Human Cytomegalovirus Use and Manipulation of Host Phospholipids
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gingival!Health!Transcriptome!
! ! ! Gingival!Health!Transcriptome! ! Thesis! ! Presented!in!Partial!Fulfillment!of!the!Requirements!for!the!Degree!Master!of! Science!in!the!Graduate!School!of!The!Ohio!State!University! ! By! Christina!Zachariadou,!DDS! Graduate!Program!in!Dentistry! The!Ohio!State!University! 2018! ! ! Thesis!Committee:! Angelo!J.!Mariotti,!DDS,!PhD,!Advisor! Thomas!C.!Hart,!DDS,!PhD! John!D.!Walters,!DDS,!MMSc! ! ! ! 1! ! ! ! ! ! ! ! ! ! ! Copyright!by! Christina!Zachariadou! 2018! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! 2! ! ! ! Abstract! ! Introduction:!In!the!field!of!periodontology,!a!satisfactory!definition!of!periodontal! health!is!lacking.!Instead,!clinicians!use!surrogate!measures,!such!as!color,!texture,! consistency,!probing!depths!and!bleeding!on!probing!to!examine!periodontal!tissues! and! diagnose! disease,! or! the! absence! of! it,! which! they! define! as! “clinical! health”.!! Additionally,!it!has!been!shown!that!age!progression!is!accompanied!by!changes!in! the!periodontium.!As!a!result,!understanding!the!gene!expression!in!healthy!gingiva,! through!the!field!of!transcriptomics,!could!provide!some!insight!on!the!molecules! that!contribute!to!gingival!health.!Also,!comparing!the!transcriptome!of!young!and! older!subjects,!taking!into!consideration!the!effect!of!sex/gender,!can!shed!light!on! differential! gene! expression! with! age! progression! and! on! individual! differences! between! sexes,! and! may! provide! future! therapeutic! endpoints! of! periodontal! treatment.!The!main!focus!of!this!study!was!to!ascertain!collagen!(COL)!and!matrix! -

Transdifferentiation of Human Mesenchymal Stem Cells
Transdifferentiation of Human Mesenchymal Stem Cells Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades der Julius-Maximilians-Universität Würzburg vorgelegt von Tatjana Schilling aus San Miguel de Tucuman, Argentinien Würzburg, 2007 Eingereicht am: Mitglieder der Promotionskommission: Vorsitzender: Prof. Dr. Martin J. Müller Gutachter: PD Dr. Norbert Schütze Gutachter: Prof. Dr. Georg Krohne Tag des Promotionskolloquiums: Doktorurkunde ausgehändigt am: Hiermit erkläre ich ehrenwörtlich, dass ich die vorliegende Dissertation selbstständig angefertigt und keine anderen als die von mir angegebenen Hilfsmittel und Quellen verwendet habe. Des Weiteren erkläre ich, dass diese Arbeit weder in gleicher noch in ähnlicher Form in einem Prüfungsverfahren vorgelegen hat und ich noch keinen Promotionsversuch unternommen habe. Gerbrunn, 4. Mai 2007 Tatjana Schilling Table of contents i Table of contents 1 Summary ........................................................................................................................ 1 1.1 Summary.................................................................................................................... 1 1.2 Zusammenfassung..................................................................................................... 2 2 Introduction.................................................................................................................... 4 2.1 Osteoporosis and the fatty degeneration of the bone marrow..................................... 4 2.2 Adipose and bone -

Variation in Protein Coding Genes Identifies Information Flow
bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 1 1 2 3 4 5 Variation in protein coding genes identifies information flow as a contributor to 6 animal complexity 7 8 Jack Dean, Daniela Lopes Cardoso and Colin Sharpe* 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Institute of Biological and Biomedical Sciences 25 School of Biological Science 26 University of Portsmouth, 27 Portsmouth, UK 28 PO16 7YH 29 30 * Author for correspondence 31 [email protected] 32 33 Orcid numbers: 34 DLC: 0000-0003-2683-1745 35 CS: 0000-0002-5022-0840 36 37 38 39 40 41 42 43 44 45 46 47 48 49 Abstract bioRxiv preprint doi: https://doi.org/10.1101/679456; this version posted June 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Animal complexity and information flow 2 1 Across the metazoans there is a trend towards greater organismal complexity. How 2 complexity is generated, however, is uncertain. Since C.elegans and humans have 3 approximately the same number of genes, the explanation will depend on how genes are 4 used, rather than their absolute number. -

