January 2015 Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
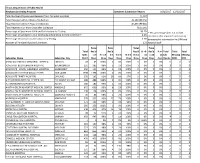
NBS 3Rd Quarter Report
Illinois Department of Public Health Newborn Screening Program Specimen Submission Report 7/1/2018 - 9/30/2018 Total Number of Specimens Received from Perinatal Hospitals 43,345 Total Received within 3 Days of Collection 42,732 (98.6 %) Total Received within 5 Days of Collection 43,297 (99.9 %) Total Received 6 or More Days after Collection 24 (0.1%) Percentage of Specimens Valid and Satisfactory for Testing 92.8% * This percentage does not include Percentage Unsatisfactory Due to Missing Information or Early Collection* 7.0% specimens that required correction of Percentage Unsatisfactory for Laboratory Testing 0.2% demographic information by IDPH and Number of Perinatal Hospital Submitters 121 hospital staff. Total Total Total Total Total Rec'd Rec'd Rec'd % >5- Rec'd Total Total Total Spec. <=3 % <= 3 4-5 % 4-5 % 0-5 >5-14 14 >=14 % >= 14 Lab Missing Missing Submitter Name Submitter City Rec'd Days Days Days Days Days Days Days Days days Unsats DOB DOC ABRAHAM LINCOLN MEMORIAL HOSPITAL LINCOLN 57 57 100% 0 0% 100% 0 0% 0 0% 0 0 0 ADVENTIST BOLINGBROOK HOSPITAL BOLINGBROOK 257 250 97% 5 2% 99% 0 0% 0 0% 0 0 2 ADVOCATE - SOUTH SUBURBAN HOSPITAL HAZELCREST 167 167 100% 0 0% 100% 0 0% 0 0% 0 0 0 ADVOCATE CHRIST MEDICAL CENTER OAK LAWN 1592 1592 100% 0 0% 100% 0 0% 0 0% 2 0 0 ADVOCATE TRINITY HOSPITAL CHICAGO 162 158 98% 4 2% 100% 0 0% 0 0% 0 0 0 ALEXIAN BROS MEDICAL CENTER LAB ELK GROVE VILLAGE 570 557 98% 13 2% 100% 0 0% 0 0% 2 0 0 ALTON MEMORIAL HOSPITAL ALTON 199 197 99% 2 1% 100% 0 0% 0 0% 0 0 0 AMITA HEALTH ADVENTIST MEDICAL CENTER - HHINSDALE 805 801 100% 4 0% 100% 0 0% 0 0% 10 0 0 AMITA HEALTH ADVENTIST MEDICAL CENTER - LLA GRANGE 3 2 67% 1 33% 100% 0 0% 0 0% 0 0 0 AMITA HEALTH-ADVENTIST MEDICAL CENTER - GGLENDALE HEIGHTS 111 107 96% 4 4% 100% 0 0% 0 0% 1 0 0 ANDERSON HOSPITAL MARYVILLE 357 345 97% 12 3% 100% 0 0% 0 0% 0 0 0 ANN & ROBERT H. -
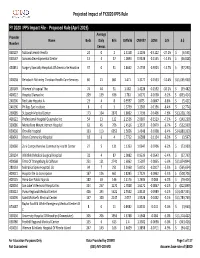
FY 2020 Proposed Rule Impact File.Xlsx
Projected Impact of FY2020 IPPS Rule FY 2020 IPPS Impact File ‐ Proposed Rule (April 2019) Average Provider Name Beds Daily Bills CMIV36 CMIV37 ∆CMI ∆ % ∆ $ Number Census 060107 National Jewish Health 24 0 2 1.5158 1.1036 ‐0.4122 ‐27.2%$ (6,595) 050547 Sonoma Developmental Center 13 4 37 1.0893 0.9338 ‐0.1555 ‐14.3% $ (46,028) 450831 Surgery Specialty Hospitals Of America Se Houston 37 0 31 2.8662 2.4739 ‐0.3923 ‐13.7%$ (97,290) 320038 Rehoboth Mckinley Christian Health Care Services 60 21 861 1.471 1.3177 ‐0.1533 ‐10.4%$ (1,055,930) 150149 Women's Hospital The 74 44 31 1.582 1.4228 ‐0.1592 ‐10.1%$ (39,482) 400022 Hospital Damas Inc 209 139 636 1.781 1.6172 ‐0.1638 ‐9.2%$ (833,414) 240206 Red Lake Hospital A 23 4 8 0.9597 0.875 ‐0.0847 ‐8.8%$ (5,421) 240196 Phillips Eye Institute 8 0 3 1.3739 1.2583 ‐0.1156 ‐8.4%$ (2,774) 260085 St Joseph Medical Center 173 104 2870 1.8602 1.7196 ‐0.1406 ‐7.6%$ (3,228,176) 400122 Professional Hospital Guaynabo Inc 54 13 122 2.1536 2.0007 ‐0.1529 ‐7.1%$ (149,230) 330086 Montefiore Mount Vernon Hospital 63 45 706 1.4516 1.3537 ‐0.0979 ‐6.7%$ (552,939) 050030 Oroville Hospital 133 113 6052 1.5656 1.4648 ‐0.1008 ‐6.4%$ (4,880,333) 460043 Orem Community Hospital 18 6 4 1.7712 1.6588 ‐0.1124 ‐6.3%$ (3,597) 320060 Zuni Comprehensive Community Health Center 27 5 131 1.1353 1.0647 ‐0.0706 ‐6.2%$ (73,989) 250134 Whitfield Medical Surgical Hospital 32 4 87 1.0082 0.9539 ‐0.0543 ‐5.4%$ (37,793) 420068 Trmc Of Orangeburg & Calhoun 251 121 2741 1.6062 1.5207 ‐0.0855 ‐5.3%$ (1,874,844) 280133 Nebraska Spine Hospital, -

