A Fundamental Concept in COVID-19 Lung Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Physiology an Integrated Approach
Gas Exchange and Transport Gas Exchange in the Lungs and Tissues 18 Lower Alveolar P Decreases Oxygen Uptake O2 Diff usion Problems Cause Hypoxia Gas Solubility Aff ects Diff usion Gas Transport in the Blood Hemoglobin Binds to Oxygen Oxygen Binding Obeys the Law of Mass Action Hemoglobin Transports Most Oxygen to the Tissues P Determines Oxygen-Hb Binding O2 Oxygen Binding Is Expressed As a Percentage Several Factors Aff ect Oxygen-Hb Binding Carbon Dioxide Is Transported in Three Ways Regulation of Ventilation Neurons in the Medulla Control Breathing Carbon Dioxide, Oxygen, and pH Infl uence Ventilation Protective Refl exes Guard the Lungs Higher Brain Centers Aff ect Patterns of Ventilation The successful ascent of Everest without supplementary oxygen is one of the great sagas of the 20th century. — John B. West, Climbing with O’s , NOVA Online (www.pbs.org) Background Basics Exchange epithelia pH and buff ers Law of mass action Cerebrospinal fl uid Simple diff usion Autonomic and somatic motor neurons Structure of the brain stem Red blood cells and Giant liposomes hemoglobin of pulmonary Blood-brain barrier surfactant (40X) From Chapter 18 of Human Physiology: An Integrated Approach, Sixth Edition. Dee Unglaub Silverthorn. Copyright © 2013 by Pearson Education, Inc. All rights reserved. 633 Gas Exchange and Transport he book Into Thin Air by Jon Krakauer chronicles an ill- RUNNING PROBLEM fated trek to the top of Mt. Everest. To reach the summit of Mt. Everest, climbers must pass through the “death zone” T High Altitude located at about 8000 meters (over 26,000 ft ). Of the thousands of people who have attempted the summit, only about 2000 have been In 1981 a group of 20 physiologists, physicians, and successful, and more than 185 have died. -

Everest and Oxygen—Ruminations by a Climber Anesthesiologist by David Larson, M.D
Everest and Oxygen—Ruminations by a Climber Anesthesiologist By David Larson, M.D. Gaining Altitude and Losing Partial Pressure with Dave and Samantha Larson Dr. Dave Larson is an obstetric anesthesiologist who practices at Long Beach Memorial Medical Center, and his daughter Samantha is a freshman at Stanford University. Together they have successfully ascended the Seven Summits, the tallest peaks on each of the seven continents, a feat of mountaineering postulated in the 1980s by Richard Bass, owner of the Snowbird Ski Resort in Utah. Bass accomplished it first in 1985. Samantha Larson, who scaled Everest in May 2007 (the youngest non-Sherpa to do so) and the Carstensz Pyramid in August 2007, is at age 18 the youngest ever to have achieved this feat. Because of varying definitions of continental borders based upon geography, geology, and geopolitics, there are nine potential summits, but the Seven Summits is based upon the American and Western European model. Reinhold Messner, an Italian mountaineer known for ascending without supplemental oxygen, postulated a list of Seven Summits that replaced a mountain on the Australian mainland (Mount Kosciuszko—2,228 m) with a higher peak in Oceania on New Guinea (the Carstensz Pyramid—4,884 m). The other variation in defining summits is whether you define Mount Blanc (4,808 m) as the highest European peak, or use Mount Elbrus (5,642 m) in the Caucasus. Other summits include Mount Kilimanjaro in Kenya, Africa (5,895 m), Vinson Massif in Antarctica (4,892 m), Mount Everest in Asia (8,848 m), Mount McKinley in Alaska, North America (6,194 m), and Mount Aconcagua in Argentina, South America (6,962 m). -

