Type 1 Diabetes: Management Strategies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of Diabetes Mellitus Standards of Care and Clinical Practice Guidelines
WHO-EM/DIN6/E/G MANAGEMENT OF DIABETES MELLITUS STANDARDS OF CARE AND CLINICAL PRACTICE GUIDELINES Edited by Dr A.A.S. Alwan Regional Adviser, Noncommunicable Diseases WHO Regional Office for the Eastern Mediterranean WHO-EM/DIN6/E/G INTRODUCTION Available data from many countries of the Eastern Mediterranean Region (EMR) indicate that diabetes mellitus has become a problem of great magnitude and a major public health concern. Studies have demonstrated that, in some countries, diabetes affects up to 10% of the population aged 20 years and older. This rate may be doubled if those with impaired glucose tolerance (IGT) are also included. The manifestations of diabetes cause considerable human suffering and enormous economic costs. Both acute and late diabetic complications are commonly encountered. Long-term complications represented by cardiovascular diseases, cerebrovascular accidents, end-stage renal disease, retinopathy and neuropathies are already major causes of morbidity, disability and premature death in countries of this Region. The development of long-term complications is influenced by hyperglycaernia. Poor control of diabetes accelerates their progression. Thus, to prevent complications, good control of diabetes is essential and the management of diabetes should therefore aim to improve glycaemic control beyond that required to control its symptoms. Intensified therapy and maintaining near-normal blood glucose levels can result in considerable reduction in the risk of development of retinopathy, nephropathy and neuropathy. However, despite the high prevalence of diabetes and its complications and the availability of successful prevention strategies, essential health care requirements and facilities for self-care are often inadequate in this Region. Action is needed at all levels of health care and in the various aspects of diabetes care to bridge this gap and to improve health care delivery to people with diabetes. -

Clinical Use of Hemoglobin A1c to Improve Diabetes Management
PRACTICAL POINTERS Clinical Use of Hemoglobin A1c to Improve Diabetes Management Alan M. Delamater, PhD, ABPP or more than 25 years, the hemo- one recent study conducted in Norway6 A1C values. Only 14% of the youths globin A1c (A1C) test has been revealed that the majority (82.6%) of were able to accurately describe the A1C Fthe most widely accepted out- 201 adult patients with type 1 diabetes test. Just 11, 7.8, and 7.8% correctly come measure for evaluating glycemic knew what their last A1C was, and most identified the A1C ranges for good, fair, control in individuals with diabetes. patients (90%) knew what a satisfactory and poor glycemic control, respectively. The test provides an index of a patient’s A1C value would be. But a significant Very few youths (1.6–3.2%) knew the average blood glucose level during the number of patients (42%) reported they blood glucose values corresponding to past 2–3 months1 and is considered to had low knowledge of A1C testing in specific A1C results. Only a small num- be the most objective and reliable general. Furthermore, 25% of patients ber of youths correctly estimated the measure of long-term metabolic con- did not think that treatment intensifica- short- and long-term risks associated trol.2,3 The Diabetes Control and tion should occur at an A1C value of with A1C values of 7 and 12%. In this Complications Trial established that 10%. sample, there was a significant lack of maintaining A1C levels as close as pos- A recent cross-sectional study knowledge concerning the meaning and sible to the normal range results in con- examined the relationship between implications of the A1C test. -

Glossary of Technical Terms
