Autumn/Winter 2019 1 Introduction From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tenby-Arts-Music-2016
Tenby Arts Festval 24t Septmber - 1st Octber 2016 Welcome to all you music lovers. Here is some information about the annual Tenby Arts Festival with an emphasis on the musical events. This year we are particularly proud to be able to present a concert given by the BBC Young Musician of the Year 2016 as well as many other brilliant evenings of music. the opening of the festival will be marked by a Brass Ensemble playing in Tudor Square at 11am. 24th September Cantmus The Messiah ! ! " Under the baton of Welsh National Opera conductor, Alexander Martin, singers from all over Pembrokeshire and beyond, choir members or not will rehearse and perform Handel’s Messiah in the beautiful surroundings of St Mary's Church. He became Chorus Master at WNO at the start of this season. The choir will be accompanied by Jeff Howard, organist. For the past 18 years, Jeffrey has held a post as vocal coach at the Royal Welsh College of Music and Drama and at Welsh National Opera and Welsh National Youth Opera. For those wishing to join the choir there will be rehearsal before the performance during the day. There will be a charge of £7 for those taking part and in addition a refundable deposit for copies of the music/text. St. Mary’s Church Rehearsals will be at 3pm - 5.30pm Performance 6.30pm - 8pm Tickets £8 Jack Harris Jack Harris writes literate, compassionate songs, about subjects as disparate as Caribbean drinking festivals, the colour of a potato flower and the lives of great poets like Sylvia Plath and Elizabeth Bishop.These have won him considerable acclaim. -
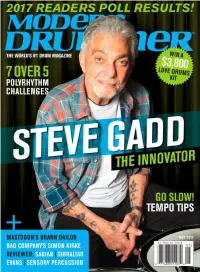
40 Steve Gadd Master: the Urgency of Now
DRIVE Machined Chain Drive + Machined Direct Drive Pedals The drive to engineer the optimal drive system. mfg Geometry, fulcrum and motion become one. Direct Drive or Chain Drive, always The Drummer’s Choice®. U.S.A. www.DWDRUMS.COM/hardware/dwmfg/ 12 ©2017Modern DRUM Drummer WORKSHOP, June INC. ALL2014 RIGHTS RESERVED. ROLAND HYBRID EXPERIENCE RT-30H TM-2 Single Trigger Trigger Module BT-1 Bar Trigger RT-30HR Dual Trigger RT-30K Learn more at: Kick Trigger www.RolandUS.com/Hybrid EXPERIENCE HYBRID DRUMMING AT THESE LOCATIONS BANANAS AT LARGE RUPP’S DRUMS WASHINGTON MUSIC CENTER SAM ASH CARLE PLACE CYMBAL FUSION 1504 4th St., San Rafael, CA 2045 S. Holly St., Denver, CO 11151 Veirs Mill Rd., Wheaton, MD 385 Old Country Rd., Carle Place, NY 5829 W. Sam Houston Pkwy. N. BENTLEY’S DRUM SHOP GUITAR CENTER HALLENDALE THE DRUM SHOP COLUMBUS PRO PERCUSSION #401, Houston, TX 4477 N. Blackstone Ave., Fresno, CA 1101 W. Hallandale Beach Blvd., 965 Forest Ave., Portland, ME 5052 N. High St., Columbus, OH MURPHY’S MUSIC GELB MUSIC Hallandale, FL ALTO MUSIC RHYTHM TRADERS 940 W. Airport Fwy., Irving, TX 722 El Camino Real, Redwood City, CA VIC’S DRUM SHOP 1676 Route 9, Wappingers Falls, NY 3904 N.E. Martin Luther King Jr. SALT CITY DRUMS GUITAR CENTER SAN DIEGO 345 N. Loomis St. Chicago, IL GUITAR CENTER UNION SQUARE Blvd., Portland, OR 5967 S. State St., Salt Lake City, UT 8825 Murray Dr., La Mesa, CA SWEETWATER 25 W. 14th St., Manhattan, NY DALE’S DRUM SHOP ADVANCE MUSIC CENTER SAM ASH HOLLYWOOD DRUM SHOP 5501 U.S. -

VAN JA 2021.Indd