DEATH ZONE FREERIDE About the Project
DEATH ZONE FREERIDE About the project We are 3 of Snow Leopards, who commit the hardest anoxic high altitude ascents and perform freeride from the tops of the highest mountains on Earth (8000+). We do professional one of a kind filming on the utmost altitude. THE TRICKIEST MOUNTAINS ON EARTH NO BOTTLED OXYGEN CHALLENGES TO HUMAN AND NATURE NO EXTERIOR SUPPORT 8000ERS FREERIDE FROM THE TOPS MOVIES ALONE WITH NATURE FREERIDE DESCENTS 5 3 SNOW LEOS Why the project is so unique? PROFESSIONAL FILMING IN THE HARDEST CONDITIONS ❖ Higher than 8000+ m ❖ Under challenging efforts ❖ Without bottled oxygen & exterior support ❖ Severe weather conditions OUTDOOR PROJECT-OF-THE-YEAR “CRYSTAL PEAK 2017” AWARD “Death zone freeride” project got the “Crystal Peak 2017” award in “Outdoor project-of-the-year” nomination. It is comparable with “Oscar” award for Russian outdoor sphere. Team ANTON VITALY CARLALBERTO PUGOVKIN LAZO CIMENTI Snow Leopard. Snow Leopard. Leader The first Italian Snow Leopard. MC in mountaineering. Manaslu of “Mountain territory” club. Specializes in a ski mountaineering. freeride 8163m. High altitude Ski-mountaineer. Participant cameraman. of more than 20 high altitude expeditions. Mountains of the project Manaslu Annapurna Nanga–Parbat Everest K2 8163m 8091m 8125m 8848m 8611m The highest mountains on Earth ❖ 8027 m Shishapangma ❖ 8167 m Dhaulagiri I ❖ 8035 m Gasherbrum II (K4) ❖ 8201 m Cho Oyu ❖ 8051 m Broad Peak (K3) ❖ 8485 m Makalu ❖ 8080 m Gasherbrum I (Hidden Peak, K5) ❖ 8516 m Lhotse ❖ 8091 m Annapurna ❖ 8586 m Kangchenjunga ❖ 8126 m Nanga–Parbat ❖ 8614 m Chogo Ri (K2) ❖ 8156 m Manaslu ❖ 8848 m Chomolungma (Everest) Mountains that we climbed on MANASLU September 2017 The first and unique freeride descent from the altitude 8000+ meters among Russian sportsmen. -

Deadly High Altitude Pulmonary Disorders: Acute Mountain Sickness
Research Article Int J Pul & Res Sci Volume 1 Issue 1 - April 2016 Copyright © All rights are reserved by Michael Obrowski DOI : 10.19080/IJOPRS.2016.01.555553 Deadly High Altitude Pulmonary Disorders: Acute Mountain Sickness (AMS); High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE): A Clinical Review Michael Obrowski1* and Stephanie Obrowski2 1Doctor of Medicine (M.D. – 2000); Assistant Professor of Anatomy; CEO, Chief Physician and Surgeon of Wilderness Physicians, European Union 2Doctor of Medicine (M.D. – 2019); Medical University of Łódź; President of Wilderness Physicians, European Union Submission: January 26, 2016; Published: April 15, 2016 *Corresponding author: Michael Obrowski, M.D., Doctor of Medicine (M.D. – 2000); Assistant Professor of Anatomy; CEO, Chief Physician and Surgeon of Wilderness Physicians, European Union, 43C Żeligowskiego Street, #45, Łódź, Poland 90-644, Email: Abstract Acute Mountain Sickness (AMS); High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE). These three disorders, withMountain relatively Sickness, unimportant also smallcalled variationsHigh Altitude seen Sickness, in some isPulmonology specifically aTextbooks, triad of different because disorders, these are inso orderserious, of increasingthey are all seriousness: potentially deadly pulmonary disorders and we will discuss these three major, deadly disorders. Each one, starting with AMS, can progress rapidly to HAPE and then HACE. The two authors of this article have over half a century of high altitude mountaineering experience. They have also alsohad anddisaster still domedicine. have, for Since the lastspring twenty is rapidly years, approaching an NGO, Non-Profit and many Medical “weekend Organization backpackers” (Wilderness will start Physicians going into www.wildernessphysicians. -

