Calcium Chloride
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix a Common Abbreviations Used in Medication
UNIVERSITY OF AMSTERDAM MASTERS THESIS Impact of Medication Grouping on Fall Risk Prediction in Elders: A Retrospective Analysis of MIMIC-III Critical Care Database Student: SRP Mentor: Noman Dormosh Dr. Martijn C. Schut Student No. 11412682 – SRP Tutor: Prof. dr. Ameen Abu-Hanna SRP Address: Amsterdam University Medical Center - Location AMC Department Medical Informatics Meibergdreef 9, 1105 AZ Amsterdam Practice teaching period: November 2018 - June 2019 A thesis submitted in fulfillment of the requirements for the degree of Master of Medical Informatics iii Abstract Background: Falls are the leading cause of injury in elderly patients. Risk factors for falls in- cluding among others history of falls, old age, and female gender. Research studies have also linked certain medications with an increased risk of fall in what is called fall-risk-increasing drugs (FRIDs), such as psychotropics and cardiovascular drugs. However, there is a lack of consistency in the definitions of FRIDs between the studies and many studies did not use any systematic classification for medications. Objective: The aim of this study was to investigate the effect of grouping medications at different levels of granularity of a medication classification system on the performance of fall risk prediction models. Methods: This is a retrospective analysis of the MIMIC-III cohort database. We created seven prediction models including demographic, comorbidity and medication variables. Medica- tions were grouped using the anatomical therapeutic chemical classification system (ATC) starting from the most specific scope of medications and moving up to the more generic groups: one model used individual medications (ATC level 5), four models used medication grouping at levels one, two, three and four of the ATC and one model did not include med- ications. -

Chemicals Used for Chemical Manufacturing Page 1 of 2
Chemicals used for Chemical Manufacturing Page 1 of 2 Acetic Acid (Glacial, 56%) Glycol Ether PMA Acetone Glycol Ether PNB Acrylic Acid Glycol Ether PNP Activated Carbon Glycol Ether TPM Adipic Acid Glycols Aloe Vera Grease Aluminum Stearate Gum Arabic Aluminum Sulfate Heat Transfer Fluids Amino Acid Heptane Ammonium Acetate Hexane Ammonium Bicarbonate Hydrazine Hydrate Ammonium Bifluoride Hydrochloric Acid (Muriatic) Ammonium Chloride Hydrogen Peroxide Ammonium Citrate Hydroquinone Ammonium Hydroxide Hydroxylamine Sulfate Ammonium Laureth Sulfate Ice Melter Ammonium Lauryl Sulfate Imidazole Ammonium Nitrate Isobutyl Acetate Ammonium Persulfate Isobutyl Alcohol Ammonium Silicofluoride Calcium Stearate Dipropylene Glycol Isopropanolamine Ammonium Sulfate Carboxymethylcellulose Disodium Phosphate Isopropyl Acetate Antifoams Caustic Potash D'Limonene Isopropyl Alcohol Antifreeze Caustic Soda (All Grades) Dodecylbenzene Sulfonic Acid Isopropyl Myristate Antimicrobials Caustic Soda (Beads, Prills) (DDBSA) Isopropyl Palmitate Antimony Oxide Cetyl Alcohol Dowfrost Itaconic Acid Aqua Ammonia Cetyl Palmitate Dowfrost HD Jojoba Oil Ascorbic Acid Chlorine, Granular Dowtherm SR-1 Keratin Barium Carbonate Chloroform Dowtherm 4000 Lactic Acid Barium Chloride Chromic Acid EDTA Lanolin Beeswax Citric Acid (Dry and Liquid) EDTA Plus Lauric Acid Bentonite Coal Epsom Salt Lauryl Alcohol Benzaldehyde Cocamide DEA Ethyl Acetate Lecithin Benzoic Acid Copper Nitrate Ethyl Alcohol (Denatured) Lime Benzyl Alcohol Copper Sulfate Ethylene Glycol Linoleic Acid Bicarbonate -

