How the Nations Should Gear up for Future Pandemics?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pandemic Planning , File Type: PDF, File Size
July 2021 Dear ATISN 15194 – Pandemic Planning Thank you for your request to the Welsh Government for information under the Freedom of Information Act (2000) received on 03 June 2021. I have interpreted your requested information regarding pandemic planning as follows: 1. What plans were in place for a potential future pandemic before the COVID19 crisis began? 2. What conversations were had at ministerial level, before COVID19, about the potential of a future pandemic? 3. What plans are now in place for a future pandemic, if any? Our Response What plans were in place for a potential future pandemic before the COVID-19 crisis began? Wales, together with the rest of the UK, has been preparing its response to an influenza pandemic for many years. In 2007, Wales participated in the UK level (Tier 1) pandemic flu exercise Winter Willow, which led to the development of the 2007 National Framework for Responding to an Influenza Pandemic. This framework was used to support our Welsh Government response to the 2009 H1N1 Swine Flu pandemic. Although the H1N1 pandemic was not as severe as initially predicted, it did identify areas for further planning and Wales worked with the other UK governments to put in place the UK Influenza Preparedness Strategy 2011. This UK Strategy was agreed by the Health Ministers of all four nations. In 2016, our pandemic influenza plans were tested during Exercise Cygnus. The subsequent lessons identified were taken forward into an ongoing review of pandemic preparedness led by the UK Cabinet Office and Department of Health and Social Care. -

27Th APRIL 2020
27th APRIL 2020 19 COVID-19 REPORT SUMMARY • The number of confirmed deaths as a result of COVID-19 has now passed 200,000 with Johns Hopkins University confirming almost 2,980,053 cases worldwide. • On 25th April, the UK became the fifth country in the world to record 20,000 hospital deaths as a result of COVID- 19. The UK death toll currently stands at 20,732. • Several Muslim majority countries have now begun to soften COVID-19 measures in preparation for the holy month of Ramadan with Saudi Arabia, Egypt and Algeria all shortening curfews that had been in place. • Multiple US States and European countries have begun to ease lockdown restrictions having instituted plans to begin reopening shops. • The World Health Organisation has warned that Africa could see as many as 10 million cases of COVID-19 within three to six months. In the last 10 days alone, the continent has seen a 40% rise in new COVID-19 cases. • A second wave of locusts has descended on East Africa and the swarm is estimated to be 20 times bigger than the first invasion at the end of 2019. Amidst the COVID-19 global lockdown, pesticides and bio-pesticides usually sourced from countries such as Japan, Morocco and the Netherlands, have become more expensive and harder to obtain. Further to this, protective clothing worn when using pesticides have been taken for those combating this coronavirus outbreak. • The World Health Organisation has warned against introducing ‘immunity passports’ for people who have recovered from the COVID-19 virus, citing that ‘there is currently no evidence that people who have recovered from Covid-19 and have antibodies are protected from a second infection’. -

