WLCCG Board Meeting August 11, 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Covid-19-Weekly-Hotspot-Report-For
Weekly COVID-19 Surveillance Report in Leicestershire Cumulative data from 01/03/2020 - 29/09/2021 This report summarises the information from the surveillance system which is used to monitor the cases of the Coronavirus Disease 2019 (COVID-19) pandemic in Leicestershire. The report is based on daily data up to 29th September 2021. The maps presented in the report examine counts and rates of COVID-19 at Middle Super Output Area. Middle Layer Super Output Areas (MSOAs) are a census based geography used in the reporting of small area statistics in England and Wales. The minimum population is 5,000 and the average is 7,200. Disclosure control rules have been applied to all figures not currently in the public domain. Counts between 1 to 5 have been suppressed at MSOA level. An additional dashboard examining weekly counts of COVID-19 cases by Middle Super Output Area in Leicestershire, Leicester and Rutland can be accessed via the following link: https://public.tableau.com/profile/r.i.team.leicestershire.county.council#!/vizhome/COVID-19PHEWeeklyCases/WeeklyCOVID- 19byMSOA Data has been sourced from Public Health England. The report has been complied by Business Intelligence Service in Leicestershire County Council. Weekly COVID-19 Surveillance Report in Leicestershire Cumulative data from 01/03/2020 - 29/09/2021 Breakdown of testing by Pillars of the UK Government’s COVID-19 testing programme: Pillar 1 + 2 Pillar 1 Pillar 2 combined data from both Pillar 1 and Pillar 2 data from swab testing in PHE labs and NHS data from swab testing for the -

Breakdown of COVID-19 Cases in Leicestershire
Weekly COVID-19 Surveillance Report in Leicestershire Cumulative data from 01/03/2020 - 11/08/2021 This report summarises the information from the surveillance system which is used to monitor the cases of the Coronavirus Disease 2019 (COVID-19) pandemic in Leicestershire. The report is based on daily data up to 11th August 2021. The maps presented in the report examine counts and rates of COVID-19 at Middle Super Output Area. Middle Layer Super Output Areas (MSOAs) are a census based geography used in the reporting of small area statistics in England and Wales. The minimum population is 5,000 and the average is 7,200. Disclosure control rules have been applied to all figures not currently in the public domain. Counts between 1 to 5 have been suppressed at MSOA level. An additional dashboard examining weekly counts of COVID-19 cases by Middle Super Output Area in Leicestershire, Leicester and Rutland can be accessed via the following link: https://public.tableau.com/profile/r.i.team.leicestershire.county.council#!/vizhome/COVID-19PHEWeeklyCases/WeeklyCOVID- 19byMSOA Data has been sourced from Public Health England. The report has been complied by Strategic Business Intelligence in Leicestershire County Council. Weekly COVID-19 Surveillance Report in Leicestershire Cumulative data from 01/03/2020 - 11/08/2021 Breakdown of testing by Pillars of the UK Government’s COVID-19 testing programme: Pillar 1 + 2 Pillar 1 Pillar 2 combined data from both Pillar 1 and Pillar 2 data from swab testing in PHE labs and NHS data from swab testing for the -

Infant Feeding Support Groups Across Leicester, Leicestershire and Rutland
Infant feeding support groups across Leicester, Leicestershire and Rutland Leicester City Venue Day and Time Information Mammas Baby & Me Wednesday Highfields Children Young Help with all feeding issues 0-2 People and Family Centre 10am – 12pm years. Inclusive of bottle feeding Barnard Close issues. Leicester LE2 OUZ Keep up to date Join the (Other venues are also WhatsApp group used) Call /text Nasreen 07402829698 or Sally 07580159278 Please check before attending as some sessions take place in other venues, such as parks, cafes, museums etc Mammas Baby & Me Monday Help with all feeding issues 0-2 Thurnby Lodge Children, years. Inclusive of bottle feeding Young People and Family 1.00 -2.30pm issues. Centre Dudley Avenue Leicester Keep up to date Join the LE5 2EG WhatsApp group Call /text Nasreen 07402829698 or Sally 