Comparative Muscle Transcriptome Associated with Carcass Traits of Nellore Cattle Bárbara Silva-Vignato1* , Luiz L
Silva-Vignato et al. BMC Genomics (2017) 18:506 DOI 10.1186/s12864-017-3897-x RESEARCH ARTICLE Open Access Comparative muscle transcriptome associated with carcass traits of Nellore cattle Bárbara Silva-Vignato1* , Luiz L. Coutinho2, Aline S. M. Cesar2, Mirele D. Poleti2, Luciana C. A. Regitano3 and Júlio C. C. Balieiro4 Abstract Background: Commercial cuts yield is an important trait for beef production, which affects the final value of the products, but its direct determination is a challenging procedure to be implemented in practice. The measurement of ribeye area (REA) and backfat thickness (BFT) can be used as indirect measures of meat yield. REA and BFT are important traits studied in beef cattle due to their strong implication in technological (carcass yield) and nutritional characteristics of meat products, like the degree of muscularity and total body fat. Thus, the aim of this work was to study the Longissimus dorsi muscle transcriptome of Nellore cattle, associated with REA and BFT, to find differentially expressed (DE) genes, metabolic pathways, and biological processes that may regulate these traits. Results: By comparing the gene expression level between groups with extreme genomic estimated breeding values (GEBV), 101 DE genes for REA and 18 for BFT (false discovery rate, FDR 10%) were identified. Functional enrichment analysis for REA identified two KEGG pathways, MAPK (Mitogen-Activated Protein Kinase) signaling pathway and endocytosis pathway, and three biological processes, response to endoplasmic reticulum stress, cellular protein modification process, and macromolecule modification. The MAPK pathway is responsible for fundamental cellular processes, such as growth, differentiation, and hypertrophy. For BFT, 18 biological processes were found to be altered and grouped into 8 clusters of semantically similar terms. -

Spen Modulates Lipid Droplet Content in Adult Drosophila Glial Cells And
www.nature.com/scientificreports OPEN Spen modulates lipid droplet content in adult Drosophila glial cells and protects against paraquat toxicity Victor Girard1, Valérie Goubard1, Matthieu Querenet1, Laurent Seugnet4, Laurent Pays2,3, Serge Nataf2,3, Eloïse Dufourd1, David Cluet1, Bertrand Mollereau1,5* & Nathalie Davoust1* Glial cells are early sensors of neuronal injury and can store lipids in lipid droplets under oxidative stress conditions. Here, we investigated the functions of the RNA-binding protein, SPEN/SHARP, in the context of Parkinson’s disease (PD). Using a data-mining approach, we found that SPEN/SHARP is one of many astrocyte-expressed genes that are signifcantly diferentially expressed in the substantia nigra of PD patients compared with control subjects. Interestingly, the diferentially expressed genes are enriched in lipid metabolism-associated genes. In a Drosophila model of PD, we observed that fies carrying a loss-of-function allele of the ortholog split-ends (spen) or with glial cell-specifc, but not neuronal-specifc, spen knockdown were more sensitive to paraquat intoxication, indicating a protective role for Spen in glial cells. We also found that Spen is a positive regulator of Notch signaling in adult Drosophila glial cells. Moreover, Spen was required to limit abnormal accumulation of lipid droplets in glial cells in a manner independent of its regulation of Notch signaling. Taken together, our results demonstrate that Spen regulates lipid metabolism and storage in glial cells and contributes to glial cell-mediated neuroprotection. Parkinson’s disease (PD) is a neurodegenerative disorder characterized by the selective loss of dopaminergic neurons in the substantia nigra pars compacta (SN). -
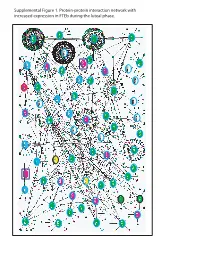
Supplemental Figure 1. Protein-Protein Interaction Network with Increased Expression in Fteb During the Luteal Phase
Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during luteal phase. LEGENDS TO SUPPLEMENTAL FIGURES Supplemental Figure 1. Protein-protein interaction network with increased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with increased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. Genes encoding proteins shown as large ovals highlighted in blue were exclusively found in the first comparison (Manuscript Figure 2), whereas those highlighted in red were only found in the second comparison (Manuscript Figure 3). Genes encoding proteins shown as large ovals highlighted in black were found in both comparisons. The color of each node indicates the ontology of the corresponding protein as determined by the Online Predicted Human Interaction Database (OPHID) link with the NAViGaTOR software. Supplemental Figure 2. Protein-protein interaction network with decreased expression in FTEb during the luteal phase. Submission of probe sets differentially expressed in the FTEb specimens that clustered with SerCa as well as those specifically altered in FTEb luteal samples to the online I2D database revealed overlapping networks of proteins with decreased expression in the four FTEb samples and/or FTEb luteal samples overall. Proteins are represented by nodes, and known and predicted first-degree interactions are represented by solid lines. -

