Defensive Medicine in Cases of Poor Prenatal Diagnoses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
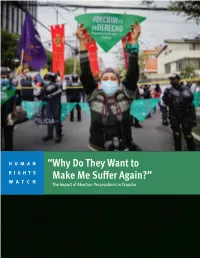
“Why Do They Want to Make Me Suffer Again?” the Impact of Abortion Prosecutions in Ecuador
HUMAN “Why Do They Want to RIGHTS WATCH Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Copyright © 2021 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 978-1-62313-919-3 Cover design by Rafael Jimenez Human Rights Watch defends the rights of people worldwide. We scrupulously investigate abuses, expose the facts widely, and pressure those with power to respect rights and secure justice. Human Rights Watch is an independent, international organization that works as part of a vibrant movement to uphold human dignity and advance the cause of human rights for all. Human Rights Watch is an international organization with staff in more than 40 countries, and offices in Amsterdam, Beirut, Berlin, Brussels, Chicago, Geneva, Goma, Johannesburg, London, Los Angeles, Moscow, Nairobi, New York, Paris, San Francisco, Sydney, Tokyo, Toronto, Tunis, Washington DC, and Zurich. For more information, please visit our website: http://www.hrw.org JULY 2021 ISBN: 978-1-62313-919-3 “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Summary ........................................................................................................................... 1 Key Recommendations ....................................................................................................... 8 To the Presidency ................................................................................................................... -
Contraception and Abortion: a Utilitarian View
Contraception and Abortion: A Utilitarian View Leslie Allan Published online: 13 September 2015 Copyright © 2015 Leslie Allan Conservative and liberal approaches to the problem of abortion are oversimplified and deeply flawed. Accepting that the moral status of the conceptus changes during gestation, the author advances a more sophisticated and nuanced perspective on contraception and abortion policy. He also critically questions the moral relevance of the conceptus’ membership of the human species and reviews other crucial meta-ethical presuppositions to bolster his case. Through applying a form of rules in practice utilitarianism within the context of overall population policy, he provides a compelling ethical and legal framework for regulating contraception and abortion practices. To cite this essay: Allan, Leslie 2015. Contraception and Abortion: A Utilitarian View, URL = <http://www.RationalRealm.com/philosophy/ethics/contraception-abortion-utilitarian-view.html> To link to this essay: www.RationalRealm.com/philosophy/ethics/contraception-abortion-utilitarian-view.html Follow this and additional essays at: www.RationalRealm.com This article may be used for research, teaching, and private study purposes. Any substantial or systematic reproduction, redistribution, reselling, loan, sublicensing, systematic supply, or distribution in any form to anyone is expressly forbidden. Terms and conditions of access and use can be found at www.RationalRealm.com/policies/tos.html Leslie Allan Contraception and Abortion: A Utilitarian View 1. Introduction -

Pecuniary Reparations Following National Crisis: a Convergence of Tort Theory, Microfinance, and Gender Equality
Brooklyn Law School BrooklynWorks Faculty Scholarship Fall 2009 Pecuniary Reparations Following National Crisis: A convergence of Tort Theory, Microfinance, and Gender Equality Anita Bernstein Brooklyn Law School, [email protected] Follow this and additional works at: https://brooklynworks.brooklaw.edu/faculty Part of the Law and Gender Commons, Legislation Commons, Other Law Commons, and the Torts Commons Recommended Citation 31 U. Pa. J. Int'l L. 1 (2009-2010) This Article is brought to you for free and open access by BrooklynWorks. It has been accepted for inclusion in Faculty Scholarship by an authorized administrator of BrooklynWorks. ARTICLES PECUNIARY REPARATIONS FOLLOWING NATIONAL CRISIS: A CONVERGENCE OF TORT THEORY, MICROFINANCE, AND GENDER EQUALITY ANITA BERNSTEIN* 1. INTRODUCTION Numerous possible contexts can impel national governments to start reparations programs. From the array of possibilities, this Article focuses on reparations for the effects of a crisis that ravaged a whole nation-for example civil war, genocide, dictatorship, or apartheid -rather than on one discrete, odious deviation from the norms of a functioning democracy. Isolated incidents can generate urgent needs for repair, but the reparations under discussion in this Article presume a more fundamental ambition: a declaration of the nation's past as broken, and its future in need of mending.1 The government of a nation, acknowledging grave strife in its * Anita and Stuart Subotnick Professor of Law, Brooklyn Law School. My thanks to the New York Tort Theory Reading Group and the faculties of Emory, Washington University, and the Australian National University law schools for valuable comments on an earlier version of this Article. -

