Novel Mutation in an Indian Patient with Methylmalonic Acidemia, Cbla Type
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Causes and Evaluation of Mildly Elevated Liver Transaminase Levels ROBERT C
Causes and Evaluation of Mildly Elevated Liver Transaminase Levels ROBERT C. OH, LTC, MC, USA, and THOMAS R. HUSTEAD, LTC, MC, USA Tripler Army Medical Center Family Medicine Residency Program, Honolulu, Hawaii Mild elevations in levels of the liver enzymes alanine transaminase and aspartate transaminase are commonly dis- covered in asymptomatic patients in primary care. Evidence to guide the diagnostic workup is limited. If the history and physical examination do not suggest a cause, a stepwise evaluation should be initiated based on the prevalence of diseases that cause mild elevations in transaminase levels. The most common cause is nonalcoholic fatty liver disease, which can affect up to 30 percent of the population. Other common causes include alcoholic liver disease, medication- associated liver injury, viral hepatitis (hepatitis B and C), and hemochromatosis. Less common causes include α1-antitrypsin deficiency, autoimmune hepatitis, and Wilson disease. Extrahepatic conditions (e.g., thyroid disorders, celiac disease, hemolysis, muscle disorders) can also cause elevated liver transaminase levels. Initial testing should include a fasting lipid profile; measurement of glucose, serum iron, and ferritin; total iron-binding capacity; and hepa- titis B surface antigen and hepatitis C virus antibody testing. If test results are normal, a trial of lifestyle modification with observation or further testing for less common causes is appropriate. Additional testing may include ultrasonog- raphy; measurement of α1-antitrypsin and ceruloplasmin; serum protein electrophoresis; and antinuclear antibody, smooth muscle antibody, and liver/kidney microsomal antibody type 1 testing. Referral for further evaluation and possible liver biopsy is recommended if transaminase levels remain elevated for six months or more. -

Neuroleptic Malignant Syndrome: Another Medical Cause of Acute Abdomen T.C.N
Postgraduate Medical Journal (1989) 65, 653 - 655 Postgrad Med J: first published as 10.1136/pgmj.65.767.653 on 1 September 1989. Downloaded from Missed Diagnosis Neuroleptic malignant syndrome: another medical cause of acute abdomen T.C.N. Lo, M.R. Unwin and I.W. Dymock Department ofMedicine, Stepping Hill Hospital, Stockport, UK. Summary: We present a patient with neuroleptic malignant syndrome and intestinal pseudo- obstruction misdiagnosed as being secondary to septicaemia. The management of the patient is discussed with emphasis on the role of creatine kinase and liver function tests. Introduction Neuroleptic malignant syndrome (NMS) is an occas- (92% neutrophils), serum sodium 130 mmol/l, potas- ional but potentially lethal idiosyncratic complication sium 5.1 mmol/l, urea 8.8 mmol/l, creatinine 79 1tmol/ ofneuroleptic drugs.'"2 By February 1989 the Commit- 1, bilirubin 15 Amol/l, alanine transaminase 837 IU/i tee on Safety of Medicines had received reports of 99 (normal 7-45), aspartate transaminase 392 IU/l (nor- cases. (Committee on Safety of Medicines, personal mal 9-41), gamma glutamyl transferase 15 IU/I (nor- Protected by copyright. Communication). It is thought that the condition is mal <65), alkaline phosphatase 62 IU/I (normal underdiagnosed.34 We report on a case of NMS of 35-125). Serial electrocardiograms showed sinus which the presenting features and therapeutic comp- tachycardia with no acute change. Abdominal X-ray lications occurring during the course of the illness revealed marked gaseous distension ofsmall and large served to further our knowledge in this condition. bowels with multiple fluid levels seen on decubitus films. -