The World's Most Active Hospital & Healthcare
The USA's Most Active Hospital & Healthcare Professionals on Social - August 2021 Industry at a glance: Why should you care? So, where does your company rank? Position Company Name LinkedIn URL Location Employees on LinkedIn No. Employees Shared (Last 30 Days) % Shared (Last 30 Days) 1 symplr https://www.linkedin.com/company/symplr/United States 1,101 204 18.53% 2 Covenant Care https://www.linkedin.com/company/covenant-care-corp/United States 509 88 17.29% 3 Johnson & Johnson Consumer Health https://www.linkedin.com/company/johnson-johnson-consumer-health/United States 727 112 15.41% 4 Phreesia https://www.linkedin.com/company/phreesia/United States 1,201 185 15.40% 5 Labcorp Drug Development https://www.linkedin.com/company/labcorpdrugdev/United States 4,362 661 15.15% 6 BrightSpring Health Services https://www.linkedin.com/company/brightspringhealth/United States 17,110 2,500 14.61% 7 Teladoc Health https://www.linkedin.com/company/teladoc-health/United States 3,932 572 14.55% 8 Alto Pharmacy https://www.linkedin.com/company/altopharmacy/United States 749 104 13.89% 9 Quantum Health https://www.linkedin.com/company/quantum-health/United States 899 119 13.24% 10 Imprivata https://www.linkedin.com/company/imprivata/United States 612 78 12.75% 11 American College of Cardiology https://www.linkedin.com/company/american-college-of-cardiology/United States 771 97 12.58% 12 VillageMD https://www.linkedin.com/company/villagemd/United States 862 108 12.53% 13 Oak Street Health https://www.linkedin.com/company/oak-street-health/United States 1,692 211 12.47% 14 ECRI https://www.linkedin.com/company/ecri-org/United States 539 64 11.87% 15 Shields Health Solutions https://www.linkedin.com/company/shields-health-solutions/United States 603 70 11.61% 16 Amwell https://www.linkedin.com/company/amwellcorp/United States 1,104 125 11.32% 17 St. -

Community Health Needs Assessment
Community Health Needs Assessment Northwestern Medicine Huntley Hospital Northwestern Medicine McHenry Hospital Northwestern Medicine Woodstock Hospital Northwestern Medicine Community Health Needs Assessment Northwestern Medicine’s northwest region consists of the following hospitals: Northwestern Medicine Northwestern Medicine Northwestern Medicine Huntley Hospital McHenry Hospital Woodstock Hospital Northwestern Medicine Huntley Hospital, Northwestern Medicine McHenry Hospital, Northwestern Medicine Woodstock Hospital 2 2019 Community Health Needs Assessment Northwestern Medicine Table of contents Introduction . 4 Cancer About Northwestern Memorial HealthCare Respiratory Disease About Northwestern Medicine Huntley Hospital, Diabetes McHenry Hospital and Woodstock Hospital Reproductive Health Acknowledgements Risk Factors Impacting Health Outcomes The Community Health Needs Assessment . 9 Diet & Nutrition Background Physical Activity Goals Overweight and Obesity NM Medicine Huntley Hospital, McHenry Hospital Sexual Health and Woodstock Hospital Community Service Area Sexually Transmitted Diseases Methodology Access to Health Services & Primary Care Providers Primary Data Collection Oral Health Secondary Data Collection Interpreting and Prioritizing Health Needs . 36 Information Gaps Public Dissemination Additional Resources Available to Address Significant Health Needs . 38 Public Comment Prioritization Process of Health Needs . 39 Key Findings . 13 Community Description & Demographics Community Health Needs Assessment Social Determinants -

Mqii Stakeholders and Collaborators