The Changing Chromatome As a Driver of Disease: a Panoramic View from Different Methodologies
The changing chromatome as a driver of disease: A panoramic view from different methodologies Isabel Espejo1, Luciano Di Croce,1,2,3 and Sergi Aranda1 1. Centre for Genomic Regulation (CRG), Barcelona Institute of Science and Technology, Dr. Aiguader 88, Barcelona 08003, Spain 2. Universitat Pompeu Fabra (UPF), Barcelona, Spain 3. ICREA, Pg. Lluis Companys 23, Barcelona 08010, Spain *Corresponding authors: Luciano Di Croce ([email protected]) Sergi Aranda ([email protected]) 1 GRAPHICAL ABSTRACT Chromatin-bound proteins regulate gene expression, replicate and repair DNA, and transmit epigenetic information. Several human diseases are highly influenced by alterations in the chromatin- bound proteome. Thus, biochemical approaches for the systematic characterization of the chromatome could contribute to identifying new regulators of cellular functionality, including those that are relevant to human disorders. 2 SUMMARY Chromatin-bound proteins underlie several fundamental cellular functions, such as control of gene expression and the faithful transmission of genetic and epigenetic information. Components of the chromatin proteome (the “chromatome”) are essential in human life, and mutations in chromatin-bound proteins are frequently drivers of human diseases, such as cancer. Proteomic characterization of chromatin and de novo identification of chromatin interactors could thus reveal important and perhaps unexpected players implicated in human physiology and disease. Recently, intensive research efforts have focused on developing strategies to characterize the chromatome composition. In this review, we provide an overview of the dynamic composition of the chromatome, highlight the importance of its alterations as a driving force in human disease (and particularly in cancer), and discuss the different approaches to systematically characterize the chromatin-bound proteome in a global manner. -

Human COL4A3BP Protein (His & GST Tag)
Human COL4A3BP Protein (His & GST Tag) Catalog Number: 14306-H20B General Information SDS-PAGE: Gene Name Synonym: CERT; CERTL; GPBP; STARD11 Protein Construction: A DNA sequence encoding the human COL4A3BP (Q9Y5P4-1) (Met1- Phe598) was fused with the N-terminal polyhistidine-tagged GST tag at the N-terminus. Source: Human Expression Host: Baculovirus-Insect Cells QC Testing Purity: > 90 % as determined by SDS-PAGE Endotoxin: Protein Description < 1.0 EU per μg of the protein as determined by the LAL method COL4A3BP is a member of the StarD2 subfamily. It contains a pleckstrin homology domain at its amino terminus and a START domain towards the Stability: end of the molecule. COL4A3BP has a lipid-binding domain that mediates intracellular trafficking of ceramide in a non-vesicular manner. One isoform ℃ Samples are stable for up to twelve months from date of receipt at -70 of COL4A3BP is also involved in ceramide intracellular transport. COL4A3BP specifically phosphorylates the N-terminal region of the non- Met Predicted N terminal: collagenous domain of the alpha 3 chain of type IV collagen, known as the Molecular Mass: Goodpasture antigen. An autoimmune response directed at this antigen can cause goodpasture disease. The recombinant human COL4A3BP/GST chimera consists of 835 amino acids and has a calculated molecular mass of 95.8 kDa. The recombinant References protein migrates approximately 96 kDa band in SDS-PAGE under reducing 1.Rual JF, et al. (2005) Towards a proteome-scale map of the human conditions. protein-protein interaction network. Nature. 437(7062):1173-8. 2.Granero F, Formulation: et al. -

