. Difference between genders was statistically Received: 1 October 2018 significant. -

Anatomy Respect in Implant Dentistry. Assortment, Location, Clinical Importance (Review Article)
ISSN: 2394-8418 DOI: https://doi.org/10.17352/jdps CLINICAL GROUP Received: 19 August, 2020 Review Article Accepted: 31 August, 2020 Published: 01 September, 2020 *Corresponding author: Dr. Rawaa Y Al-Rawee, BDS, Anatomy Respect in Implant M Sc OS, MOMS MFDS RCPS Glasgow, PhD, MaxFacs, Department of Oral and Maxillofacial Surgery, Al-Salam Dentistry. Assortment, Teaching Hospital, Mosul, Iraq, Tel: 009647726438648; E-mail: Location, Clinical Importance ORCID: https://orcid.org/0000-0003-2554-1121 Keywords: Anatomical structures; Dental implants; (Review Article) Basic implant protocol; Success criteria; Clinical anatomy Rawaa Y Al-Rawee1* and Mohammed Mikdad Abdalfattah2 https://www.peertechz.com 1Department of Oral and Maxillofacial Surgery, Al-Salam Teaching Hospital. Mosul, Iraq 2Post Graduate Student in School of Dentistry, University of Leeds. United Kingdom, Ministry of Health, Iraq Abstract Aims: In this article; we will reviews critically important basic structures routinely encountered in implant therapy. It can be a brief anatomical reference for beginners in the fi eld of dental implant surgeries. Highlighting the clinical importance of each anatomical structure can be benefi cial for fast informations refreshing. Also it can be used as clinical anatomical guide for implantologist and professionals in advanced surgical procedures. Background: Basic anatomy understanding prior to implant therapy; it's an important fi rst step in dental implant surgery protocol specifi cally with technology advances and the popularity of dental implantation as a primary choice for replacement loosed teeth. A thorough perception of anatomy provides the implant surgeon with the confi dence to deal with hard or soft tissues in efforts to restore the exact aim of implantation whether function or esthetics and end with improving health and quality of life. -
Radiography 1016105 Student Test Report on Midt 1 A
-, Radiography 1016105 Student Test Report On Midt 1 A Course #: 229 Instructor: Dr. S. Baden Course Title: Radiography Description: Radiography DayITime: TermNear: Fall 2005 Student ~m Student ID: Code: Possible Pts. Raw Obiective Subj./Essay Percent Grade MlDT 1: 22.00 18.00 18.00 0 81.82% B Response <dash> correct response <#> multiple marks <space> no response Description: <alphabet> student's incorrect response <*> bonus test item Test Items: 1-5 6-1 0 11-15 16-20 21-22 TestKey: E,B.D,E,C B,D,D,C,B A,C,D,A,C E,C,E,A,B D,A A - - - - D - - - - - - - - - - - Answers - 1 - ,- ,c 1 6 1 1 , 1 1 1 1 1 , , , , , Remarks: Student's Answer to Multiple Mark Question: No multiple mark answers or answer keys found on this test - Name - Place the following films in the correct position in the film mount. /Lf - d AlI slms have the bump facing up. 1 I I Name Basic Principles of Radiology Multiple choice: Choose the best single answer. 1. The key interproximal space for a maxillary right premolar PA is between. a.#2and3 b. # 13 and 14 c.#4and5 d. # 12 and 13 e.#3and4 2. Which of the following would not be seen in a maxillary central PA? a. lip b. ethrnoid sinus c. incisive foramen d. vomer e. nose 3. What would you change to make a film darker? a increase developing time b. increase mA setting c. decreased kVp setting d. increase exposure time e. decrease developing time 4. Which of the following has the highest percent interaction with biological tissues? a. -
Smithsonian Miscellaneous Collections
SMITHSONIAN MISCELLANEOUS COLLECTIONS VOLUME 121, NUMBER 8 WESTERN ATLANTIC SCORPIONFISHES BY ISAAC GINSBURd U. S. Fish and Wildlife Service -f'SS^af-o m (Publication 4106) CITY OF WASHINGTON PUBLISHED BY THE SMITHSONIAN INSTITUTION MAY 28, 1953 SMITHSONIAN MISCELLANEOUS COLLECTIONS VOLUME 121, NUMBER 8 WESTERN ATLANTIC SCORPIONFISHES BY ISAAC GINSBURG U. S. Fish and Wildlife Service (Publication 4106) CITY OF WASHINGTON PUBLISHED BY THE SMITHSONIAN INSTITUTION MAY 28, 1953 2^^e Bovi (§&itimovi (preec BALTIMORE, MS., n. S. A. WESTERN ATLANTIC SCORPIONFISHES By ISAAC GINSBURG U. S. Fish and Wildlife Service INTRODUCTION The present state of the taxonomy of the western Atlantic scor- paenids leaves much to be desired. The literature is filled with inade- quate original or supplementary descriptions of species, containing many unessential details of little or no practical use for the correct determination of the species, while the critical characters that dis- tinguish the species often are not considered adequately. I found it well-nigh impossible to identify and distinguish the species properly by the use of current accounts. One of the main factors that operate to bedevil the taxonomist who conscientiously tries to identify his specimens is the undue multiplication by past authors of the number of fictitious species. Such untenable "species" have been established, in large measure, as a result of failure to elaborate properly, or even to take into consideration, the intraspecific range of variability of taxonomic characters, or their change with growth which, in the scorpaenids, is considerable. The multiplication of names that have been proposed for scorpaenid species that have no existence in fact is as confusing as the grouping of two or more closely related species under one name that has entered into the literature of other families.