Chlorthalidone Is Superior to Potassium Citrate in Reducing Calcium Phosphate Stones and Increasing Bone Quality in Hypercalciuric Stone-Forming Rats
BASIC RESEARCH www.jasn.org Chlorthalidone Is Superior to Potassium Citrate in Reducing Calcium Phosphate Stones and Increasing Bone Quality in Hypercalciuric Stone-Forming Rats Nancy S. Krieger,1 John R. Asplin,2 Ignacio Granja,2 Felix M. Ramos,1 Courtney Flotteron,1 Luojing Chen,1 Tong Tong Wu,3 Marc D. Grynpas,4 and David A. Bushinsky1 1Division of Nephrology, Department of Medicine, University of Rochester School of Medicine and Dentistry, Rochester, New York; 2Litholink Corporation, Laboratory Corporation of America Holdings, Chicago, Illinois; 3Department of Biostatistics and Computational Biology, University of Rochester School of Medicine, Rochester, New York; and 4Lunenfeld-Tanenbaum Research Institute, Mount Sinai Hospital, Toronto, Ontario, Canada ABSTRACT Background The pathophysiology of genetic hypercalciuric stone-forming rats parallels that of human idiopathic hypercalciuria. In this model, all animals form calcium phosphate stones. We previously found that chlorthalidone, but not potassium citrate, decreased stone formation in these rats. Methods To test whether chlorthalidone and potassium citrate combined would reduce calcium phos- phate stone formation more than either medication alone, four groups of rats were fed a fixed amount of a normal calcium and phosphorus diet, supplemented with potassium chloride (as control), potassium citrate, chlorthalidone (with potassium chloride to equalize potassium intake), or potassium citrate plus chlorthalidone. We measured urine every 6 weeks and assessed stone formation and bone quality at 18 weeks. Results Potassium citrate reduced urine calcium compared with controls, chlorthalidone reduced it fur- ther, and potassium citrate plus chlorthalidone reduced it even more. Chlorthalidone increased urine citrate and potassium citrate increased it even more; the combination did not increase it further. -

Bactericide-Disinfectant
, r f.~ n,r.~il·'\L H.. ~t.t;I" "" . i ltM)"ft . "' .' .,.,,~: .. ;;:.~ ,.;·~~~t:.:.· ,.J.~ . ... --' "'.~.};" ,",>;"'!:,., ~ " .. ". , ; IlUNGtCIOE' MID RCOfNTlCtOI .. ~.' ".' • ., . <",~. .. ,'. 1 ~Of: ~~Itr. ,<"{}~ _ t EO IJ"OS~A C :J-) l - (BACTERICIDE -DISINFECTANT) DESC Rlt.JllC"N: P''1k'or is a nor-sudsing, chlorinated, perman a solution can be recommended for dairy utensils, milking ma 4. For home l gana·ed o~tprger.t F'owaE'r for q'Jick, efficient cleaning, disin chines and equipment. The same solution can be us~d on dairy water for dis fecting, sani rizing and (JE:odorizir,g. It is designed for use on all farm utensils as well as washing cows' udders and milkr.:rs' utensils. For c11 types of equipment and utensils that are used in the handling hands. surfaces such of food products, milk, meats, beverages, etc. Authorized for ounce per que use under the U. S. Department of Agriculture Consumer and 2. Pinklor can be used very effec1ively in food and beveraqe Marketing Service Inspection Programs for poultry, meat, milk plants as a disinfectant for equipment using a solution of 1 and egg product plants. F oer 40 gallons of water and applying this solution in DANGI c.. i.:,.'r that insures conto(t '/./ith all po "ts and surfaces. OREN. AVOI Specifications 0 STUFFS. HAF Active: Trisodium Phosphate (hydrated) over 91.00 0 3. Where local and state regulations are in effect, consu:t Sodium Hypochlorite over 3.500 0 rules of you" local authorities tor volume of chlorine required SKIN OR IN 0 Sodium Lauryl Sulfate under 0.05 0 in rinse solutil'ns. -
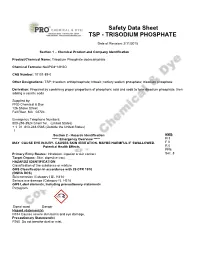
Safety Data Sheet TSP - TRISODIUM PHOSPHATE
Safety Data Sheet TSP - TRISODIUM PHOSPHATE Date of Revision: 2/11/2015 Section 1 – Chemical Product and Company Identification Product/Chemical Name: Trisodium Phosphate dodecahydrate Chemical Formula: Na3PO4*12H2O CAS Number: 10101-89-0 Other Designations: TSP; trisodium orthophosphate; tribasic; tertiary sodium phosphate; trisodium phosphate Derivation: Prepared by combining proper proportions of phosphoric acid and soda to form disodium phosphate, then adding a caustic soda Supplied by: PRO Chemical & Dye 126 Shove Street Fall River, MA 02724 Emergency Telephone Numbers: 800-255-3924 ChemTel. (United States) + 1 01 813-248-0585 (Outside the United States) 1. Section 2 - Hazards Identification HMIS ***** Emergency Overview ***** H 3 MAY CAUSE EYE INJURY. CAUSES SKIN IRRITATlON. MAYBE HARMFUL IF SWALLOWED. F 0 Potential Health Effects R 0 PPE Primary Entry Routes: Inhalation, ingestion or skin contact. Sec. 8 Target Organs: Skin, digestive tract. HAZARDS IDENTIFICATION Classification of the substance or mixture GHS Classification in accordance with 29 CFR 1910 (OSHA DCS) Skin corrosion (Category I B). H314 Serious eye damage (Category I). H318 GHS Label elements, including precautionary statements Pictogram Signal word Danger Hazard statement(s) H314 Causes severe skin burns and eye damage. Precautionary Statement(s) P260 Do not breathe dust or mist. P264 Wash skin thoroughly after handling. P280 Wear protective gloves protective clothing/ eye protection/ face protection. P301 + P330 + P331 IF SWALLOWED: rinse mouth. DO NOT induce vomiting. P303 + P36l + P353 IF ON SKIN (or hair): Remove. Take off immediately all contaminated clothing. Rinse skin with water / shower. P304 + P340 IF INHALED: Remove victim to fresh air and keep at rest in a position comfortable for breathing. -