THIS DOCUMENT IS IN DRAFT FORM, INCOMPLETE AND SUBJECT TO CHANGE AND THAT THE INFORMATION MUST BE READ IN CONJUNCTION WITH THE SECTION HEADED “WARNING” ON THE COVER OF THIS DOCUMENT. GLOSSARY OF TECHNICAL TERMS This glossary contains explanations of certain technical terms used in this Document in connection with our Company and its business. Such terminology and meanings may not correspond to standard industry meanings or usages of those terms. “acetaminophen” a non-opioid analgesic and antipyretic agent used to treat pain and fever “artificial pancreas” an integrated diabetes management system that tracks blood glucose levels using a continuous glucose monitor and automatically delivers the insulin when needed using an insulin pump according to its control algorithm “ascorbic acid” a potent reducing and antioxidant agent that functions in fighting bacterial infections, in detoxifying reactions, and in the formation of collagen in fibrous tissue, teeth, bones, connective tissue, skin, and capillaries “basal insulin” a small, continuous infusion of background insulin delivered automatically at a programmed rate, all day and night “BG Port” blood glucose strip port, the port that accepts and electrically connects a disposable blood glucose strip to the electronics “BGMS” blood glucose monitoring system “BLE” bluetooth low energy “blood glucose” blood glucose, also referred to as blood sugar, is the amount of glucose in your blood, an indicator of diabetes monitoring “bolus insulin” insulin that is taken to lower abnormally high blood glucose -
Diabetes Management: Directory of Provider Resources (PDF)
DIABETES MANAGEMENT: DIRECTORY OF PROVIDER RESOURCES 2 Diabetes Management: Directory of Provider Resources ACKNOWLEDGMENTS Diabetes Management: Directory of Provider Resources was prepared with input from National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases; Centers for Medicare & Medicaid Services Advisory Panel on Outreach and Education; NORC at the University of Chicago; Jamie Murkey, MPH, PhD, Program Alignment and Partner Engagement Group 2019 summer intern; Asian Services in Action – International Community Health Center; Chinatown Public Health Center; Colorado Coalition for the Homeless; Garden City Community Health Center, Genesis Family Health; Jackson Medical Mall and Jackson Hinds Comprehensive Health Center; Montefiore Medical Center; Nash Health Care Systems; Sun Life Family Health Center; and Bryan W. Whitfield Memorial Hospital, Tombigbee Healthcare Authority. 3 Diabetes Management: Directory of Provider Resources PURPOSE The purpose of this directory is to support providers and care teams by identifying resources on the management of type 2 diabetes. It is particularly suited for providers who work with Medicare beneficiaries and vulnerable populations for whom the prevalence of type 2 diabetes and diabetes complications is higher. This directory will help the care team identify resources to improve diabetes management by promoting medication adherence. This directory also aims to equip primary care teams with tools to manage diabetes and that patients with more complex needs are appropriately referred to specialists. While some patients require care from endocrinologists, primary care teams can effectively manage many patients with prediabetes and type 2 diabetes.i Other health professionals and patients can play an important role in facilitating medication management and other diabetes self-care behaviors. -

Delivering on Our Commitment to Patients
Delivering on our commitment to patients Zealand Pharma Corporate Presentation Forward-looking statements This presentation contains information pertaining to Zealand Pharma A/S (“Zealand"). Neither Zealand nor its management, directors, employees or representatives make any representation or warranty, express or implied, as to the accuracy or completeness of any of the information contained in this presentation or any other information transmitted or made available to the viewer or recipient hereof, whether communicated in written or oral form. This presentation does not constitute or form part of, and should not be construed as, an offer to sell or issue or the solicitation of an offer to buy or acquire Zealand securities, in any jurisdiction, or an inducement to enter into investment activity, nor shall there be any sale of Zealand securities in any state or jurisdiction in which such offer, solicitation or sale would be unlawful prior to registration or qualification under the securities laws of any such state or jurisdiction. No part of this presentation, nor the fact of its distribution, should form the basis of, or be relied on in connection with, any contract or commitment or investment decision whatsoever. This presentation contains forward-looking statements that reflect management's current views with respect to Zealand's product candidates' development, clinical and regulatory timelines and anticipated results, market opportunity, potential financial performance and other statements of future events or conditions. Although Zealand believes that the expectations reflected in such forward-looking statements are reasonable, no assurance can be given that such expectations will prove to have been correct. Accordingly, results could differ materially from those set out in the forward-looking statements as a result of various factors, many of which are beyond Zealand’s control. -