Liver Intracellular L-Cysteine Concentration Is Maintained After Inhibition of the Trans-Sulfuration Pathway by Propargylglycine in Rats
Downloaded from British Journal of Nutrition (1997), 78, 823-831 823 https://www.cambridge.org/core Liver intracellular L-cysteine concentration is maintained after inhibition of the trans-sulfuration pathway by propargylglycine in rats BY ANA TRIGUERO', TERESA BARBER', CONCHA GARC~A', . IP address: INMACULADA R. PUERTES', JUAN SASTRE~AND JUAN R. VIRA' 'Departamento de Bioquhica y Biologia Molecular and 2Departamento de Fisiologfa, Facultades de Farmucia y Medicina, Universidad de Valencia, 46010-Valencia, Spain 170.106.33.14 (Received 31 January 1997 - Revised 24 April I997 - Accepted 7 May 1997) , on 26 Sep 2021 at 14:28:26 To study the fate of L-cysteine and amino acid homeostasis in liver after the inhibition of the trans- sulfuration pathway, rats were treated with propargylglycine (PPG). At 4 h after the administration of PPG, liver cystathionase (EC 4.4.1.1) activity was undetectable, L-cystathionine levels were significantly higher, L-cysteine was unchanged and GSH concentration was significantly lower than values found in livers from control rats injected intraperitoneally with 0.15 M-NaCl. The hepatic levels of amino acids that are intermediates of the urea cycle, L-ornithine, L-citrulline and L-arginine and blood urea were significantly greater. Urea excretion was also higher in PPG-treated rats when , subject to the Cambridge Core terms of use, available at compared with control rats. These data suggest a stimulation of ureagenesis in PPG-treated rats. The inhibition of y-cystathionase was reflected in the blood levels of amino acids, because the L- methionine :L-cyst(e)ine ratio was significantly higher in PPG-treated rats than in control rats; blood concentration of cystathionine was also greater. -

Independent Effect of Alanine Transaminase on the Incidence Of
Clinica Chimica Acta 495 (2019) 54–59 Contents lists available at ScienceDirect Clinica Chimica Acta journal homepage: www.elsevier.com/locate/cca Independent effect of alanine transaminase on the incidence of type 2 diabetes mellitus, stratified by age and gender: A secondary analysis based T on a large cohort study in China Feng Gaoa, Xie-lin Huangb, Xue-Pei Jianga, Min Xuea, Ya-Ling Lia, Xin-Ran Lina, Yi-Han Chena, ⁎ Zhi-Ming Huanga, a Department of Gastroenterology and Hepatology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China b Department of Gastroenterology Surgery, The Second Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, China ARTICLE INFO ABSTRACT Keywords: Background: Previous studies have revealed that alanine aminotransferase (ALT) may be one of the risk factors Alanine transaminase of developing diabetes. We aimed to demonstrate the independent effect of ALT on incident diabetes and to Diabetes investigate whether the association between ALT and incident diabetes is modified by age and gender in the Age general Chinese population. Sex Methods: The present study was a retrospective cohort study, including 210,051 Chinese adult participants. The primary outcome was developing diabetes. The serum ALT activities were stratified by quintiles. We obtained data from ‘DATADRYAD’ website and used the data for secondary analysis. Results: At a median follow-up of 3.0 y, 4144 of 210,051 (1.97%) participants developed diabetes. After ad- justment for potential confounders, a significantly higher risk of the incident diabetes (HR: 1.43, 95% CI: 1.25–1.63) was found in participants in the fifth quintile (Q5, ≥31 U/L) compared to those in the first to fourth quintiles (Q1–4) for ALT activities. -