CX/FA 18/50/5 January 2018 JOINT FAO/WHO FOOD STANDARDS
E Agenda Item 4 (a) CX/FA 18/50/5 January 2018 JOINT FAO/WHO FOOD STANDARDS PROGRAMME CODEX COMMITTEE ON FOOD ADDITIVES Fiftieth Session ENDORSEMENT AND/OR REVISION OF MAXIMUM LEVELS FOR FOOD ADDITIVES AND PROCESSING AIDS IN CODEX STANDARDS BACKGROUND 1. In accordance with the section concerning Relations between Commodity Committees and General Committees of the Codex Alimentarius Commission Procedural Manual, “All provisions in respect of food additives (including processing aids) contained in Codex commodity standards should be referred to the Committee on Food Additives, preferably before the Standards have been advanced to Step 5 of the Procedure for the Elaboration of Codex Standards or before they are considered by the commodity committee concerned at Step 7, though such referral should not be allowed to delay the progress of the Standard to the subsequent Steps of the Procedure.”. 2. The following food additive and processing aids provisions of Codex standards have been submitted for endorsement since the 49th Session of the Codex Committee on Food Additives and are listed by: (i) Technological function, INS number and food additive name; (ii) Maximum level; (iii) ADI (mg additive/kg body weight per day); and (iv) Notes. 3. The following abbreviations have been used in the preparation of this paper: INS International Numbering System for food additives. The INS (INS) is intended as a harmonised naming system for food additives as an alternative to the use of the specific name, which may be lengthy1. ADI Acceptable Daily Intake. An estimate of the amount of a substance in food or drinking-water, expressed on a body-weight basis, that can be ingested daily over a lifetime without appreciable risk (standard human = 60 kg)2. -

Calcium Chloride CAS N°:10043-52-4
OECD SIDS CALCIUM CHLORIDE FOREWORD INTRODUCTION Calcium chloride CAS N°:10043-52-4 UNEP PUBLICATIONS 1 OECD SIDS CALCIUM CHLORIDE SIDS Initial Assessment Report For SIAM 15 Boston, USA 22-25th October 2002 1. Chemical Name: Calcium chloride 2. CAS Number: 10043-52-4 3. Sponsor Country: Japan National SIDS Contact Point in Sponsor Country: Mr. Yasuhisa Kawamura Director Second Organization Div. Ministry of Foreign Affairs 2-2-1 Kasumigaseki, Chiyoda-ku Tokyo 100 4. Shared Partnership with: 5. Roles/Responsibilities of the Partners: • Name of industry sponsor Tokuyama Corporation /consortium Mr. Shigeru Moriyama, E-mail: [email protected] Mr. Norikazu Hattori, E-mail: [email protected] • Process used 6. Sponsorship History • How was the chemical or This substance is sponsored by Japan under ICCA Initiative and category brought into the is submitted for first discussion at SIAM 15. OECD HPV Chemicals Programme ? 7. Review Process Prior to The industry consortium collected new data and prepared the the SIAM: updated IUCLID, and draft versions of the SIAR and SIAP. Japanese government peer-reviewed the documents, audited selected studies. 8. Quality check process: 9. Date of Submission: 10. Date of last Update: 2 UNEP PUBLICATIONS OECD SIDS CALCIUM CHLORIDE 11. Comments: No testing (X) Testing ( ) The CaCl2-HPV Consortium members: (Japan) Asahi Glass Co., Ltd. Central Glass Co., Ltd. Sanuki Kasei Co., Ltd. Tokuyama Corporation [a global leader of the CaCl2-HPV Consortium] Tosoh Corporation (Europe) Brunner Mond (UK) Ltd. Solvay S.A. (North America) The Dow Chemical Company General Chemical Industrial Products Inc. Tetra Technologies, Inc. -