COVID-19/SARS-Cov2: an Exploration
COVID-19/SARS-CoV2: An Exploration How we act now INTERACTIVE DOWNLOADABLE PDF will build the future for our children An urgent invitation: • To question all that is happening before the chance is lost • To explore broader science, views and statistics • To research further A compilation of links to resources that will: • Help you to navigate the current situation • Help you to make informed decisions • Promote open debate and explore different views • Offer a starting point for further research • Introduce just the tip of the iceberg of the wealth of knowledge we can explore Photo by Monica Gozalo on Unsplash.com • June 2021 COVID-19/SARS-CoV2: An Exploration PLEASE NOTE: Any text you see coloured orange with an underline throughout this document, will be clickable live links to internal Sections or Pages within this document, or go to external reference websites. INTRODUCTION In response to the remarkable times we are living in, we have created this shareable, downloadable, interactive PDF Exploration document ( also found on-lineHERE ), a gathering of our extensive research into the covid pandemic and its effects on us all. We hope that it will enable and inspire you to research further if you choose to. We respect and appreciate that some of what you read and explore may challenge views you hold to be true at the moment, but we believe there are significant questions that need asking about the Covid19 narrative as it is. We all wish to make choices that will enable a full and healthy life for ourselves, our communities and our children, and that are right for now and for the future. -
Wetherspoon-News-Do-Lockdowns-Work-Winter-2020.Pdf
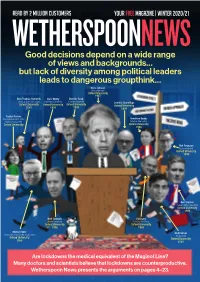
READ BY 2 MILLION CUSTOMERS your free magazine | winter 2020/21 WETHERSPOONNEWS Good decisions depend on a wide range of views and backgrounds… but lack of diversity among political leaders leads to dangerous groupthink… Boris Johnson (Prime Minister) Oxford University 1987 Nick Thomas-Symonds Chris Whitty Dominic Raab (Shadow Home Secretary) (Chief Medical Officer) (Foreign Secretary) Dominic Cummings Oxford University Oxford University Oxford University Oxford University 2001 1991 1993 1994 Rachel Reeves (Shadow Chancellor of the Anneliese Dodds Duchy of Lancaster) (Shadow Chancellor) Oxford University Oxford University 1998 Neil Ferguson (epidemiologist) Oxford University 1990 Keir Starmer (Leader of the Opposition) Oxford University 1986 Matt Hancock Ed Davey (Health Secretary) (Leader, Lib Dems) Oxford University Oxford University 1996 1988 Michael Gove Rishi Sunak (Chancellor of the Duchy of Lancaster) (Chancellor) Oxford University Oxford University 1988 2001 Are lockdowns the medical equivalent of the Maginot Line? Many doctors and scientists believe that lockdowns are counterproductive. Wetherspoon News presents the arguments on pages 4–23. Tim’s Viewpoint Weak leaders follow the crowd – only the brave will stand alone Politicians have become disciples of failed forecasters – and continue to promote lockdowns Johan Giesecke, the ‘Great Recession’ of 2008– country’s highest-paid economy and to mental Swedish epidemiologist, 10 is a fairly recent example. journalist as a young man, and physical health. said in April (interview No sector of the economy then a renowned historian – In addition, as former on page 14) that it was comprises more top-class and, against the odds, rallied Supreme Court judge “fascinating” how deeply university graduates than the country in its darkest hour Jonathan Sumption flawed Imperial College the banks, brokers and fund to battle for survival. -

Of the Royal College of Pathologists
The Bulletin of the Royal College of Pathologists Number 191 July 2020 SPECIAL EDITION: Pathology and COVID-19 The role of genomics in shaping the response Cytology and the pandemic Experiences of NHS Nightingale Death certification Establishing convalescent plasma therapy Caring for the deceased Testing in the devolved nations Our COVID-19 seminars Also in this issue: The Royal College of Pathologists Haematology workforce challenges Pathology: the science behind the cure Going digital: training and exams Kate Gould: an appreciation The Royal College of Pathologists CONTENTS Pathology: the science behind the cure July 2020 NuMBER 191 EDITORIALS 114 INTERNATIONAL 150 From the Editor 114 Challenges for pathology laboratories during From the President 115 the pandemic: the view from Australia 150 PATHOLOGY AND COVID-19 117 Reorganisation of mobile blood collections in the age of social distancing 152 A new plague year 117 The role of viral genomics in shaping the TRAINING 154 response to the pandemic 118 FRCPath examinations during the COVID Nightingale tales 121 pandemic 154 The journey from Oxford medical school to Digital pathology and safe workplace the world’s largest ICU 124 station awareness 157 Cytology and the pandemic 125 Creating e-learning modules for undergraduate Establishing convalescent plasma as an medical students 159 effective therapy 126 Digital pathology validation for trainees: 160 Healthcare scientists in pathology: the CLINICAL EFFECTIVENESS 162 challenges of responding to the virus 128 What does patient safety in -
PDF, File Size
ATISN 14601 16 December 2020 Dear ATISN 14601 – Covid-19 Thank you for your request to the Welsh Government for information under the Freedom of Information Act (2000) received on 29 November. You asked for: 1. Why are SARS-CoV-2 antibody levels flat or dropping across all age groups since May if the pandemic is still going? The Welsh Government does not hold information that shows levels of antibodies are flat or dropping across all age groups since May. The latest information the Welsh Government holds on levels of antibodies in the population is published here: https://gov.wales/coronavirus-covid-19-infection-survey This information is taken from the Coronavirus (COVID-19) Infection Survey (CIS) which is run across the whole of the UK and aims to estimate: how many people have the infection over a given time (positivity); how many new cases occur over a given period (incidence); and how many people have antibodies to COVID-19. This shows that antibody rates in those tested appear to have increased since the summer. 2. What percentage of the population is assumed to have had prior immunity to SARS-CoV-2 in the SAGE forecasting models? The Welsh Government does not hold information on the assumptions made in the SAGE forecasting models with regard to the percentage of the population and prior immunity. Information on how to make an FOI request to the Scientific Advisory Group for Emergencies can be found here: https://www.gov.uk/government/organisations/scientific-advisory-group-for-emergencies 3. Why do 50% of household members not catch SARS-CoV-2 from infected persons with whom they live? Parc Cathays ● Cathays Park Caerdydd ● Cardiff CF10 3NQ The Welsh Government does not hold recorded information on the percentage of household members that catch the virus from infected persons with whom they live. -