The Genomic Landscape of Cutaneous SCC Reveals Drivers and a Novel Azathioprine Associated Mutational Signature
ARTICLE DOI: 10.1038/s41467-018-06027-1 OPEN The genomic landscape of cutaneous SCC reveals drivers and a novel azathioprine associated mutational signature Gareth J. Inman 1, Jun Wang 2, Ai Nagano2, Ludmil B. Alexandrov 3, Karin J. Purdie4, Richard G. Taylor1, Victoria Sherwood1, Jason Thomson4, Sarah Hogan4, Lindsay C. Spender1, Andrew P. South5, Michael Stratton6, Claude Chelala2, Catherine A. Harwood4, Charlotte M. Proby1 & Irene M. Leigh1 1234567890():,; Cutaneous squamous cell carcinoma (cSCC) has a high tumour mutational burden (50 mutations per megabase DNA pair). Here, we combine whole-exome analyses from 40 primary cSCC tumours, comprising 20 well-differentiated and 20 moderately/poorly differ- entiated tumours, with accompanying clinical data from a longitudinal study of immuno- suppressed and immunocompetent patients and integrate this analysis with independent gene expression studies. We identify commonly mutated genes, copy number changes and altered pathways and processes. Comparisons with tumour differentiation status suggest events which may drive disease progression. Mutational signature analysis reveals the pre- sence of a novel signature (signature 32), whose incidence correlates with chronic exposure to the immunosuppressive drug azathioprine. Characterisation of a panel of 15 cSCC tumour- derived cell lines reveals that they accurately reflect the mutational signatures and genomic alterations of primary tumours and provide a valuable resource for the validation of tumour drivers and therapeutic targets. 1 Division of Cancer Research, Jacqui Wood Cancer Centre, School of Medicine, University of Dundee, Dundee DD1 9SY, UK. 2 Centre for Molecular Oncology, Barts Cancer Institute, Queen Mary University of London, London EC1M 6BQ, UK. 3 Department of Cellular and Molecular Medicine and Department of Bioengineering and Moores Cancer Center, University of California, San Diego, La Jolla, CA 92093, USA. -

Anti-COL4A3BP Antibody (ARG64754)
Product datasheet [email protected] ARG64754 Package: 100 μg anti-COL4A3BP antibody Store at: -20°C Summary Product Description Goat Polyclonal antibody recognizes COL4A3BP Tested Reactivity Hu Predict Reactivity Cow, Dog Tested Application WB Specificity This antibody is expected to recognize both reported isoforms (NP_005704.1; NP_112729.1). Host Goat Clonality Polyclonal Isotype IgG Target Name COL4A3BP Antigen Species Human Immunogen C-KREDSWQKRLDKETEK Conjugation Un-conjugated Alternate Names START domain-containing protein 11; STARD11; Goodpasture antigen-binding protein; StARD11; Ceramide transfer protein; CERTL; StAR-related lipid transfer protein 11; CERT; GPBP; MRD34; Collagen type IV alpha-3-binding protein; hCERT Application Instructions Application table Application Dilution WB 1 - 3 µg/ml Application Note WB: Recommend incubate at RT for 1h. * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Calculated Mw 71 kDa Properties Form Liquid Purification Purified from goat serum by ammonium sulphate precipitation followed by antigen affinity chromatography using the immunizing peptide. Buffer Tris saline (pH 7.3), 0.02% Sodium azide and 0.5% BSA Preservative 0.02% Sodium azide Stabilizer 0.5% BSA Concentration 0.5 mg/ml www.arigobio.com 1/2 Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C or below. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. -