MQii Stakeholders and Collaborators The Malnutrition Quality Improvement Initiative (MQii) is a project of the Academy of Nutrition and Dietetics, Avalere Health, and other stakeholders who provided guidance and expertise through a collaborative partnership. Support for the MQii is provided by Abbott. Special thanks to the members of the MQii Advisory Committee for their guidance in designing and informing the content of the Toolkit; to the members of the Technical Expert Panel for their guidance in specifying and testing the malnutrition electronic clinical quality measures (eCQMs); and to the members of the MQii Learning Collaborative for their work to implement the MQii Toolkit and eCQMs, and provide feedback to inform revisions and future iterations to MQii tools. MQii Advisory Committee Members Al Barrocas, MD, FACS, FASPEN Bob Blancato, MPA Owner of Alma, LLC President Fellow and Co-Chair of ASPEN’s Value Project Matz, Blancato and Associates (Former Chief Medical Officer of WellStar Atlanta (Former Chair of American Society on Aging, Director of Medical Center, Clinical Professor in the Surgery National Association of Nutrition and Aging Services Departments of LSU and Tulane Schools of Medicine) Programs, and board member for AARP) Member: 2020–Present Member: 2020–Present Charley John, PharmD Leslie Kelly-Hall Director of U.S. Public Policy Founder of Engaging Patient Strategy, Senior Vice Walgreens President of Policy Member of Government Affairs Committee at National Healthwise Association of Specialty Pharmacy Member: 2014–Present -
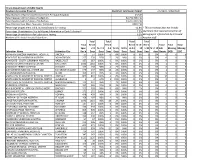
Illinois Department of Public Health Newborn Screening Program Total
Illinois Department of Public Health Newborn Screening Program Specimen Submission Report 10/1/2017 - 12/31/2017 Total Number of Specimens Received from Perinatal Hospitals 41,907 Total Received within 3 Days of Collection 41,180 (98.3%) Total Received within 5 Days of Collection 41,835 (99.8%) Total Received 6 or More Days after Collection 50 (0.2%) Percentage of Specimens Valid and Satisfactory for Testing 93.2% * This percentage does not include Percentage Unsatisfactory Due to Missing Information or Early Collection* 6.6% specimens that required correction of Percentage Unsatisfactory for Laboratory Testing 0.2% demographic information by IDPH and Number of Perinatal Hospital Submitters 123 hospital staff. Total Total Total Total Total Rec'd Rec'd Rec'd % >5- Rec'd % >= Total Total Total Spec. <=3 % <=3 4-5 % 4-5 % 0-5 >5-14 14 >=14 14 Lab Missing Missing Submitter Name Submitter City Rec'd Days Days Days Days Days Days Days Days days Unsats DOB DOC ABRAHAM LINCOLN MEMORIAL HOSPITAL LINCOLN 43 43 100% 0 0% 100% 0 0% 0 0% 0 0 0 ADVENTIST BOLINGBROOK HOSPITAL BOLINGBROOK 291 285 98% 5 2% 100% 1 0% 0 0% 3 0 0 ADVOCATE - SOUTH SUBURBAN HOSPITAL HAZELCREST 156 155 99% 1 1% 100% 0 0% 0 0% 0 0 0 ADVOCATE CHRIST MEDICAL CENTER OAK LAWN 1398 1398 100% 0 0% 100% 0 0% 0 0% 7 0 0 ADVOCATE TRINITY HOSPITAL CHICAGO 176 161 91% 10 6% 97% 5 3% 0 0% 0 0 0 ALEXIAN BROS MEDICAL CENTER LAB ELK GROVE VILLAGE 488 488 100% 0 0% 100% 0 0% 0 0% 0 0 0 ALTON MEMORIAL HOSPITAL ALTON 186 185 99% 1 1% 100% 0 0% 0 0% 0 0 0 AMITA HEALTH ADVENTIST MEDICAL CENTER HINSDALE 672 666 99% 6 1% 100% 0 0% 0 0% 2 0 0 AMITA HEALTH ADVENTIST MEDICAL CENTER LA GRANGE 138 138 100% 0 0% 100% 0 0% 0 0% 0 0 0 AMITA HEALTH-ADVENTIST MED CTR GLENDALE HEIGHTS 90 88 98% 2 2% 100% 0 0% 0 0% 0 0 0 ANDERSON HOSPITAL MARYVILLE 378 352 93% 25 7% 100% 1 0% 0 0% 0 0 0 ANN & ROBERT H. -

The Philanthropist