Outcomes from the 2015 Round Table on Sepsis
The official daily newsletter of the 35th ISICEM Thursday 19 March 2015 Day 3 Outcomes from the 2015 Round Table on sepsis uring the opening session on Tues- day morning, Simon Finfer (Royal North Shore Hospital of Sydney and Sydney Adventist Hospital, Sydney, Australia) was joined by Steven DOpal (Memorial Hospital of Rhode Island, RI, USA) to summarize the major outcomes of the two-day Round Table discussion “This will be a on sepsis. This was a joint conference significant part of our conducted between ISICEM and the Inter- national Sepsis Forum, with representa- research agenda in the tives from every continent highlighting the future – making sure global nature of the problem. Beginning by addressing the current that our patients are state of knowledge in the epidemiology of doing well after they sepsis, Professor Finfer noted that we know leave the hospital.” surprising little, but that obtaining this data will be crucial if any meaningful strategy is Steven Opal to be developed: “To some degree we have data from developed countries, possibly far less than you would expect or think,” he said. “But there are certainly places in, notably, Africa, where we are completely devoid of data.” The reasons for this lack of data can in part be understood by an appreciation of how patient data are currently characterized and treated, with the Global Burden of Disease Project emerging as a central player in generating evidence and guiding is surprising because we believe that sepsis kills one comes into your ICU with community-acquired global health policy. more people than prostate cancer, breast cancer, pneumonia, you treat the pneumonia; maybe they “The only reference to sepsis in these sta- and many other high profile diseases. -

Mount Everest's Death Zone
Mount Everest’s Death Zone Climate change and crowds of climbers are making the world’s tallest mountain more dangerous than ever Mara Grunbaum ast year, 73-year-old Tamae Watanabe of Japan became the oldest woman to climb Mount Everest, the world’s tallest mountain. In L 2010, 13-year-old Jordan Romero of California became the youngest to reach the top. All sorts of people of varying abilities scale the massive mountain in Asia these days. That may not be a good thing—for Everest or the climbers. Last year, more than 500 people reached the top of the Himalayan mountain, which towers 8,850 meters (29,035 feet) above sea level. Hundreds more climbed partway up. While it’s a great achievement to scale Everest, it can sometimes cause problems for the climbers and the mountain itself. Everest is changing. Warming Up Why is Everest becoming more dangerous to climb? One reason is changes in its environment. Much of the mountain is covered in huge sheets of ice called glaciers. Lately, warmer temperatures in the region have been melting these glaciers. Some places that used to be covered in ice year-round are now completely ice-free in the summer. Shrinking glaciers put climbers at risk. As glaciers melt, snow, ice, and rock are more likely to tumble down the mountain in huge avalanches. These snowslides can injure or even kill climbers. “As it gets warmer, more debris tends to fall down,” says American climbing guide Freddie Wilkinson. He’s one of a number of people who think that climbing Everest is becoming too risky. -
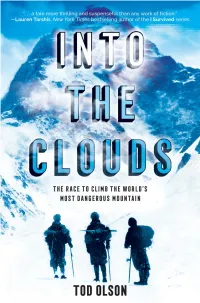
Into the Clouds
Into the Clouds ALSO BY TOD OLSON THE LOST® SERIES: Lost in the Pacific, 1942 Lost in Outer Space Lost in the Amazon Lost in the Antarctic Into the Clouds The Race to Climb the World’s Most Dangerous Mountain TOD OLSON New York Copyright © 2020 by Tod Olson All rights reserved. Published by Scholastic Focus, an imprint of Scholastic Inc., Publishers since 1920. SCHOLASTIC, SCHOLASTIC FOCUS, and associated logos are trademarks and/ or registered trademarks of Scholastic Inc. The publisher does not have any control over and does not assume any responsibility for author or third- party websites or their content. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without written permission of the publisher. For information regarding permission, write to Scholastic Inc., Attention: Permissions Department, 557 Broadway, New York, NY 10012. Library of Congress Cataloging-in-Publication Data Names: Olson, Tod, author. Title: Into the clouds : the race to climb the world’s most dangerous mountain / Tod Olson. Description: New York, NY : Scholastic Focus, 2020. | Audience: Age 10-14. Identifiers: LCCN 2019002127 (print) | LCCN 2019014682 (ebook) | ISBN 9781338207378 (E-book) | ISBN 9781338207361 (hardcover : alk. paper) Subjects: LCSH: K2 (Pakistan : Mountain)—Juvenile literature. | Mountaineering—Pakistan—K2 (Mountain)—Juvenile literature. Classification: LCC GB546.K13 (ebook) | LCC GB546.K13 O55 2020 (print) | DDC -