Insulin Replacement Therapy
Diabetes Educational Services Training Healthcare Professionals On State of the Art Diabetes Care Insulin Replacement Therapy Another Downloadable Article from the Diabetes Educational Services Site Insulin Replacement Therapy is an excellent review of strategies to effectively dose and adjust insulin for patients with type 1 and type 2 diabetes. It is authored by our faculty member, Evelyne Fleury Milfort. Diabetes Educational Services Beverly Dyck Thomassian 45 Old Chico Way Chico, CA 95928 530 893-8635 [email protected] http://www.diabetesed.net/ Insulin Replacement Therapy Vol. 16 •Issue 11 • Page 32 2009 Diabetes CE Insulin Replacement Therapy Minimizing Complications and Side Effects by Evelyne Fleury-Milfort, NP Objectives: The purpose of this article is to educate nurse practitioners about insulin replacement therapy. After reading this article, the nurse practitioner should be able to: * define insulin replacement therapy and discuss appropriate candidates for this form of insulin management * describe the major components of insulin replacement therapy * identify criteria for choosing insulin regimen modalities * explain the initiation and titration process for multiple daily injections and insulin pump therapy. Insulin therapy is the cornerstone of treatment for all patients with type 1 diabetes and for patients with type 2 diabetes who reach severe beta cell failure. Multiple studies have documented the importance of optimal glucose control to prevent the devastating complications of the disease. The best strategy to achieve optimal glucose control is to imitate normal insulin delivery. This continuing education article discusses strategies for the initiation and titration of insulin replacement therapy. Current State of Diabetes Diabetes has reached an epidemic level in the United States. -
Enhance Detection of Recent Hyperglycemia with a Simple Blood Test
Enhance detection of recent hyperglycemia with a simple blood test. The GlycoMark® Test Detects recent hyperglycemia and hyperglycemic excursions. Reveals improving or worsening glycemic control for the prior one to two weeks. Is independently associated with increased rates of diabetes complications. Identifies patients that may benefit from closer diabetes management. Is a non-fasting, FDA cleared blood test that complements A1C. Nearly 40% of patients in “good control” may have significant postprandial hyperglycemia or glycemic variability.1,2 A1C reflects an individual’s average blood glucose over the prior two to three months. High and low glucose values are NOT represented with A1C. In fact, the estimated blood glucose range for an A1C of 7% is 123 - 185 mg/dL.3 Detect recent hyperglycemia with the GlycoMark test. The GlycoMark test measures 1,5-Anhydroglucitol (1,5-AG), a glucose-like sugar found in most foods.4,5 Glycemic Control Hyperglycemia When blood glucose is well-controlled, When glucose exceeds the renal threshold glucose and 1,5-AG circulate in the bloodstream, (>180 mg/dL†), glycosuria occurs. Glycosuria blocks are filtered in the kidneys and reabsorbed by the body. reabsorption of 1,5-AG. 1,5-AG is excreted in the urine, Urinary 1,5-AG is equal to the ingested 1,5-AG. depleting the serum level. 1,5-AG1,5-AG 1,5-AG1,5-AG ood ood ood ood B B B B L L L L O O O O O O 1,5-AG1,5-AG O O GeGe he he 1,5-AG1,5-AG tribute tribute D D 1,5-AG1,5-AG tribute tribute D D reeree ee all allorgans organs and and tissues tissues -

Management of Type 1 and Type 2 Diabetes Requiring Insulin