Data Flows of COVID-19
The data flows of COVID-19 Drawing on published documents, media reports and various individual and crowdsourced efforts listed in ‘Other references’ below, what do we know about the (health and social care) data flows of COVID-19? We all know there’s far more than just dodgy PPE contracts, Serco, Faculty AI and Palantir to be concerned about – but few seem to appreciate the full extent and very few the detail of what has been going on. N.B. This document covers what has been going on with health data in England in 2020, with occasional references to what has been happening in the other nations. Legal basis Firstly, in terms of the lawfulness of data flows, what changed? Much of what has been done with data during the pandemic has been enabled by the COPI Notices, first issued in March 2020, extended in July 2020, and extended again in February 2021. At the time of writing, the COPI Notices will expire on 30 September 2021. What is perhaps less well known is that on 30 January 2020, a “Level 4 National Incident” was declared by NHS England. This was six weeks before the Government was seen to act. In a crisis, the NHS operates at one of four different incident levels – described on page 11 of the National Incident Response Plan – that is decided according to the severity and impact of the incident on the health service. At Level 4, NHS England takes control of the overall coordination of the NHS's response. What this means in practice is that, in data terms, NHS England took operational control of care providing bodies such as hospitals, and so became a joint data controller of all of the data flowing through and around the NHS at the very beginning of the pandemic. -

Governing the UK Contribution to Health Security: in Our National Interest?
Governing the UK Contribution to Health Security: in Our National Interest? Emily McMullen ( [email protected] ) King’s College London Research Keywords: Global Health Security, Health Security, Global Health Diplomacy, COVID-19, Governance Posted Date: September 28th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-83030/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/11 Abstract Introduction Recent shifts in the UK international development and foreign policy landscape have revealed a broader scope for global health security activity across UK funding and policy priorities. A lack of clarity surrounding the governance architecture for the expanding UK health security community has led to a risk of fragmentation within the health, development and foreign policy communities. The study aimed to explore the contemporary governance capacity around the UK health security community through the accounts of its leaders and decision makers. Methods A qualitative research study was undertaken in the form of once off, semi-structured, in depth interviews with 12 key informants. Interviews were audio recorded and transcribed. Thematic analysis was used to code the data into themes. These coded transcripts and observations were supported by a review of contemporary literature and policy documentation in order to form a narrative of ndings and draw conclusions. Results UK global health leaders and decision makers considered the governance architecture of the expanding UK health security community to be of insucient capacity. The need for stronger governance is essential to make a compelling case for the ongoing political commitment and resourcing of the UK contribution to global health security, and its impact on wider UK global health efforts. -

Opinion on the Organisation of Resilient Health and Social Care Following the COVID-19 Pandemic
THE ORGANISATION OF RESILIENT HEALTH AND SOCIAL CARE FOLLOWING THE COVID-19 PANDEMIC Opinion of the Expert Panel on effective ways of investing in Health (EXPH) Health Further information on the Health and Food Safety Directorate-General is available on the internet at: http://ec.europa.eu/dgs/health_food-safety/index_en.htm Neither the European Commission nor any person acting on behalf of the Commission is responsible for the use that might be made of the following information. Luxembourg: Publications Office of the European Union, 2020 © European Union, 2020 Reuse is authorised provided the source is acknowledged. The reuse policy of European Commission documents is regulated by Decision 2011/833/EU (OJ L 330, 14.12.2011, p. 39). For any use or reproduction of photos or other material that is not under the EU copyright, permission must be sought directly from the copyright holders. © Photos : https://www.gettyimages.com/, Health and Food Safety Directorate-General Print ISBN 978-92-76-26123-0 doi:10.2875/158132 EW-06-20-027-EN-C PDF ISBN 978-92-76-26122-3 doi:10.2875/005848 EW-06-20-027-EN-N EXPERT PANEL ON EFFECTIVE WAYS OF INVESTING IN HEALTH (EXPH) Opinion on the organisation of resilient health and social care following the COVID-19 pandemic The EXPH adopted this opinion at the 5th plenary on 25 November 2020 after public hearing on 20 October 2020 The organisation of resilient health and social care following the COVID-19 pandemic About the Expert Panel on effective ways of investing in health (EXPH) Sound and timely scientific advice is an essential requirement for the Commission to pursue modern, responsive and sustainable health systems. -