Human Factors in High-Altitude Mountaineering
Journal of Human Performance in Extreme Environments Volume 12 Issue 1 Article 1 Published online: 5-8-2015 Human Factors in High-Altitude Mountaineering Christopher D. Wickens Alion Science and Technology, [email protected] John W. Keller Alion Science and Technology, [email protected] Christopher Shaw Alion Science and Technology, [email protected] Follow this and additional works at: https://docs.lib.purdue.edu/jhpee Part of the Industrial and Organizational Psychology Commons Recommended Citation Wickens, Christopher D.; Keller, John W.; and Shaw, Christopher (2015) "Human Factors in High-Altitude Mountaineering," Journal of Human Performance in Extreme Environments: Vol. 12 : Iss. 1 , Article 1. DOI: 10.7771/2327-2937.1065 Available at: https://docs.lib.purdue.edu/jhpee/vol12/iss1/1 This document has been made available through Purdue e-Pubs, a service of the Purdue University Libraries. Please contact [email protected] for additional information. This is an Open Access journal. This means that it uses a funding model that does not charge readers or their institutions for access. Readers may freely read, download, copy, distribute, print, search, or link to the full texts of articles. This journal is covered under the CC BY-NC-ND license. Human Factors in High-Altitude Mountaineering Christopher D. Wickens, John W. Keller, and Christopher Shaw Alion Science and Technology Abstract We describe the human performance and cognitive challenges of high altitude mountaineering. The physical (environmental) and internal (health) stresses are first described, followed by the motivational factors that lead people to climb. The statistics of mountaineering accidents in the Himalayas and Alaska are then described. -

Safe Sojourns to High Altitudes: the Risks of Annual Religious Pilgrimages in Jammu and Kashmir, India- Clinical Diagnostics and Treatment
Research Article JOJ Pub Health Volume 2 Issue 1 - May 2017 Copyright © All rights are reserved by SM Kadri Safe Sojourns to High Altitudes: The Risks of Annual Religious Pilgrimages in Jammu and Kashmir, India- Clinical Diagnostics and Treatment SM Kadri1*, Saleem-ur-Rehman2, Michael W Popejoy3 and Christoph S Eberle4 1Division of Epidemiology and Public Health, Integrated Disease Surveillance Programme, India 2Department of Health Services, Fellow WHO Director, India 3Department of Health Promotion and Disease Prevention, Florida International University, USA 4National Academy of Clinical Biochemistry, Associate Fellow, USA Submission: May 04, 2017; Published: May 26, 2017 *Corresponding author: SM Kadri, Division of Epidemiology and Public Health, RFPTC Building, Barzulla, Srinagar 190005, Kashmir, India, Email: Abstract increasing prevalence for this type of illness. In The behavioral characteristics of high altitude climbers and the precautions necessary to This article addresses the clinical diagnosis and clinical treatment plan for several diseases that afflict high altitude climbers and the described; then, the common treatment regimens for climbermal adaptation for high altitude sickness are covered. The conclusion explored inprevent the discussion death from is thatthe high no one altitude need sportdie from activities high altitude are introduced; sickness iffirst; proper then. planning The clinical and manifestationsgood judgment ofare different applied diseaseto climbing complexes protocols; are and, that these rules are -

Clinical Review
BMJ 2011;343:d4943 doi: 10.1136/bmj.d4943 Page 1 of 10 Clinical Review CLINICAL REVIEW Acute altitude illnesses Chris Imray professor of vascular and endovascular surgery 1, Adam Booth general practioner 2, Alex Wright consultant physician 3, Arthur Bradwell professor of immunology 4 1Warwick Medical School, University Hospitals Coventry and Warwickshire NHS Trust, Coventry CV2 2DX, UK; 2Jiggins Lane Medical Centre, Birmingham, UK; 3Medical School, University of Birmingham, Birmingham; 4Immunodiagostic Research Laboratory, Medical School, University of Birmingham Acute altitude illnesses are potentially serious conditions that exceptions, most altitude related illnesses occur when there has can affect otherwise fit individuals who ascend too rapidly to been insufficient time to acclimatise at altitudes over 3000 m. altitude. They include high altitude headache, acute mountain sickness, high altitude cerebral oedema, and high altitude What are the altitude related illnesses? pulmonary oedema. The number of people travelling to altitude for work (soldiers, miners, construction workers, and The common altitude specific illnesses are high altitude astronomers) or for recreation (skiing, trekking, mountain biking, headache and acute mountain sickness. Much rarer, but more and climbing) is rising, and increased media attention towards serious, are high altitude cerebral oedema and high altitude these activities has also raised the profile of altitude related pulmonary oedema. illness. Typical scenarios in which such illness might occur are a family trek to Everest base camp in Nepal (5360 m), a fund High altitude headache raising climb of Mount Kilimanjaro (5895 m), or a tourist visit High altitude headache is defined by the International Headache to Machu Picchu (2430 m). -