Volume 6, Issue 1 (March 2019) The Philanthropist A publication for supporters and friends of Northwestern University Feinberg School of Medicine and Northwestern Memorial Foundation Investing in Our People: Changing Lives, Making a Difference Donors who make gifts to Northwestern University Feinberg School of Medicine and Northwestern Memorial Foundation are supporting the very heart of Northwestern Medicine—our people. By investing in our talented physicians, nurses, scientists, medical students, fellowship trainees and other devoted health professionals, you are changing lives and shaping the trajectory of Northwestern Medicine. In this issue, we feature supporters who believe that the greatest impact can be gained by supporting the people who ultimately make a difference in the lives of patients and families, here and across the globe. Donor generosity takes action through the patient care efforts, breakthrough research and innovative medical education and training programs led by Northwestern Medicine’s finest. We are proud to share just a few examples of that generosity in action here. p.2 p.5 p.8 p.11 Polsky Family Creates a Urologic Cancer The Davee Foundation—47 Years of Giving IDP Foundation Fellowship Boosts Vision Newman Family Scholarship Promotes Institute to Transform How Urologic Builds a Legacy to Last a Lifetime for Future of Ophthalmology Primary Care Path for MD Graduates Cancers are Treated p.3 p.6 p.9 p.12 Chez Professorship Raises Bar in Myeloma Richard A. Bernstein Distinguished Physician Lurain Fellowship Supports -

219 Health Network • Chicago, IL
219 Health Network • Chicago, IL Adventist Midwest Health • Hinsdale, IL Advocate Illinois Masonic Medical Center • Chicago, IL Advocate Sherman Hospital • Elgin, IL Albanna Neuro Surgical Consultants • St. Louis, MO Albert Einstein Hospital Lubin Rehabilitation Ctr. • Bronx, NY Algemeen Ziekenhuis de Tjongerschans • Amsterdam & Heerenveen, NLD Alliance Health, Inc. • Edmond, OK Alliance of Free Democrat • Budapest, HUN Allied Health Services, Inc. • Scranton, PA Ambulatory & Community Health Network of Cook Cnty. • Chicago, IL Ambulatory Hospitals of America • Houston, TX Ambulatory SurgiCtr. of Downers Grove • Downers Grove, IL American Baptist Homes of the Midwest • Encinitas, CA Amgen International • Lucerne, CHE Amita Health Adventist Bolingbrook Hospital • Bolingbrook, IL Amita Health Adventist Glen Oaks Hospital • Glendale Heights, IL Amita Health Adventist Hinsdale Hospital • Hinsdale, IL Amita Health Adventist La Grange Memorial Hospital • La Grange, IL Anne Arundel Health System • Annapolis, MD Apostolic Christian Restmor, Inc. • Morton, IL Appalachian Regional Health • Lexington, KY Arete Healthcare • San Antonio, TX AS Realty Investors • Culver City, CA Ardent Health Services • Nashville, TN & Tulsa, OK ARTEMIS Law Firm • Scottsdale, AZ Aspen Medical Ventures, Inc. • Basalt, CO Aultman Hospital • Canton, OH Aurora Health System • Milwaukee, WI Avamere Health Services • Wilsonville, OR Balance Institute of Indiana • Indianapolis, IN Baptist Beaumont Hospital – Beaumont/Orange • Beaumont, TX Baptist Health La Grange • LaGrange, KY Baptist Health System • Little Rock, AR Baptist Health System • San Antonio, TX Baptist Memorial Hospital • Memphis, TN Baptist Memorial Rehab Hospital • New Orleans, LA Baptist St. Anthony’s Health System • Amarillo, TX Barnes-Jewish Hospital • St. Louis, MO Baycare Health System • Clearwater, New Port Richey & St. Petersburg, FL 1 BayCare St. Joseph’s Children’s Hospital • Tampa, FL BayHealth Medical Ctr. -

2017 Strategic Plan: Medicaid Behavioral Health Delivery & Payment System Reform