Potassium-Magnesium Citrate Is an Effective Prophylaxis Against Recurrent Calcium Oxalate Nephrolithiasis
0022-5347/97/1586-2069$03.00/0 JOURNAL OF UROLOGY Vol. 158,2069-2073, December 1997 Copyright Q 1997 by AMERICANUROLOGICAL ASS~CIATION, INC. Printed in U.S.A. POTASSIUM-MAGNESIUM CITRATE IS AN EFFECTIVE PROPHYLAXIS AGAINST RECURRENT CALCIUM OXALATE NEPHROLITHIASIS BRUCE ETTINGER,* CHARLES Y. C. PAK, JOHN T. CITRON, CARL THOMAS, BEVERLEY ADAMS-HIJET AND ARLINE VANGESSEL From the Diuision of Research, Kaiser Permanente Medical Care Program, Oakland, California, the Department of Mineral Metabolism, Center for Mineral Metabolism and Clinical Research, University of Texas Southwestern Medical Center at Dallas, Dallas, Texas, Department of Medicine, Kaiser Permanente Medical Center, Walnut Creek, California, Department of Urology, Kaiser Permanente Medical Center, San Francisco, California, and Kaiser Foundation Research Institute, Kaiser Foundation Hospitals, Oakland, California ABSTRACT Purpose: We examined the efficacy of potassium-magnesium citrate in preventing recurrent calcium oxalate kidney calculi. Materials and Methods: We conducted a prospective double-blind study of 64 patients who were randomly assigned to receive placebo or potassium-magnesium citrate (42 mEq. potassium, 21 mEq. magnesium, and 63 mEq. citrate) daily for up to 3 years. Results. New calculi formed in 63.6%of subjects receiving placebo and in 12.9%of subjects receiving potassium-magnesiumcitrate. When compared with placebo, the relative risk of treat- ment failure for potassium-magnesium citrate was 0.16 (95%confidence interval 0.05 to 0.46). potassium-magnesium citrate had a statistically significant effect (relative risk 0.10,95%confi- dence interval 0.03 to 0.36) even after adjustment for possible confounders, including age, pretreatment calculous event rate and urinary biochemical abnormalities. -

Electro-Activation of Potassium Acetate, Potassium Citrate and Calcium
Liato et al. SpringerPlus (2016) 5:1760 DOI 10.1186/s40064-016-3453-1 RESEARCH Open Access Electro‑activation of potassium acetate, potassium citrate and calcium lactate: impact on solution acidity, Redox potential, vibrational properties of Raman spectra and antibacterial activity on E. coli O157:H7 at ambient temperature Viacheslav Liato1,2, Steve Labrie1,3 and Mohammed Aïder1,2,4* *Correspondence: [email protected] Abstract 1 Institute of Nutrition and Functional Foods (INAF), Aims: To study the electro-activation of potassium acetate, potassium citrate and Université Laval, Quebec, QC calcium lactate aqueous solutions and to evaluate their antimicrobial effect against E. G1V 0A6, Canada coli O157:H7 at ambient temperature. Full list of author information is available at the end of the Methods and results: Potassium acetate, potassium citrate and calcium lactate aque- article ous solutions were electrically excited in the anodic compartment of a four sectional electro-activation reactor. Different properties of the electro-activated solutions were measured such as: solutions acidity (pH and titratable), Redox potential and vibrational properties by Raman spectroscopy. Moreover, the antimicrobial activity of these solu- tions was evaluated against E. coli O157:H7. The results showed a pH decrease from 7.07 0.08, 7.53 0.12 and 6.18 0.1 down to 2.82 0.1, 2.13 0.09 and 2.26 0.15, after ±180 min of electro-activation± ± of potassium acetate,± potassium± citrate and calcium± lactate solution, respectively. These solutions were characterized by high oxidative ORP of 1076 12, 958 11 and 820 14 mV, respectively. -