07580159278 Please check before attending as some sessions take place in other venues, such as parks, cafes, museums etc Mammas Baby & Me Friday Help with all feeding issues 0-2 years. Inclusive of bottle feeding Beaumont Leys Children 10-11.30 issues. and Young People Centres, Home Farm Keep up to date Join the Walk, LE4 0RW WhatsApp group Call /text Nasreen 07402829698 or Sally 07580159278 Please check before attending as some sessions take place in other venues, such as parks, cafes, museums etc Mammas Breastfeeding support group New Parks Children centre 1st and 3rd Pindar Road Tuesday in month LE3 9RN 10-11.30 Fosse Library, 4th Tuesday in Mantle road, month LE3 5HG Braunstone Thursdays Breastfeeding Support 12.30 – 2pm Contact Steph Cave, Healthy Group Child Programme Practitioner Braunstone Children, 0116 3737150 Young People and Family Centre Gallards Hill Leicester LE3 1QR Leicester Bumps Babies Tuesdays Breastfeeding support offered in and Beyond Group 10am – 12pm the group on the first Tuesday of Great Meeting Unitarian the month by trained NCT Chapel Breastfeeding counsellor. -

Breakdown of COVID-19 Cases in Leicestershire
Weekly COVID-19 Surveillance Report in Leicestershire Cumulative data from 01/03/2020 - 05/05/2021 This report summarises the information from the surveillance system which is used to monitor the cases of the Coronavirus Disease 2019 (COVID-19) pandemic in Leicestershire. The report is based on daily data up to 5th May 2021. The maps presented in the report examine counts and rates of COVID-19 at Middle Super Output Area. Middle Layer Super Output Areas (MSOAs) are a census based geography used in the reporting of small area statistics in England and Wales. The minimum population is 5,000 and the average is 7,200. Disclosure control rules have been applied to all figures not currently in the public domain. Counts between 1 to 5 have been suppressed at MSOA level. An additional dashboard examining weekly counts of COVID-19 cases by Middle Super Output Area in Leicestershire, Leicester and Rutland can be accessed via the following link: https://public.tableau.com/profile/r.i.team.leicestershire.county.council#!/vizhome/COVID-19PHEWeeklyCases/WeeklyCOVID- 19byMSOA Data has been sourced from Public Health England. The report has been complied by Strategic Business Intelligence in Leicestershire County Council. Weekly COVID-19 Surveillance Report in Leicestershire Cumulative data from 01/03/2020 - 05/05/2021 Breakdown of testing by Pillars of the UK Government’s COVID-19 testing programme: Pillar 1 + 2 Pillar 1 Pillar 2 combined data from both Pillar 1 and Pillar 2 data from swab testing in PHE labs and NHS data from swab testing for the wider -

East Midlands
Liberal Democrat submission for BCE 3rd consultation East Midlands Submission to the Boundary Commission for England third period of consultation: East Midlands Summary There is a factual error in the Commission’s report concerning the Liberal Democrat counter-proposals in the Leicestershire / Northamptonshire / Nottinghamshire / Rutland sub-region. We would, therefore, ask the Commission to reconsider the scheme we put forward. We welcome the change the Commission has made to its proposal for Mansfield. We welcome the fact that the Commission has kept to its original proposals in Lincolnshire, much of Derbyshire and Derby, and in Northampton. We consider that the changes that the Commission has made to four constituencies in Derbyshire, affecting the disposition of three wards, are finely balanced judgement calls with which we are content to accept the Commission’s view. The change that the Commission has made to the Kettering and Wellingborough constituencies would not have needed to be considered if it had agreed to our proposal for an unchanged Wellingborough seat. The Commission’s proposal to move the Burton Joyce and Stoke Bardolph ward into its proposed Sherwood constituency means that it is now proposing three Nottinghamshire constituencies (Bassetlaw, Broxtowe, Sherwood) which contain a ward which is inaccessible from the rest of the seat. We are not in agreement with the Commission’s failure to comply with the spirit of the legislation or the letter of its own guidelines in respect of these three proposed constituencies. We are not in agreement with the Commission’s failure to respect the boundaries of the City of Nottingham to the extent of proposing three constituencies that cross the Unitary Authority boundary. -