The Proteins
The Proteins The name protein is derived from Greek word Proteioes which means first because proteins essential for growth and maintenance of life. Proteins: are complex nitrogenous polymers present in all living matter, contain C,H,O and nitrogen, also contain sulfur, phosphorous, zinc, copper and iron. -- are made up of hundreds or thousands of smaller units called amino acids which are attached to one another in long chains. -- there are 20 different types of amino acids that can be combined to make a protein. -- the sequence of amino acids determines each protein’s unique 3-dimensional structure and its specific function. We need protein in diet 1. repair cells and make new ones. 2. important for growth and development in children, teens, and pregnant women. Amino acids Amino acids : are organic acids containing an amino group (NH2) and a carboxylic acid (COOH) group. The side chain can be, aliphatic, aromatic, heterocyclic, containing sulphar group . All amino acids are L-amino acids configuration. Proteins are made up of 20 amino acids in different sequences and numbers. Classification: Amino acids are classified into three groups: 1. neutral amino acids: are the largest group which are divided into: a.aliphatic amino acids ( glycine,valine,alanine,leucine,isoleucine). b. aromatic amino acids ( tyrosine, phenylalanine). c. heterocyclic amino acids ( tryptophan, histidine). d. sulpher containing amino acid ( cystine , cysteine , methionine ) 2. Acidic amino acids ( aspartic acid , glutamic acid ) 3. Basic amino acids (Lysine , arginine). Essential amino acids : Amino acids are not synthesized in the body and are essential as constituents of tissue proteins , therefore it must be supplied in food. -

Supplementary Information
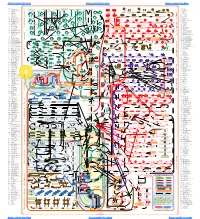
Supplementary information (a) (b) Figure S1. Resistant (a) and sensitive (b) gene scores plotted against subsystems involved in cell regulation. The small circles represent the individual hits and the large circles represent the mean of each subsystem. Each individual score signifies the mean of 12 trials – three biological and four technical. The p-value was calculated as a two-tailed t-test and significance was determined using the Benjamini-Hochberg procedure; false discovery rate was selected to be 0.1. Plots constructed using Pathway Tools, Omics Dashboard. Figure S2. Connectivity map displaying the predicted functional associations between the silver-resistant gene hits; disconnected gene hits not shown. The thicknesses of the lines indicate the degree of confidence prediction for the given interaction, based on fusion, co-occurrence, experimental and co-expression data. Figure produced using STRING (version 10.5) and a medium confidence score (approximate probability) of 0.4. Figure S3. Connectivity map displaying the predicted functional associations between the silver-sensitive gene hits; disconnected gene hits not shown. The thicknesses of the lines indicate the degree of confidence prediction for the given interaction, based on fusion, co-occurrence, experimental and co-expression data. Figure produced using STRING (version 10.5) and a medium confidence score (approximate probability) of 0.4. Figure S4. Metabolic overview of the pathways in Escherichia coli. The pathways involved in silver-resistance are coloured according to respective normalized score. Each individual score represents the mean of 12 trials – three biological and four technical. Amino acid – upward pointing triangle, carbohydrate – square, proteins – diamond, purines – vertical ellipse, cofactor – downward pointing triangle, tRNA – tee, and other – circle. -