■ DRUG REVIEW Management of type 1 and type 2 diabetes requiring insulin DOROTHY ABIOLA, THOZHUKAT SATHYAPALAN, DAVID HEPBURN Insulin is a required therapy for people Symptomatic (ie polyruria, polydipsia, unexplained weight with type 1 diabetes, and its use in the loss) treatment of type 2 diabetes has been • Single fasting plasma glucose ≥7mmol/L increasing in recent years. This article • Single random plasma glucose ≥11.1mmol/L discusses the main types of insulin Asymptomatic currently available, their properties and • A fasting plasma glucose ≥7mmol/L on two separate their role in the management of both occasions OR • A random plasma glucose ≥11.1mmol/L on two separate type 1 and type 2 diabetes. occasions OR • An HbA1c ≥48mmol/mol (6.5%) on two separate occasions OR • An HbA1c ≥48mmol/mol AND a single elevated plasma glucose (fasting ≥7mmol/L or random ≥11.1mmol/L) Note: HbA1c cannot be used for type 1 diabetes diagnosis An HbA1c <48mmol/mol does not exclude type 2 diabetes Table 1. Diagnostic criteria for diabetes mellitus, based on the WHO’s 2006 Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia and 2011 Use of Glycated Haemoglobin in the Diagnosis of Diabetes Mellitus iabetes mellitus is a common chronic condition character- Dised by absolute or relative insulin deficiency, and its prev- alence is increasing across the Western world and developing countries. This is particularly true of type 2 diabetes mellitus (T2DM) and UK data from the Quality and Outcomes Framework (QOF), published in 2015, showed there to be almost 3.5 mil- lion people in the UK with a diagnosis of diabetes.1 Diabetes costs the NHS close to £10 billion annually, with the majority of this cost going towards the treatment of diabetes-related com- plications.2 Furthermore, it is suspected that there are at least 590,000 people in the UK with undiagnosed T2DM.2 This review discusses the role of insulin therapy in type 1 diabetes mellitus (T1DM) and T2DM in the UK, including current guidelines and management options. -

IDF Clinical Practice Recommendations for Managing Type 2 Diabetes in Primary Care
IDF Clinical Practice Recommendations for managing Type 2 Diabetes in Primary Care International Diabetes Federation - 2017 IDF Working Group Duality of interest statement: Chair: All members of the guidelines working group declared dualities of interest in re- Pablo Aschner, MD,MSc, Javeriana University and San Ignacio University Hospital, spect of commercial enterprises, governments and non-governmental organ- Bogota, Colombia. isations. No fees were paid to Working Group members in connection with the current activity Core Contributors: Amanda Adler, MD, PhD, FRCP, Addenbrooke´s Hospital and National Institute for Copyright Health and Care Excellence(NICE), Cambridge, UK Cliff Bailey, PhD, FRCP(Edin), FRCPath, Aston University, Birmingham, UK All rights reserved. No part of this publication may be reproduced or transmit- ted in any form or by any means without the written prior permission of the Juliana CN Chan, MB ChB, MD, MRCP (UK), FRCP (Lond), FRCP (Edin), FRCP (Glasgow), FHKAM (Medicine), Hong Kong Institute of Diabetes and Obesity, The Chinese IDF. Requests to reproduce or translate IDF publications should be addressed to University of Hong Kong and Prince of Wales Hospital, Hong Kong, China [email protected] MB, BS Honours Class II, FRACP, The Boden Institute, University of Stephen Colagiuri, © International Diabetes Federation 2017 Sydney, Sydney, Australia Caroline Day, PhD, FRSB, MedEd UK and Aston University, Birmingham, UK Publisher: Juan Jose Gagliardino, MD, Cenexa (Unlp-Conicet), La Plata, Argentina Lawrence A. Leiter, -

Value of Serum 1,5-Anhydroglucitol Measurements in Childhood Obesity in the Continuum of Diabetes
Original article http://dx.doi.org/10.6065/apem.2015.20.4.192 Ann Pediatr Endocrinol Metab 2015;20:192-197 Value of serum 1,5-anhydroglucitol measurements in childhood obesity in the continuum of diabetes Ha Yeong Yoo, MD, Purpose: The prevalence of type 2 diabetes mellitus (T2DM) and obesity are Byung Ok Kwak, MD, currently increasing. Accordingly, the concept of “preventing diabetes” in high- Jae Sung Son, MD, PhD, risk groups has become more important in diabetic care, but the use of glycated Kyo Sun Kim, MD, PhD, hemoglobin (HbA1c) as a measure has limitations in this field. The aim of this Sochung Chung, MD, PhD study was to investigate the utility of 1,5-anhydroglucitol (1,5-AG) in assessing prediabetes status in obese children. Methods: The medical records of 74 subjects aged 6–19 years (of which 27 were Department of Pediatrics, Konkuk overweight/obese and 47 had diabetes) who had 1,5-AG data were reviewed University Medical Center, Konkuk University School of Medicine, Seoul, retrospectively. We compared 1,5-AG with HbA1c using the Pearson correlation test Korea to assess the clinical utility of 1,5-AG. Results: 1,5-AG levels were higher (31.1±10.1 μg/mL vs. 7.4±7.3 μg/mL) and HbA1c levels were lower (5.5%±0.3% vs. 8.9%±2.7%) in the overweight/obese group than in the diabetics group. The range of 1,5-AG levels in obese children was wide (16.8–59.3 μg/mL), and did not have significance with HbA1c. -