Archaeology in Leicester, Leicestershire and Rutland 2008
230487 10c-241-272 18/10/09 12:17 Page 241 ARCHAEOLOGY IN LEICESTER, LEICESTERSHIRE AND RUTLAND 2008 Edited by Tim Higgins and Nicholas J. Cooper Archaeological watching briefs which have produced no significant archaeological features or finds are listed at the end of the relevant county sections. In each case, the parish/site name is followed by the name of the organisation which undertook the fieldwork. For abbreviations see below p. iv. Some entries may relate to fieldwork undertaken before 2008 but not previously reported. LEICESTER All finds and records are deposited with LCMS under the accession number cited at the end of the entry. Humberstone, Manor Farm (SK 6285 0642) John Thomas Archaeological recording of a medieval windmill mound at Manor Farm, Humberstone was undertaken by ULAS in advance of development by Gateway College. Excavation revealed the mound to consist of two deposits of clay, both associated with a phase of the mound’s development. A re-cut ditch encircled the mound and originally acted as quarry for the mound soils. Beneath the mound, well-preserved timber cross-tree foundations survived in situ within a construction slot cut directly into the natural clay. Pottery recovered from the construction slot and primary fills of each ditch cut indicated a twelfth –thirteenth century period of use for the mill. Later pottery in the final ditch fills suggest the mill ditches had become largely in-filled by the seventeenth –eighteenth century. A6.1999. Leicester Abbey (SK 585 060) Andrew Hyam and Stephen Jones In June and July of 2006 and 2007, ULAS undertook a seventh and eighth season of training excavations at the site of Leicester Abbey, for students of the University’s School of Archaeology and Ancient History. -

Braunstone Parish Leaflet 2021
Braunstone Town Council Council Tax Services 2021/2022 Braunstone Civic Centre Kingsway, Braunstone Town, LE3 2PP Tel: 0116 2890045 Email: [email protected] Function rooms for up to 200 people! ● Weddings ● Parties ● Conferences ● Events ● Community group meetings ● Receptions ● Dances ● Exhibitions ● Civic Community Lounge - Licensed Bar ● Mon-Thurs 12:00-15:00, 17:00-23:00 ● ● Fri-Sat - 12:00-23:30 ● Sun - 12:00-22:30 ● Thorpe Astley Community Centre Lakin Drive, Thorpe Astley, LE3 3RU Tel: 0116 2890704 Email: [email protected] Function rooms for up to 80 people! ● Meeting rooms ● Large main hall ● Full sized football pitch ● Full sized tennis courts ● Multi use games area ● Braunstone Town Community Library On the grounds of Braunstone Civic Centre, King- sway, LE3 2PP Tel: 0116 3055909 ● Daily newspapers ● Internet access ● ● Photocopier ● Computer access ● Opening times: ● Mon 2-7PM ● Tues 2-5PM ● Weds 10-12Noon, 2 -5PM ● Thurs 2-5PM ● Fri 10AM-12Noon, 2-5PM ● Sat 10AM-1PM ● Sun CLOSED ● Braunstone Civic Centre, Kingsway, Braunstone Town, Leicester LE3 2PP Thorpe Astley Community Centre, Lakin Drive, Thorpe Astley, Leicester LE3 3RU Telephone 0116 289 0045 Fax 0116 282 4785 [email protected] www.braunstonetowncouncil.org.uk Budget 2020/2021 Budget 2021/2022 Exp. Inc Net Exp Services Exp Inc Net Exp £90,091.70 £1,560.00 £88,531.70 Corporate Management £96,371.13 £1,560.00 £94,811.13 £215,824.77 £91,971.00 £123,853.77 Braunstone Civic Centre £232,915.69 £84,484.00 £148,431.69 -
Himp Maps Page2
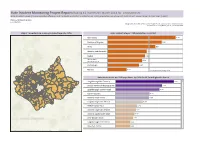