Relationship of Liver Enzymes to Insulin Sensitivity and Intra-Abdominal Fat
Diabetes Care Publish Ahead of Print, published online July 31, 2007 Relationship of Liver Enzymes to Insulin Sensitivity and Intra-abdominal Fat Tara M Wallace MD*, Kristina M Utzschneider MD*, Jenny Tong MD*, 1Darcy B Carr MD, Sakeneh Zraika PhD, 2Daniel D Bankson MD, 3Robert H Knopp MD, Steven E Kahn MB, ChB. *Metabolism, Endocrinology and Nutrition, VA Puget Sound Health Care System 1Obstetrics and Gynecology, University of Washington, Seattle, WA 2Pathology and Laboratory Medicine, Veterans Affairs Puget Sound Health Care System, University of Washington, Seattle, WA 3Harborview Medical Center, University of Washington, Seattle, WA Running title: Liver enzymes and insulin sensitivity Correspondence to: Steven E. Kahn, M.B., Ch.B. VA Puget Sound Health Care System (151) 1660 S. Columbian Way Seattle, WA 98108 Email: [email protected] Received for publication 18 August 2006 and accepted in revised form 29 June 2007. 1 Copyright American Diabetes Association, Inc., 2007 Liver enzymes and insulin sensitivity ABSTRACT Objective: To determine the relationship between plasma liver enzyme concentrations, insulin sensitivity and intra-abdominal fat (IAF) distribution. Research Design and Methods: Plasma gamma-glutamyl transferase (GGT), aspartate transaminase (AST), alanine transaminase (ALT) levels, insulin sensitivity (SI), IAF and subcutaneous fat (SCF) areas were measured on 177 non-diabetic subjects (75M/102, 31-75 2 -5 years) with no history of liver disease. Based on BMI (< or ≥27.5 kg/m ) and SI (< or ≥7.0x10 min-1 pM-1) subjects were divided into lean insulin sensitive (LIS, n=53), lean insulin resistant (LIR, n=60) and obese insulin resistant (OIR, n=56) groups. -

Diagnostic Value of the Γ-Glutamyltransferase and Alanine
www.nature.com/scientificreports OPEN Diagnostic value of the γ‑glutamyltransferase and alanine transaminase ratio, alpha‑fetoprotein, and protein induced by vitamin K absence or antagonist II in hepatitis B virus‑related hepatocellular carcinoma Guangrong Wang1,2,3,4, Xiaolan Lu1,2,4, Qin Du1,2, Guoyuan Zhang1,2, Dongsheng Wang1,3, Qiang Wang1,2,3* & Xiaolan Guo1,2,3* Hepatocellular carcinoma is a common type of malignancy with a poor prognosis. Identifcation and utilisation of markers for monitoring and diagnosis are urgently needed. Alpha‑fetoprotein (AFP) and Protein Induced by Vitamin K Absence or Antagonist‑II (PIVKA‑II) have been proved to be efcient biomarkers for hepatitis B virus (HBV)‑related hepatocellular carcinoma (HCC). The combination of the two markers could improve the detection rate. However, these indicators cannot meet the need of clinical diagnosis.It is necessary to discover novel serological markers and more cost‑efective, appropriate combination of these markers for the diagnosis and surveillance of HBV‑related HCC. Accordingly, in this study, we aimed to evaluate the diagnostic value of γ‑glutamyltransferase (γ‑GT) to alanine amino transferase (ALT) ratio alone or in combination with AFP and PIVKA‑II for HBV‑ related HCC. 234 patients with HBV‑related HCC and 396 patients with chronic hepatitis B (CHB) were enrolled in this study and approved by the institutional review board. Our results showed levels of AFP and PIVKA‑II, and γ‑GT/ALT ratio in cases with early‑stage HCC, HCC, HCC plus HBV DNA positivity, and HCC plus HBV DNA negativity were higher than those in the corresponding CHB control group. -

Alanine Transaminase Assay (ALT) Catalog #8478 100 Tests in 96-Well Plate