Abortion and Human Rights in Central America
Janus Head: Volume 17 Issue 1 9 Abortion and Human Rights in Central America Gabriela Arguedas-Ramírez Translated from Spanish to English by Gabriela Argueda-Ramírez and Allison B. Wolf Abstract This essay aims to show that the nations of Central America must create access to safe and legal abortion as well as promote a political dialogue on the subject that is based on reason and science, rather than religion. Not only does prohibiting abortion constitute a violation of women's human rights, but, based on international human rights law as well as the minimum duties of civil ethics, failing in to provide such access or dialogue would mean failing to meet the standards of a legitimate democratic state. Keywords: Abortion, Human Rights, Women, Democracy, Ethics, Central America Copyright © 2019 by Trivium Publications, Pittsburgh, PA All rights reserved. Janus Head: Volume 17 Issue 1 10 Introduction Complete bans of abortion constitute human rights violations, specifically of the human rights of pregnant women. In fact, there are no robust arguments from either the legal or ethical perspective to justify such bans. This is not simply my opinion. The doctrine and jurisprudence of the Inter-American Court of Human Rights, the European and the African human rights systems, and the human rights system of the United Nations, all maintain that the absolute criminalization of abortion is an irrational excess that lacks a basis within the international law of human rights. And, reports from the Convention for the Elimination of All Forms of Discrimination against Women (CEDAW) 1 and the United Nations Human Rights Commission,2 all argue that the absolute criminalization of abortion constitutes an arbitrary obstruction of the fundamental rights of women. -

A Remedy for Abortion Seekers Under the Invasion of Privacy Tort Rachel L
Brooklyn Law Review Volume 68 | Issue 1 Article 6 9-1-2002 A Remedy for Abortion Seekers Under the Invasion of Privacy Tort Rachel L. Braunstein Follow this and additional works at: https://brooklynworks.brooklaw.edu/blr Recommended Citation Rachel L. Braunstein, A Remedy for Abortion Seekers Under the Invasion of Privacy Tort, 68 Brook. L. Rev. 309 (2002). Available at: https://brooklynworks.brooklaw.edu/blr/vol68/iss1/6 This Note is brought to you for free and open access by the Law Journals at BrooklynWorks. It has been accepted for inclusion in Brooklyn Law Review by an authorized editor of BrooklynWorks. NOTES A REMEDY FOR ABORTION SEEKERS UNDER THE INVASION OF PRIVACY TORT* INTRODUCTION The United States Supreme Court articulated the right to an abortion as a fundamental constitutional privacy right in Roe v. Wade.' The Court stated, "[t]his right of privacy, whether it be found in the Fourteenth Amendment's concept of personal liberty and restrictions upon state action.., or... in the Ninth Amendment's reservation of rights to the people, is broad enough to encompass a woman's decision whether or not to terminate her pregnancy."2 The Court thus defined the constitutional privacy right encompassing abortion as a woman's right to be free from governmental interference in reproductive choice. In exercising this right, some abortion clinic clients, or "abortion seekers," have been photographed by anti-abortion protestors in the vicinity of clinics. Anti-abortion protestors have posted some of those photographs on the Internet. One such protestor, Neal Horsley, maintains a website on which he3 posts the names of abortion providers and clinic workers. -