Hate Incident Monitoring Project Report: Rolling 12 months ll March 2014 for Leicestershire Hate Incident Levels (Police recorded offences and incidents and HIMP incidents) per 1000 populaon are shown at District and Lower Super Output Area (LSOA) Choose Partnership Area Leicestershire Designed by Karen Earp, Research & Insight Team , Leicestershire County Council, Contact: [email protected] , 0116 305 7260 Map of Leicestershire showing incident levels by LSOA Hate incident rate per 1000 populaon by district. -1 Charnwood 0.76 -1 Oadby and Wigston 0.61 -1 Blaby 0.53 0 Hinckley and Bosworth 0.44 0 Melton 0.42 North West 0 0.39 Leicestershire 0 Harborough 0.35 0 Rutland 0.21 Leicestershire Average 0.46 Hate incident rate per 1000 populaon by LSOA for All from highest to lowest -9 Loughborough Bell Foundry 9.27 -7 Oadby The Parade & Leicester Ra.. 7.40 -7 Loughborough Toothill Road 7.00 -5 Coalville Centre 5.44 -5 Hinckley Town Centre 5.35 -4 Loughborough Centre South 4.34 -3 Melton Egerton East 3.46 -3 Hinckley Town Centre North 3.24 -3 Hinckley Castle South West 3.06 -3 Lile Bowden South 2.83 -2 Loughborough Centre West 2.39 -2 Measham Centre 2.39 -2 Loughborough Meadow Lane 2.37 About Tableau maps: www.tableausoftware.com/ mapdata Hate Incident Monitoring Project Report: Rolling 12 months ll March 2014 for Blaby Hate Incident Levels (Police recorded offences and incidents and HIMP incidents) per 1000 populaon are shown at District and Lower Super Output Area (LSOA) Choose Partnership Area Blaby Designed by Karen Earp, Research & Insight Team , Leicestershire County Council, Contact: [email protected] , 0116 305 7260 Map of Blaby showing incident levels by LSOA Hate incident rate per 1000 populaon by district. -

Blaby District Council Local Plan (Delivery) Development Plan Document
BRAUNSTONE TOWN COUNCIL www.braunstonetowncouncil.org.uk Darren Tilley – Executive Officer & Town Clerk Braunstone Civic Centre, Kingsway, Braunstone Town, Leicester, LE3 2PP Telephone: 0116 2890045 Fax: 0116 2824785 Email: [email protected] PLANNING APPLICATIONS PUBLIC INSPECTION OF PLANS AND PARTICIPATION 1. The Planning Applications can be inspected at the offices of Blaby District Council to whom representations should be made and they are also available Blaby District Council’s website at www.blaby.gov.uk under Planning Application Search 2. A list of the applications to be considered by the Town Council’s Planning & Environment Committee are listed on the Town Council’s website www.braunstonetowncouncil.org.uk 3. The applications will be considered by the Braunstone Town Council’s Planning and Environment Committee, which may make its own observations and forward them to the relevant Planning Authority. 4. Braunstone Town Council and Blaby District Council have introduced procedures to enable applicants, objectors and supporters to speak on applications brought before their relevant Committees. 10th January 2018 To: Councillor Robert Waterton (Chair), Councillor Sharon Betts (Vice-Chair) and Councillors Parminder Basra, Roger Berrington, David Di Palma, Dinesh Joshi, Berneta Layne, Phil Moitt, Tracey Shepherd, Darshan Singh and Mr John Dodd (Ex- Officio). Dear Councillor You are summoned to attend a meeting of the PLANNING & ENVIRONMENT COMMITTEE to be held in the Fosse Room at Braunstone Civic Centre on Thursday, 18th January 2018 commencing at 7.30pm, for the transaction of the business as set out below. Yours sincerely, Executive Officer & Town Clerk AGENDA 1. Apologies To receive apologies for absence. -
Ageing Well Guide a Directory of Services, Clubs and Activities in Blaby District
Ageing Well Guide A directory of services, clubs and activities in Blaby District Published June 2016 Introduction Welcome to the new Ageing Well Guide for Blaby District. Our Ageing Population remains a priority for Blaby District Council. It is our vision that people are able to enjoy happy, healthy and independent lives, feeling involved and valued in their community during later life. Cllr David Freer – Portfolio Holder for Partnerships & Corporate Services – says: ‘Residents and professionals alike have told us what a valuable resource the Older Persons’ Guide has been and this new edition is bigger than ever. The Council and its partners provide a number of schemes that support our vision for our ageing population. The new Ageing Well Guide includes information about these and the numerous activities that are taking place across our parishes that are all helping in some way to reduce isolation and improve health and wellbeing’. The frst part of this guide provides information about district-wide services that provide help on issues such as health and social care, transport, community safety, money advice and library services. The second part of the guide gives details of clubs and activities taking place in each parish within the district, including GP practices, social or lunch clubs, ftness and exercise classes and special interest or hobby groups. 