Alanine Transaminase Assay (ALT) Catalog #8478 100 Tests in 96-well plate Product Description Alanine Aminotransferase (ALT), also known as serum glutamic-pyruvic transaminase (SGPT), catalyzes the reversible transfer of an amino group from alanine to α-ketoglutarate. The products of this transamination reaction are pyruvate and glutamate. ALT is found primarily in liver and serum, but occurs in other tissues as well. Significantly elevated serum ALT levels often suggest the existence of medical problems, such as hepatocellular injury, hepatitis, diabetes, bile duct problem and myopathy. This colorimetric assay is based on the oxidization of NADH to NAD in the presence of pyruvate and lactate dehydrogenase. The ALT activity is determined by assaying the rate of NADH oxidation, which is proportional to the reduction in absorbance at 340nm over time (ΔOD340nm/min). Kit Components Cat. No. # of vials Reagent Quantity Storage 8478a 1 Assay buffer 10 mL -20°C 8478b 1 ALT standard 10 µL -20°C 8478c 1 Substrate mix 1.0 mL -20°C 8478d 1 Cofactor 0.8 mL -20°C 8478e 1 Enzyme 0.2 mL -80°C Product Use The ALT kit measures the alanine transaminase activity of different types of samples, such as serum, plasma and tissues. ALT is for research use only. It is not approved for human or animal use, or for application in in vitro diagnostic procedures. Quality Control Serially diluted alanine transaminase solutions with concentrations ranging from 0.03125 to 1.0 U/mL are measured with the ScienCell™ Alanine Transaminase Assay kit. The decrease in OD340nm is monitored as a function of time (Figure 1) and the resulting standard of ∆OD340nm/min vs alanine transaminase activity are plotted (Figure 2). -

Maternal and Fetal Amino Acid Metabolism in Gestating Sows
Amino acids and swine reproduction 185 Maternal and fetal amino acid metabolism in gestating sows Guoyao Wu,1,2,3* Fuller W. Bazer,1,2 Gregory A. Johnson,2 Robert. C. Burghardt,2 Xilong Li,1 Zhaolai Dai,3 Junjun Wang3, and Zhenlong Wu3 1Department of Animal Science and 2Department of Veterinary Integrative Biosciences, Texas A&M University, College Station, Texas, USA 77843-2471; 3State Key Laboratory of Animal Nutrition, China Agricultural University, Beijing, China 100193 Among livestock species, swine exhibit the most severe naturally-occurring intra-uterine growth restriction (IUGR) primarily due to a reduction in net protein synthesis. Thus, new knowledge about fetal metabolism of amino acids (AA), which are building blocks for proteins and regulators of intracellular protein turnover, can provide a solution to this problem. Among all AA, requirements of glutamate and glutamine by fetal pigs are quantitatively the highest, but cannot be met through uterine uptake alone. Nearly all glutamate and ~70% glutamine in diets for gestating swine are degraded in the maternal small intestine and, therefore, do not enter the portal circulation. This necessitates interorgan AA metabolism involving maternal skeletal muscle, placenta, and fetal skeletal muscle to synthesize glutamate and glutamine from branched-chain AA, as well as storage of glutamate and glutamine in allantoic and amniotic fluids. The porcine placenta does not degrade arginine or glutamine, leading to their maximal transfer from maternal to fetal blood. Therefore, maternal sources of ornithine and proline play a major role in the placental synthesis of polyamines needed for placental growth including placental vascular growth. Likewise, during late gestation, uterine uptake of arginine, proline and aspartate/asparagine cannot meet requirements for optimal fetal growth. -

Enzymes of Amino Acid Metabolism in Normal Human Skin