Datasheet: VPA00496 Product Details
Datasheet: VPA00496 Description: RABBIT ANTI COL4A3BP Specificity: COL4A3BP Format: Purified Product Type: PrecisionAb™ Polyclonal Isotype: Polyclonal IgG Quantity: 100 µl Product Details Applications This product has been reported to work in the following applications. This information is derived from testing within our laboratories, peer-reviewed publications or personal communications from the originators. Please refer to references indicated for further information. For general protocol recommendations, please visit www.bio-rad-antibodies.com/protocols. Yes No Not Determined Suggested Dilution Western Blotting 1/1000 PrecisionAb antibodies have been extensively validated for the western blot application. The antibody has been validated at the suggested dilution. Where this product has not been tested for use in a particular technique this does not necessarily exclude its use in such procedures. Further optimization may be required dependant on sample type. Target Species Human Product Form Purified IgG - liquid Preparation Rabbit polyclonal antibody purified by affinity chromatography Buffer Solution Phosphate buffered saline Preservative 0.09% Sodium Azide (NaN3) Stabilisers 2% Sucrose Immunogen Synthetic peptide directed towards the N terminal region of human COL4A3BP External Database Links UniProt: Q9Y5P4 Related reagents Entrez Gene: 10087 COL4A3BP Related reagents Synonyms CERT, STARD11 Specificity Rabbit anti Human COL4A3BP antibody recognizes COL4A3BP also known as collagen type IV alpha-3-binding protein, ceramide transfer protein, ceramide transporter, lipid-transfer protein CERTL, Goodpasture antigen-binding protein, START domain-containing protein 11 or StAR-related Page 1 of 2 lipid transfer protein 11. COL4A3BP gene encodes a kinase that specifically phosphorylates the N-terminal region of the non-collagenous domain of the alpha 3 chain of type IV collagen, known as the Goodpasture antigen. -

Lipid Transfer Proteins and Membrane Contact Sites in Human Cancer
fcell-07-00371 January 18, 2020 Time: 17:49 # 1 REVIEW published: 23 January 2020 doi: 10.3389/fcell.2019.00371 Lipid Transfer Proteins and Membrane Contact Sites in Human Cancer Diego Peretti1†, SoHui Kim2†, Roberta Tufi3† and Sima Lev4* 1 UK Dementia Research Institute, Clinical Neurosciences Department, University of Cambridge, Cambridge, United Kingdom, 2 Nakseongdae R&D Center, GPCR Therapeutics, Inc., Seoul, South Korea, 3 MRC Mitochondrial Biology Unit, University of Cambridge, Cambridge, United Kingdom, 4 Molecular Cell Biology Department, Weizmann Institute of Science, Rehovot, Israel Lipid-transfer proteins (LTPs) were initially discovered as cytosolic factors that facilitate lipid transport between membrane bilayers in vitro. Since then, many LTPs have been isolated from bacteria, plants, yeast, and mammals, and extensively studied in cell-free systems and intact cells. A major advance in the LTP field was associated with the discovery of intracellular membrane contact sites (MCSs), small cytosolic gaps between Edited by: the endoplasmic reticulum (ER) and other cellular membranes, which accelerate lipid Mitsuo Tagaya, transfer by LTPs. As LTPs modulate the distribution of lipids within cellular membranes, Tokyo University of Pharmacy and Life and many lipid species function as second messengers in key signaling pathways that Sciences, Japan control cell survival, proliferation, and migration, LTPs have been implicated in cancer- Reviewed by: Tamas Balla, associated signal transduction cascades. Increasing evidence suggests that LTPs play National Institutes of Health (NIH), an important role in cancer progression and metastasis. This review describes how United States Thomas Simmen, different LTPs as well as MCSs can contribute to cell transformation and malignant University of Alberta, Canada phenotype, and discusses how “aberrant” MCSs are associated with tumorigenesis *Correspondence: in human.