Paramedic Experiences of Providing Care in Wales (UK) During the 2020 COVID-19 Pandemic (PECC-19): a Qualitative Study Using Evolved Grounded Theory
Open access Original research BMJ Open: first published as 10.1136/bmjopen-2021-048677 on 17 June 2021. Downloaded from Paramedic experiences of providing care in Wales (UK) during the 2020 COVID-19 pandemic (PECC-19): a qualitative study using evolved grounded theory Nigel Rees ,1 Lauren Smythe,1 Chloe Hogan,1 Julia Williams2 To cite: Rees N, Smythe L, ABSTRACT Strengths and limitations of this study Hogan C, et al. Paramedic Objective To explore paramedic experiences of providing experiences of providing care care during the 2020 COVID-19 pandemic and develop in Wales (UK) during the 2020 ► The study was set up rapidly in one UK ambulance theory in order to inform future policy and practice. COVID-19 pandemic (PECC-19): service very early in their response to COVID-19. Design Qualitative study using constructivist evolved a qualitative study using evolved This was a unique opportunity to capture experienc- grounded theory. BMJ Open grounded theory (EGT) methodology. One- to-one es of Paramedics providing care as the pandemic 2021;11:e048677. doi:10.1136/ semistructured interviews were conducted using a general unfolded. bmjopen-2021-048677 interview guide. Voice over Internet Protocol was used ► A rich evolved grounded theory has been construct- through Skype. Prepublication history and ed on the Tragic Choices in providing paramedic care ► Setting Conducted between March 2020 and November additional online supplemental during the 2020 COVID-19 pandemic, but is limited material for this paper are 2020 in the Welsh Ambulance Services National Health by being conducted in one ambulance service. Services Trust UK which serves a population of three available online. -

Executive Summary Introduction
Written Evidence Submitted by Edward Sudall (CLL0109) Executive Summary ● The evidence base of lessons learnt to avert poor COVID-19 response existed before the onset of COVID-19. The political under-prioritisation of preparedness in response to prior policy documents is partially to blame for Britain's under performance. ● The dictum to ‘Follow The Science’ is problematic and counter-intuitively indicative of poor use of the necessarily broad scientific evidence base and uncertain information required to face the complexity of a pandemic ● Demarcating science from non-science in lending epistemic authority to British made epidemiological models rather than precautionary emergency management illustrates systematic errors. ● Socially constructed assumptions about risks and anxieties shaped how British decision-makers responded, and did not respond, to the threat of COVID-19. ● Whitehall communications in COBR-SAGE foster miscommunication by design in having too many voices, an overabundance of expertise, and diffuse responsibility. ● British policies such as The Civil Contingencies Act and UK Concept of Operations are agents in the process of decision-making and are too generally designed around frequent risk ‘emergencies’, such as terrorist and national security issues, than national scale rare yet high magnitude hazards such as pathogen outbreaks. Introduction 1. My name is Edward Sudall and I am submitting evidence. I am an MSc student at the department of Science and Technology Studies (STS) at University College London (UCL). I worked as an uploader who edited articles from The Washington Post, The New York Times, and our own reporters at The Independent newspaper from January 2020. I am therefore familiar with the real-time commentary and media response to COVID-19. -

CONTENTS 1 Email Detailing COBR Was Role Play – No Ministerial
CONTENTS Email detailing COBR was role play – no ministerial 1 1 involvement 2 SG participants feedback form/Exercise Evaluation Form 2 3 Debrief Forms 24 4 DH Sitrep Template email & Template 26 5 SG Sitreps 33 Social Care Capacity Assessments (Extract from - ‘Influenza Pandemic Preparedness – 6 39 Guidance for Health & Social Care Services in Scotland (2018) (Draft)’) 1. COBR Meetings Page 5 states that COBRA meetings of Exercise Cygnus were attended by “Ministers and Health Officials from the Devolved Administrations”- Please provide the title of Scottish Government Ministers (including the First Minister), Cabinet Secretaries and health officials that attended each of the four COBRA meetings. The Exercise Cygnus report on page 5 states that “The exercise activity was based around four simulated COBR meetings”. No ministers were involved. 2 officials (Deputy Chief Medical Officer and Director of Performance & Delivery Directorate) participated in a role play. 1 2.1 SG Feedback (Health Protection Unit) EXERCISE CYGNUS PARTICIPANT LESSONS IDENTIFIED AND FEEDBACK FORM Name (optional) REDACTED……. Role in exercise REDACTED observer 1. For me the two least successful aspects of managing the response to the incident were: The difficulty in actually making hard decisions (e.g. re: population triage) Lack of clarity around the roles and expectations of different parts of the SG in the response. 2. For me the two most successful aspects of managing the response to the scenario were: Good engagement by senior SG people. Effective meetings. 3. The most significant thing I have learnt from the exercise is: Pan flu is much worse, more complicated and with far more complex far-reaching implications than I had realised.