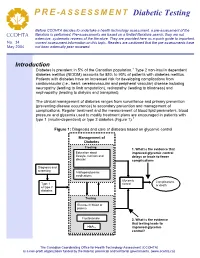
Diabetic Testing
PRE -ASSESSMENT Diabetic Testing Before CCOHTA decides to undertake a health technology assessment, a pre-assessment of the literature is performed. Pre-assessments are based on a limited literature search; they are not CCOHTA extensive, systematic reviews of the literature. They are provided here as a quick guide to important, No. 34 current assessment information on this topic. Readers are cautioned that the pre-assessments have May 2004 not been externally peer reviewed. Introduction Diabetes is prevalent in 5% of the Canadian population.1 Type 2 non-insulin dependent diabetes mellitus (NIDDM) accounts for 85% to 90% of patients with diabetes mellitus. Patients with diabetes have an increased risk for developing complications from cardiovascular (i.e., heart, cerebrovascular and peripheral vascular) disease including neuropathy (leading to limb amputation), retinopathy (leading to blindness) and nephropathy (leading to dialysis and transplant). The clinical management of diabetes ranges from surveillance and primary prevention (preventing disease occurrence) to secondary prevention and management of complications. Regular treatment and the measurement of blood lipid parameters, blood pressure and glycemia used to modify treatment plans are encouraged in patients with type 1 (insulin-dependent) or type 2 diabetes (Figure 1).1 Figure 1: Diagnosis and care of diabetes based on glycemic control Management of Diabetes Treating:Treating 1. What is the evidence that LifestyleEducation –about physical improved glycemic control nutritional,lifestyle, nutrition and and delays or leads to fewer disease knowledge complications education Diagnosis and and screening screening AntihyperglycemicAntihyperglycemic medications Glycemic Complications Type 1 control Type 1 or death or typetype 2 2 diabetes diabetes Testing:Testing GlucoseFasting in bloodplasma or plasmaglucose Fructosamine 2. -

Hemoglobin A1c in the Diagnosis and Management of Diabetes
DCCT UKPDS Hemoglobin A1c in the Diagnosis and Management of A1c Assay Diabetes Standardization Ignoring Biological Diabetes Variation in A1c Monitoring Non-enzymatic Biochemistry Separation Science ObjectivesObjectives 1.1. DescribeDescribe whatwhat clinicalclinical laboratorieslaboratories actuallyactually measuremeasure asas HbA1cHbA1c 2.2. ShowShow thatthat HbA1cHbA1c andand meanmean bloodblood glucoseglucose areare notnot interchangeableinterchangeable estimatesestimates ofof glycemicglycemic controlcontrol 3.3. ExplainExplain howhow biologicalbiological variationvariation inin HbA1cHbA1c complicatescomplicates newnew guidelinesguidelines forfor thethe diagnosisdiagnosis andand managementmanagement ofof diabetesdiabetes Main Take-home Message MBG = A1c The quantitative relationship between blood glucose MBG A1c concentration and hemoglobin A1c is not the same in all people globins (A415 nm) Globin Association is Dynamic MW 15258 15867 31125 62249 + → + ↔ Monomers Dimers Tetramer Higher Hemoglobin Concentration Higher pH Oxygenation Known Glucose Binding Sites 1 Order of affinity 8 Val1 40 17 Lys66 Lys61 61 Lys17 Val1 Lys40 Lys8 V --N=CH+ H2O 2 ׀ Non-enzymatic HCOH Labile A1c ׀ Hb glycation HOCH (aldimine/Schiff base) ׀ HCOH ׀ 1 HCOH ׀ id ap R CH2OH S V--NH2 HC=O lo w V--NH--CH2 ׀ ׀ HCOH 2 C=O ׀ ׀ HOCH HOCH ׀ + ׀ HCOH + HCOH ׀ ׀ HCOH MaillardMaillard HCOH ׀ ׀ CH2OH ReactionReaction CH2OH Glucose Stable A1c globin (ketoamine/Amadori) -NH Role of lysine V- 2 Schiff base and -amino K N=CH + H2O ׀ groups HCOH Slo ׀ 1 w id HOCH V--NH2 2 ׀ ap R HCOH ׀ V--NH2 HCOH K --NH--CH2 ׀ 2 ׀ HC=O CH2OH C=O ׀ ׀ K-NH2 HCOH HOCH ׀ ׀ ++ HOCH HCOH ׀ ׀ HCOH HCOH ׀ ׀ HCOH CH2OH 2 ׀ CH2OH Amadori globin Glucose Discovery of Hemoglobin Heterogeneity 1950 1960 1970 1980 1990 2000 2010 2020 Fast Hb Sickle Hemoglobin Heterogeneity in Normal Blood IRC-50 (Bio-Rex) Fast Hb Fast Hb cation exchange Morrison M, Cook JL.