US EPA Inert (Other) Pesticide Ingredients
U.S. Environmental Protection Agency Office of Pesticide Programs List of Inert Pesticide Ingredients List 3 - Inerts of unknown toxicity - By Chemical Name UpdatedAugust 2004 Inert Ingredients Ordered Alphabetically by Chemical Name - List 3 Updated August 2004 CAS PREFIX NAME List No. 6798-76-1 Abietic acid, zinc salt 3 14351-66-7 Abietic acids, sodium salts 3 123-86-4 Acetic acid, butyl ester 3 108419-35-8 Acetic acid, C11-14 branched, alkyl ester 3 90438-79-2 Acetic acid, C6-8-branched alkyl esters 3 108419-32-5 Acetic acid, C7-9 branched, alkyl ester C8-rich 3 2016-56-0 Acetic acid, dodecylamine salt 3 110-19-0 Acetic acid, isobutyl ester 3 141-97-9 Acetoacetic acid, ethyl ester 3 93-08-3 2'- Acetonaphthone 3 67-64-1 Acetone 3 828-00-2 6- Acetoxy-2,4-dimethyl-m-dioxane 3 32388-55-9 Acetyl cedrene 3 1506-02-1 6- Acetyl-1,1,2,4,4,7-hexamethyl tetralin 3 21145-77-7 Acetyl-1,1,3,4,4,6-hexamethyltetralin 3 61788-48-5 Acetylated lanolin 3 74-86-2 Acetylene 3 141754-64-5 Acrylic acid, isopropanol telomer, ammonium salt 3 25136-75-8 Acrylic acid, polymer with acrylamide and diallyldimethylam 3 25084-90-6 Acrylic acid, t-butyl ester, polymer with ethylene 3 25036-25-3 Acrylonitrile-methyl methacrylate-vinylidene chloride copoly 3 1406-16-2 Activated ergosterol 3 124-04-9 Adipic acid 3 9010-89-3 Adipic acid, polymer with diethylene glycol 3 9002-18-0 Agar 3 61791-56-8 beta- Alanine, N-(2-carboxyethyl)-, N-tallow alkyl derivs., disodium3 14960-06-6 beta- Alanine, N-(2-carboxyethyl)-N-dodecyl-, monosodium salt 3 Alanine, N-coco alkyl derivs. -
The Importance of Minerals in the Long Term Health of Humans Philip H
The Importance of Minerals in the Long Term Health of Humans Philip H. Merrell, PhD Technical Market Manager, Jost Chemical Co. Calcium 20 Ca 40.078 Copper 29 Cu 63.546 Iron Magnesium 26 12 Fe Mg 55.845 24.305 Manganese Zinc 25 30 Mn Zn 55.938 65.380 Table of Contents Introduction, Discussion and General Information ..................................1 Calcium ......................................................................................................3 Copper .......................................................................................................7 Iron ...........................................................................................................10 Magnesium ..............................................................................................13 Manganese ..............................................................................................16 Zinc ..........................................................................................................19 Introduction Daily intakes of several minerals are necessary for the continued basic functioning of the human body. The minerals, Calcium (Ca), Iron (Fe), Copper (Cu), Magnesium (Mg), Manganese (Mn), and Zinc (Zn) are known to be necessary for proper function and growth of the many systems in the human body and thus contribute to the overall health of the individual. There are several other trace minerals requirements. Minimum (and in some cases maximum) daily amounts for each of these minerals have been established by the Institute of -

Effect of Calcium Source and Exposure-Time on Basic Caviar Spherification Using Sodium Alginate
Available online at www.sciencedirect.com International Journal of Gastronomy and Food Science International Journal of Gastronomy and Food Science 1 (2012) 96–100 www.elsevier.com/locate/ijgfs Scientific Paper Effect of calcium source and exposure-time on basic caviar spherification using sodium alginate P. Lee, M.A. Rogersn School of Environmental and Biological Sciences, Department of Food Science, Rutgers University, The State University of New Jersey, New Brunswick, NJ 08901, USA Received 24 February 2013; accepted 12 June 2013 Available online 21 June 2013 Abstract Gelation speed is directly proportional to the concentration of calcium. Although the kinetics of gelation are altered by the source of calcium, the final alginate gel strength nor the resistance to calcium diffusion are altered. Calcium chloride reaches a gel strength plateau fastest (100 s), followed by calcium lactate (500 s) and calcium gluconoate (2000 s). Calcium chloride is the best option when the bitter taste can be masked and a fast throughput is required, while calcium gluconoate may have an advantage when the membrane thickness/hardness needs to be manipulated. & 2013 AZTI-Tecnalia. Production and hosting by Elsevier B.V. All rights reserved. Keywords: Spherification; Calcium chloride; Calcium lactate; Calcium gluconate; Sodium alginate Introduction typically contain a physical outer gel membrane with a liquid core. Spherification, an old technique in the world of modernist Alginates are an attractive ingredient because they are cuisine, was pioneered at El Bulli in 2003 and is a cornerstone derived from marine brown algae (Mabeau and Fleurence, in experimental kitchens across the world (Vega and Castells, 1993) making them non-toxic, biodegradable and naturally 2012).