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector THE JOURNAL OF INVESTIGATIVE DERMATOLOGY vol. 45, No. 3 Copyright 1557 by The Williams & Wilkins Co. Printed in U.S.A. ENZYMES OF AMINO ACID METABOLISM IN NORMAL HUMAN SKIN II. ALANINE AND ASPARTATE TRANSAMINASES* KENJI ADACHI, Mill., Pu.D., CHARLES LEWIS, Ja., B.S.t AND FALLS B. HERSHEY, M.D. In the preceding paper(1) we described the MATERIALS AND METHODS partial characterizationandquantitative Alanine (or aspartate) transaminase activity bistoehemieal localizationof glutamate dehy-was assayed according to the steps shown in drogenase in normal human skin. In compari-Equation 1, with L-alanine (or L-aspartate) and son with glutamate dehydrogenase, which cat-a-ketoglutarate as substrates. Alanine (or aspar- tate) transaminase catalyzes the formation of alyzes reversible oxidative deamination, thepyruvate (or oxaloacetate) and L-glutamate. The transaminases catalyze transferof aminoresulting pyruvate (or oxaloacetate) is imme- groups, usually from an amino acid to a keto-diately converted to lactate (or malate) in the acid, without net loss of nitrogen. In otherpresence of NADH' and purified lactate (or malate) dehydrogenase. The NAD' produced was words, transamination represents the inter-measured fluorometrically (1,2). molecular exchange of amino nitrogen. Trans- The complete alanine transaminase substrate amination plays a significant role in metab-reagent consisted of 2.5 mM a-ketoglutarate, 100 olism by providing numerous alternativemM L-alanine (adjusted to pH 7.9), 1 mg% pyridoxal phosphate, 0.5% bovine plasma albumin, pathways between amino acids. Obviously, it20 mM nicotinamide, 1 mM NADH, and 5 g/ml is a useful process for tissues, by which ex-reagent mixture of crysta]line lactate dehydro- cessive amounts of certain amino acids cangenase in 100 mM Tris-HC1 buffer at pH 7.9. -
O O2 Enzymes Available from Sigma Enzymes Available from Sigma
COO 2.7.1.15 Ribokinase OXIDOREDUCTASES CONH2 COO 2.7.1.16 Ribulokinase 1.1.1.1 Alcohol dehydrogenase BLOOD GROUP + O O + O O 1.1.1.3 Homoserine dehydrogenase HYALURONIC ACID DERMATAN ALGINATES O-ANTIGENS STARCH GLYCOGEN CH COO N COO 2.7.1.17 Xylulokinase P GLYCOPROTEINS SUBSTANCES 2 OH N + COO 1.1.1.8 Glycerol-3-phosphate dehydrogenase Ribose -O - P - O - P - O- Adenosine(P) Ribose - O - P - O - P - O -Adenosine NICOTINATE 2.7.1.19 Phosphoribulokinase GANGLIOSIDES PEPTIDO- CH OH CH OH N 1 + COO 1.1.1.9 D-Xylulose reductase 2 2 NH .2.1 2.7.1.24 Dephospho-CoA kinase O CHITIN CHONDROITIN PECTIN INULIN CELLULOSE O O NH O O O O Ribose- P 2.4 N N RP 1.1.1.10 l-Xylulose reductase MUCINS GLYCAN 6.3.5.1 2.7.7.18 2.7.1.25 Adenylylsulfate kinase CH2OH HO Indoleacetate Indoxyl + 1.1.1.14 l-Iditol dehydrogenase L O O O Desamino-NAD Nicotinate- Quinolinate- A 2.7.1.28 Triokinase O O 1.1.1.132 HO (Auxin) NAD(P) 6.3.1.5 2.4.2.19 1.1.1.19 Glucuronate reductase CHOH - 2.4.1.68 CH3 OH OH OH nucleotide 2.7.1.30 Glycerol kinase Y - COO nucleotide 2.7.1.31 Glycerate kinase 1.1.1.21 Aldehyde reductase AcNH CHOH COO 6.3.2.7-10 2.4.1.69 O 1.2.3.7 2.4.2.19 R OPPT OH OH + 1.1.1.22 UDPglucose dehydrogenase 2.4.99.7 HO O OPPU HO 2.7.1.32 Choline kinase S CH2OH 6.3.2.13 OH OPPU CH HO CH2CH(NH3)COO HO CH CH NH HO CH2CH2NHCOCH3 CH O CH CH NHCOCH COO 1.1.1.23 Histidinol dehydrogenase OPC 2.4.1.17 3 2.4.1.29 CH CHO 2 2 2 3 2 2 3 O 2.7.1.33 Pantothenate kinase CH3CH NHAC OH OH OH LACTOSE 2 COO 1.1.1.25 Shikimate dehydrogenase A HO HO OPPG CH OH 2.7.1.34 Pantetheine kinase UDP- TDP-Rhamnose 2 NH NH NH NH N M 2.7.1.36 Mevalonate kinase 1.1.1.27 Lactate dehydrogenase HO COO- GDP- 2.4.1.21 O NH NH 4.1.1.28 2.3.1.5 2.1.1.4 1.1.1.29 Glycerate dehydrogenase C UDP-N-Ac-Muramate Iduronate OH 2.4.1.1 2.4.1.11 HO 5-Hydroxy- 5-Hydroxytryptamine N-Acetyl-serotonin N-Acetyl-5-O-methyl-serotonin Quinolinate 2.7.1.39 Homoserine kinase Mannuronate CH3 etc.