2017 STRATEGIC PLAN: Medicaid Behavioral Health Delivery & Payment System Reform CURRENT SITUATION Medicaid is the single largest payer for behavioral health services in the United States, and spending for individuals with a behavioral health diagnosis can be 2.5 to 3.5 times higher than for beneficiaries without a behavioral health diagnosis.1 Throughout Illinois, 74 counties lack inpatient mental health beds within their hospitals, necessitating strong collaboration and communication to ensure patients receive care at the right time and in the right setting.2 Moreover, community-based crisis care and outpatient services are chronically underfunded, exacerbating behavioral health conditions and resulting in overuse or improper use of hospital emergency departments (EDs) to treat these patients. As Illinois has shifted greater than 60% of Medicaid enrollees from fee-for- service to managed care since 2011, a commensurate shift to successfully integrate behavioral healthcare management and streamline care coordination has not occurred. Health systems and community-based behavioral health providers have voiced frustration over excessive delays in claims processing, lengthy and time-consuming authorizations, unreasonable or unexplained denials, a lack of responsiveness from managed care organizations (MCOs), difficulty in credentialing staff, and payment delays. Furthermore, greater than one-third of our state remains in non-mandatory managed care areas that continue to depend on a disjointed system that has not received a rate increase in several years. These stressors on our behavioral healthcare safety net led the Illinois Health and Hospital Association (IHA) to develop overarching guidance to transform the Medicaid behavioral healthcare delivery and payment system for our membership, legislators, insurers, consumers and other healthcare stakeholders. -

Illinois Seif-Insured Parent Companies Abbott Laboratories ABF Freight System, Inc
Illinois SeIf-Insured Parent Companies Abbott Laboratories ABF Freight System, Inc. ABM Onsite Services - Midwest Accurate Personnel, LLC Adventist Midwest Health Advocate Health and Hospitals Corporation AEP Generating Company Aldi Inc. Alternative Staffing, Inc. Alton Steel, Inc. Ameren Services Company Archer Daniels Midland Company Ascension Health Alliance Asplundh Tree Expert Co. A. Finkl & Sons Co. A.S.G. Staffing, Inc. Baxalta Incorporated Baxter International Inc. Bethany Methodist Corporation BJC Health System Blessing Corporate Services, Inc. Boston Window Cleaning, Inc. Brewster Cheese Company Carl Buddig & Company Carle Foundation, The Cassens Transport Company Caterpillar Inc. Catholic Bishop of Chicago, The Catholic Diocese of Rockford Centegra Health System Children's Hospital of Chicago Medical Center Christy-Foltz, Inc. Clifford-Jacobs Forging Company CNH Industrial America LLC Commonwealth Edison Company Consol Energy Inc. Continental Tire the Americas, LLC Costco Wholesale Corporation Covenant Ministries of Benevolence Danville Metal Stamping Company, Inc. Dart Container Corporation of California Dart Container Corporation of Illinois Decatur Memorial Hospital Deere & Company Denk & Roche Builders DG Retail, LLC Dierbergs Markets, Inc. Diocese of Springfield in Illinois Edsal Manufacturing Company, Inc. Edward-Elmhurst Healthcare Elite Labor Services, Ltd. dba Elite Staffing, Inc. Empire Comfort Systems, Inc. Estwing Manufacturing Company, Inc. Etnyre International, Ltd. Export Packaging Co., Inc. E.I. Du Pont De Nemours & Company Fairmount Minerals, LLC FCA US LLC Federal Warehouse Company FedEx Freight, Inc. FedEx Ground Package System, Inc. Fiberteq, LLC Ford Motor Company Franciscan Health Olympia Fields & Chicago Heights Franciscan Sisiters of Chicago Service Corporation Gateway Region Young Men's Christian Association General Motors LLC Genesis Health System, an Illinois Not For Profit Corporation Gerresheimer Glass Inc. -