2 Blaby District Council has taken care to ensure the information in this booklet is accurate at the time of publication. All information has been provided by third parties and the Council cannot be held responsible for any inaccuracies in the information or any changes that may arise, such as changes to any fees, charges or activities listed. -

Asking Price £210,000 27 Larch Grove, Braunstone Town, LE3
Estate Agents Lettings Valuers Mortgages 27 Larch Grove, Braunstone Town, LE3 3FG • Semi-Detached House, Corner Plot • Detached Single Garage & Parking • Lounge\Dining Room & Kitchen • Ideal for Young and Growing Family • 3 Bedrooms & Bathroom • Potential for Further Extension A nicely presented, three bedroomed, semi-detached home situated on a corner plot in this popular location offering easy access to all local facilities. The well planned accommodation comprises a ground floor entrance porch, entrance hall, lounge/dining room and kitchen, together with three first floor bedrooms and bathroom. This property benefits from a gas heating system and double glazing and stands on a corner plot ideally suited for further extension (subject to normal planning consents), together with a driveway leading to a detached single garage. An early viewing is highly recommended to appreciate this home which would ideally suit the young and growing family. EPC TBC. NO UPWARD CHAIN. Asking price £210,000 GENERAL INFORMATION: DETAILED ACCOMMODATION The suburb of Braunstone Town is located to the south of the City of Leicester, just inside ON THE GROUND FLOOR: the City boundary, and is well known for its OVERHEAD CANOPY popularity in terms of convenience for ease of With access through UPVC framed and access to the afore-mentioned City centre and panelled part sealed unit double obscure all the excellent amenities therein, as well as glazed front entrance door with matching side to Junction 21 of the M1/M69 motorway panel to: network for travel north, south and west, and the adjoining Fosse Park and Meridian ENTRANCE PORCH shopping, entertainment, retail and business Hardwood inner door having obscure glazed centres. -
Blaby District Council Ageing Well Guide
Ageing Well Guide A directory of services, clubs and activities in Blaby District Published June 2016 Introduction Welcome to the new Ageing Well Guide for Blaby District. Our Ageing Population remains a priority for Blaby District Council. It is our vision that people are able to enjoy happy, healthy and independent lives, feeling involved and valued in their community during later life. Cllr David Freer – Portfolio Holder for Partnerships & Corporate Services – says: ‘Residents and professionals alike have told us what a valuable resource the Older Persons’ Guide has been and this new edition is bigger than ever. The Council and its partners provide a number of schemes that support our vision for our ageing population. The new Ageing Well Guide includes information about these and the numerous activities that are taking place across our parishes that are all helping in some way to reduce isolation and improve health and wellbeing’. The first part of this guide provides information about district-wide services that provide help on issues such as health and social care, transport, community safety, money advice and library services. The second part of the guide gives details of clubs and activities taking place in each parish within the district, including GP practices, social or lunch clubs, fitness and exercise classes and special interest or hobby groups. 2 Blaby District Council has taken care to ensure the information in this booklet is accurate at the time of publication. All information has been provided by third parties and the Council cannot be held responsible for any inaccuracies in the information or any changes that may arise, such as changes to any fees, charges or activities listed.