On the Brink of Death Violence Against Women and the Abortion Ban in El Salvador
ON THE BRINK OF DEATH VIOLENCE AGAINST WOMEN AND THE ABORTION BAN IN EL SALVADOR MY BODY MY RIGHTS CAMPAIGN Amnesty International is a global movement of more than 3 million supporters, members and activists in more than 150 countries and territories who campaign to end grave abuses of human rights. Our vision is for every person to enjoy all the rights enshrined in the Universal Declaration of Human Rights and other international human rights standards. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and public donations. First published in 2014 by Amnesty International Ltd Peter Benenson House 1 Easton Street London WC1X 0DW United Kingdom © Amnesty International 2014 Index: AMR 29/003/2014 Original language: English Printed by Amnesty International, International Secretariat, United Kingdom All rights reserved. This publication is copyright, but may be reproduced by any method without fee for advocacy, campaigning and teaching purposes, but not for resale. The copyright holders request that all such use be registered with them for impact assessment purposes. For copying in any other circumstances, or for reuse in other publications, or for translation or adaptation, prior written permission must be obtained from the publishers, and a fee may be payable. To request permission, or for any other inquiries, please contact [email protected] Cover photo: Mural at women’s centre in Suchitoto, El Salvador, 2014. © Amnesty International amnesty.org CONTENTS -

In the Supreme Court of the United States
No. 18-483 In The Supreme Court of the United States KRISTINA BOX, COMMISSIONER OF THE INDIANA STATE DEPARTMENT OF HEALTH, ET AL., Petitioners, v. PLANNED PARENTHOOD OF INDIANA AND KENTUCKY, INC, ET AL., Respondents. On Petition for Writ of Certiorari to the United States Court of Appeals for the Seventh Circuit AMICUS BRIEF OF THE AMERICAN CENTER FOR LAW AND JUSTICE AND PARENTS OF DISABLED CHILDREN IN SUPPORT OF PETITIONERS JAY ALAN SEKULOW Counsel of Record STUART J. ROTH COLBY M. MAY WALTER M. WEBER OLIVIA SUMMERS AMERICAN CENTER FOR LAW & JUSTICE 201 Maryland Ave., N.E. Washington, DC 20002 (202) 546-8890 [email protected] Counsel for Amici Curiae i TABLE OF CONTENTS TABLE OF AUTHORITIES.................. ii INTEREST OF AMICUS .................... 1 SUMMARY OF ARGUMENT................. 2 ARGUMENT.............................. 2 I. STATES CAN TREAT HUMAN REMAINS AS HUMAN REMAINS. .................... 3 II. STATES HAVE A STRONG INTEREST IN COMBATING THE POTENTIALLY LETHAL PESSIMISM OF SOME PRENATAL FORECASTS. .......................... 7 CONCLUSION ........................... 11 APPENDIX: List of individual amici parents . 1a ii TABLE OF AUTHORITIES Cases Page Alexander v. Whitman, 114 F.3d 1392 (3d Cir. 1997) ........................... 4 Bolin v. Wingert, 764 N.E.2d 201 (Ind. 2001) .... 5 Burwell v. Hobby Lobby, 134 S. Ct. 2751 (2014) . 4 City of Akron v. Akron Center for Reproductive Health, 462 U.S. 416 (1983) ..... 3 Franklin v. Fitzpatrick, 428 U.S. 901 (1976) ..... 3 Hickman v. Group Health Plan, Inc., 396 N.W.2d 10 (Minn. 1986) ................ 6 Maher v. Roe, 432 U.S. 464 (1977) ............. 5 Monell v. Dep’t of Social Servs., 436 U.S. -