Breathing at Extreme Altitudes. Scientific Projects “EVEREST” (First Part)
Review Breathing at extreme altitudes. Scientific projects “EVEREST” (First part) Breathing at extreme altitudes. Scientific projects “EVEREST” (First part) Eduardo Garrido1,2, Oriol Sibila3, Ginés Viscor2,4 1Servicio de Hipobaria y Fisiología Biomédica. Universidad de Barcelona. 2Instituto de Estudios de Medicina de Montaña. Barcelona. 3Servicio de Neumología. Hospital de la Santa Creu i Sant Pau. Barcelona. 4Departamento de Biología Celular, Fisiología e Inmunología. Universidad de Barcelona. Received: 03.03.2017 Summary Accepted: 31.05.2017 Climbing to the highest height on Earth, the Mt. Everest (8.848 m), without supplementary oxygen equipment involves a physiological demand that is close to the maximum human tolerance. Exposures at extreme altitudes drastically conditions lung function, stores of oxygen and physical performance. This review brings interesting aspects about respiration, blood gases and aerobic exercise reported by those scientific projects that have carried out physiological measurements between 8,000 m and 8,848 m above sea level, under real or simulated altitude: the Operations “Everest I” (1946), “Everest II” (1985), “Everest III-COMEX” (1997), and the Expeditions “AMREE” (1981), “British 40th Anniversary Everest” (1993), and “Caudwell Xtrem Everest” (2007). These fascinating scientific research events, along with other outstanding biomedical expeditions perfor- med above 5,500 m, like especially the “Silver Hut” (1960-61), “Italiana all’Everest” (1973), and “British Everest Medical” (1994), including those pioneer scientific reports made on the XIX century until the most recent research projects performed, have laid the foundations and knowledge on the human tolerance to such extreme levels of hypobaric hypoxia, where the lung, breathing and respiratory chain takes on a major role requiring fine physiological adjustments to ensure cellular oxygenation. -

Journal of Physics Special Topics an Undergraduate Physics Journal
Journal of Physics Special Topics An undergraduate physics journal P2 5 Jack and the Decompression Sickness K. Hinchcliffe, K. Golsby, H. Biddle, J. Mooney Department of Physics and Astronomy, University of Leicester, Leicester, LE1 7RH November 6, 2019 Abstract In this paper, we calculate the volume of supplemental oxygen that Jack would need to climb and descend the entire height of the beanstalk in the classic fairy-tale, Jack and the Beanstalk. We also find the pressure of the air at the beanstalk peak and compare this to the pressure at sea-level. These values were found to be 1880 litres and 0:365 Pa respectively. Introduction continue the 92000 m journey up. In the classic fairy-tale Jack and the We then find the time it would take Jack to Beanstalk, Jack climbs the Giant's beanstalk to climb the height of the beanstalk. By using the a land `high in the sky'. The beanstalk reached speed climbing record of 5:48 s to climb 15 m [3], to heaven in the fable, and therefore assuming we find that it would take 10:1 hours to climb the an altitude of the Karman Line, the volume of entire height of the beanstalk, and 9:33 hours to oxygen needed to climb both up and down the climb the 92000 m with supplemented oxygen. beanstalk can be found. The pressure at the As the average person breathes roughly 8 litres peak of the beanstalk can also be found and of air per minute [4], and oxygen is roughly 21% health effects at this pressure can be discussed.