Hospitals We Serve
Hospitals We Serve Illinois Cook County Kindred Hospital – Northlake Campus DeKalb County AMITA Health Alexian Brothers Medical Little Company of Mary Hospital and Kindred Hospital – Sycamore Center – Elk Grove Village Health Care Centers Northwestern Kishwaukee Hospital AMITA Health Alexian Brothers Loretto Hospital Northwestern Valley West Hospital Rehabilitation Hospital – Mount Sinai Hospital Elk Grove Village Northwest Community Hospital AMITA Health Adventist Medical DuPage County Center – Hinsdale Northwestern Memorial Hospital AMITA Health Adventist Medical Center AMITA Health Alexian Brothers Women & Northwestern Prentice Women’s Hospital Children’s Hospital – Hoffman Estates Edward Hospital & Health Services Norwegian American Hospital AMITA Health St. Alexius Medical Center – Elmhurst Memorial Hospital Palos Community Hospital Hoffman Estates Northwestern Central DuPage Hospital AMITA Health Adventist Medical Center Presence Holy Family Medical Center – LaGrange Presence Saint Francis Hospital Grundy County Community First Medical Center – Evanston Morris Hospital Edward Hines Jr. VA Hospital Presence Saint Joseph Hospital – Chicago Franciscan St. James Health – Presence Saints Mary and Elizabeth Chicago Heights Medical Center – Saint Elizabeth Campus Kane County Franciscan St. James Health – Presence Saints Mary and Elizabeth Northwestern Delnor Hospital Olympia Fields Medical Center – Saint Mary Campus Presence Mercy Center Holy Cross Hospital Presence Resurrection Medical Center Presence St. Joseph Hospital Ingalls Memorial -

Fss Internship & Volunteering Site Booklet 2019-2020
********************************************************************************* FSS INTERNSHIP & VOLUNTEERING SITE BOOKLET 2019-2020 Family Social Services School of Family and Consumer Sciences Northern Illinois University Primary criteria for an acceptable site is (must contain all listed below): 1. Established agency operating with at least nine months programming each year, 2. Agency directed by a professional with at least a bachelor's degree and three years of related experience, 3. Experiences provided the intern which are comparable to a position held by a staff employee with a bachelor's degree as the desired educational preparation, or Master's, if a 4. Direct supervisor of intern should hold at least a bachelor's degree with at least one year of relevant experience, 5. The direct supervisor desires assignment of an intern. NOTE: Although we make every effort to keep addresses and telephone numbers up to date, students should check this information before using it. REMEMBER, All Work Done Through Internship/Volunteering Possible Intern/Volunteer Sites for HDFS 431 MUST BE FSS RELATED WORK!! Listing Includes: 1. Site name, address, city, state, zip If a site is NOT listed as an Internship-ready (Affiliated) site, 2. Agency contact person you may NOT use it for your INTERNSHIP 3. Phone and/or email address (when available) UNTIL AN AFFILIATION AGREEMENT HAS BEEN COMPLETED. Sites Where Interns Have Been Placed Note: Detailed "Intern Job Descriptions" for sites listed below are located in file boxes in Wirtz 118. Please ask at the front desk. ~~~ Please DO NOT contact any agency person listed without first having received instructions from your faculty intern coordinator, unless the call is merely to arrange a visit to see the site and NOT TO discuss about "can I personally intern here?" ~~~~ SEE "INTERN JOB DESCRIPTIONS" FOR DETAILED DUTIES, PREREQUISITE INFORMATION, AND RECOMMENDED ELECTIVES.