Towards a Practical Implementation of the Abortion Decision: the Interests of the Physician, the Woman and the Fetus
DePaul Law Review Volume 25 Issue 3 Spring 1976 Article 6 Towards a Practical Implementation of the Abortion Decision: The Interests of the Physician, the Woman and the Fetus Mary Sebek Follow this and additional works at: https://via.library.depaul.edu/law-review Recommended Citation Mary Sebek, Towards a Practical Implementation of the Abortion Decision: The Interests of the Physician, the Woman and the Fetus, 25 DePaul L. Rev. 676 (1976) Available at: https://via.library.depaul.edu/law-review/vol25/iss3/6 This Comments is brought to you for free and open access by the College of Law at Via Sapientiae. It has been accepted for inclusion in DePaul Law Review by an authorized editor of Via Sapientiae. For more information, please contact [email protected]. COMMENTS TOWARDS A PRACTICAL IMPLEMENTATION OF THE ABORTION DECISION: THE INTERESTS OF THE PHYSICIAN, THE WOMAN AND THE FETUS The United States Supreme Court has considered the issue of a woman's right to an abortion, I and has resolved that such a right, guar- anteed under the concept of individual privacy,2 does exist. The Court did not, however, discuss the ramifications of an abortion resulting in a live birth, nor did the Court resolve the question of when life actually begins.3 Instead, the Court couched its decision in terms relating only to the fetus,4 stating that the fetus is not a person within the contempla- tion of the law.' Many have disagreed with this conclusion, asserting that traditional Anglo-American law has always recognized the fetus as a person.' However, a careful analysis of property, tort, wrongful death, social welfare and criminal law indicates that the fetus has never been accorded the rights and privileges of persons. -

Nysba Winter 2006 | Vol
NYSBA WINTER 2006 | VOL. 11 | NO. 1 Health Law Journal A publication of the Health Law Section of the New York State Bar Association SPECIAL EDITION: SELECTED TOPICS IN LONG-TERM CARE LAW Special Edition Editor: Cornelius D. Murray Inside A Message from the Section Chair 5 The Olmstead Imperative: Judicial Interpretation of ADA and Lynn Stansel Federal-State Response 46 Regular Features Raul A. Tabora, Jr. In the New York State Courts 6 A Social Ecology of Health Model in End-of-Life Decision-Making: In the New York State Legislature 13 Is the Law Therapeutic? 51 In the New York State Agencies 15 Mary Beth Morrissey, JD, MPH and Bruce Jennings, MA In the Journals 17 For Your Information 19 Article 81 Guardianship Obstacles for Petitioning Providers: Who Should Be Proposed As Guardian? Who Should Testify? 61 Feature Articles Alyssa M. Barreiro Public Health Law § 2801-d and the Nursing Home Crisis: The Propriety of Invoking the Statute in Routine Negligence Cases 20 Appellate Division Solidifies Legal Protection for Receivers—Recent Andrew L. Zwerling Decision: Niagara Mohawk Power Corporation v. Anthony Salerno 65 Jerauld E. Brydges and John M. Jennings The Use of Pre-Dispute Arbitration Clauses in New York Nursing Home Agreements 26 Editor’s Selected Court Decision Jane Bello Burke Blossom View Home v. Novello 68 The Assisted Living Reform Act of 2004: New Models of Care, State Government Reports New Choices for Consumers 31 Dietary Supplements: Balancing Consumer Choice Alan J. Lawitz and Safety (Executive Summary) 74 Certificate of Need and Long-Term Care—Changes are Coming 41 The New York State Task Force on Life and the Law Jerome Levy Section Matters Newsflash: What’s Happening in the Section 78 HEALTH LAW JOURNAL WINTER 2006 Vol. -

What to Do When a Doctor Recommends Abortion Well-Known and Respected California Pastor Took a He Healed Our Baby of Every Abnormality
Directors CENTER FOR BIO-ETHICAL REFORM MARCH 2011 Gregg & Lois Cunningham What to Do When a Doctor Recommends Abortion well-known and respected California pastor took a He healed our baby of every abnormality. The hole in the heart call on his call-in radio show in early February. The is so small that the doctor could hardly detect it. All the other female caller tearfully told him she was carrying problems cleared up. The only thing that didn’t look right were Aconjoined twins and her doctor recommended the kidneys. If God began this good work, he will finish it. abortion. She asked the pastor what she should do. Shockingly, Throughout this whole pregnancy, from the very beginning, the he said, “It’s awfully hard to actually suggest abortion, but I’m doctors wanted to abort him.” sure that in a case like this where the life expectancy is so bleak, I’m sure that the Lord would not condemn her if she had an Together we must work to spare pregnant women from medical scenarios that end in abortion tragedies. I will never forget abortion.” my dismay when we made a follow-up call to a client at the It is obvious that pastors must be better informed! You can Pregnancy Help Clinic of Glendale. The counselor did not help by sharing this newsletter with your pastor; hand him a believe the client was at risk for abortion when she left our copy or email the link from our website. In hard cases, pastors clinic, so she was just checking on her progress. -

Malpractice Claims Resulting from Negligent Preconception Genetic
MAHONEY_NOTE_FINAL.DOC 4/15/2006 11:35 AM Malpractice Claims Resulting from Negligent Preconception Genetic Testing: Do These Claims Present a Strain of Wrongful Birth or Wrongful Conception, and Does the Categorization Even Matter? Imagine that parents of a child, who bears a genetic abnormality, attempt to discern the risks in conceiving another child. Because they are concerned about the possibility of conceiving a second child with a similar defect, the parents consult a doctor for genetic testing. The doctor carelessly neglects to facilitate critical genetic tests, yet ensures the parents that the risks of an abnormality in a second child are low. Based on these optimistic test results, the parents choose to have another child. Despite the doctor’s assurances, the second child is born with the same genetic defect as the first child. The parents elect to sue the doctor for the erroneous medical consultation. Which prenatal cause of action should these parents bring for a claim based on negligent preconception genetic testing? “Confusion . arises as to the proper denomination of these prenatal torts. Because this area of the law is new and fraught with emotion, both courts and commentators have often blurred . distinctions among the actions. Believing those distinctions are vitally important to both theory and outcome, we commence . .”1 I. INTRODUCTION Medical advancements currently allow parents to undergo preconception or neonatal genetic testing to determine the likelihood of a childhood defect.2 The advent of genetic testing has compelled courts to develop novel causes of action based on traditional negligence principles to address these medical malpractice claims.3 Typically, courts recognizing such parental malpractice 1. -

The Debate Over Reproductive Rights in Germany and Slovakia
www.ssoar.info The Debate over Reproductive Rights in Germany and Slovakia: Religious and Secular Voices, a Blurred Political Spectrum and Many Inconsistencies Petrjánošová, Magda; Moulin-Doos, Claire; Plichtová, Jana Veröffentlichungsversion / Published Version Zeitschriftenartikel / journal article Empfohlene Zitierung / Suggested Citation: Petrjánošová, M., Moulin-Doos, . C., & Plichtová, J. (2008). The Debate over Reproductive Rights in Germany and Slovakia: Religious and Secular Voices, a Blurred Political Spectrum and Many Inconsistencies. Politics in Central Europe, 4(2), 61-78. https://nbn-resolving.org/urn:nbn:de:0168-ssoar-63207 Nutzungsbedingungen: Terms of use: Dieser Text wird unter einer Deposit-Lizenz (Keine This document is made available under Deposit Licence (No Weiterverbreitung - keine Bearbeitung) zur Verfügung gestellt. Redistribution - no modifications). We grant a non-exclusive, non- Gewährt wird ein nicht exklusives, nicht übertragbares, transferable, individual and limited right to using this document. persönliches und beschränktes Recht auf Nutzung dieses This document is solely intended for your personal, non- Dokuments. Dieses Dokument ist ausschließlich für commercial use. All of the copies of this documents must retain den persönlichen, nicht-kommerziellen Gebrauch bestimmt. all copyright information and other information regarding legal Auf sämtlichen Kopien dieses Dokuments müssen alle protection. You are not allowed to alter this document in any Urheberrechtshinweise und sonstigen Hinweise auf gesetzlichen way, to copy it for public or commercial purposes, to exhibit the Schutz beibehalten werden. Sie dürfen dieses Dokument document in public, to perform, distribute or otherwise use the nicht in irgendeiner Weise abändern, noch dürfen Sie document in public. dieses Dokument für öffentliche oder kommerzielle Zwecke By using this particular document, you accept the above-stated vervielfältigen, öffentlich ausstellen, aufführen, vertreiben oder conditions of use.