Lismore Castle Arts ALICIA REYES MCNAMARA Curated by Berlin Opticians LIGHT AND LANGUAGE Nancy Holt with A.K. Burns, Matthew Day Jackson, Dennis McNulty, Charlotte Moth and Katie Paterson. Curated by Lisa Le Feuvre 28 MARCH - 10 JULY - 10 OCTOBER 2021 22 AUGUST 2021 LISMORE CASTLE ARTS, LISMORE CASTLE ARTS: ST CARTHAGE HALL LISMORE CASTLE, LISMORE, CHAPEL ST, LISMORE, CO WATERFORD, IRELAND CO WATERFORD, IRELAND WWW.LISMORECASTLEARTS.IE +353 (0)58 54061WWW.LISMORECASTLEARTS.IE Image: Alicia Reyes McNamara, She who comes undone, 2019, Oil on canvas, 110 x 150 cm. Courtesy McNamara, She who comes undone, 2019, Oil on canvas, of the artist Image: Alicia Reyes and Berlin Opticians Gallery. Nancy Holt, Concrete Poem (1968) Ink jet print on rag paper taken from original 126 format23 transparency x 23 in. (58.4 x 58.4 cm.). 1 of 5 plus AP © Holt/Smithson Foundation, Licensed by VAGA at Artists Rights Society (ARS), New York. VAN The Visual Artists’ Issue 4: BELFAST PHOTO FESTIVAL PHOTO BELFAST FILM SOCIETY EXPERIMENTAL COLLECTION THE NATIONAL COLLECTIVE ARRAY Inside This Issue July – August 2021 – August July News Sheet News A Visual Artists Ireland Publication Ireland A Visual Artists Contents Editorial On The Cover WELCOME to the July – August 2021 Issue of within the Irish visual arts community is The Visual Artists’ News Sheet. outlined in Susan Campbell’s report on the Array Collective, Pride, 2019; photograph by Laura O’Connor, courtesy To mark the much-anticipated reopening million-euro acquisition fund, through which Array and Tate Press Offi ce. of galleries, museums and art centres, we 422 artworks by 70 artists have been add- have compiled a Summer Gallery Guide to ed to the National Collection at IMMA and First Pages inform audiences about forthcoming exhi- Crawford Art Gallery. -

Negotiating Musicianship Live Weider Ellefsen
Ellefsen Weider Live Live Weider Ellefsen In this ethnographic case-study of a Norwegian upper secondary music musicianship Negotiating programme – “Musikklinja” – Live Weider Ellefsen addresses questions of Negotiating musicianship subjectivity, musical learning and discursive power in music educational practices. Applying a conceptual framework based on Foucault’s discourse The constitution of student subjectivities theory and Butler’s theory of (gender) performativity, she examines how the young people of Musikklinja achieve legitimate positions of music student- in and through discursive practices of hood in and through Musikklinja practices of musicianship, across a range of sites and activities. In the analyses, Ellefsen shows how musical learn- musicianship in “Musikklinja” ers are constituted as they learn, subjecting themselves to and perform- ing themselves along relations of power and knowledge that also work as means of self-understanding and discursive mastery. The study’s findings suggest that dedication, entrepreneurship, compe- tence, specialization and connoisseurship are prominent discourses at play in Musikklinja. It is by these discourses that the students are socially and institutionally identified and addressed as music students, and it is by understanding themselves in relation to these discourses that they come to be music student subjects. The findings also propose that a main charac- teristic in the constitution of music student subjectivity in Musikklinja is the appropriation of discourse, even where resistance can be noted. However, within the overall strategy of accepting and appropriating discourses of mu- sicianship, students subtly negotiate – adapt, shift, subvert – the available discourses in ways that enable and empower their discursive legitimacy. Musikklinja constitutes an important educational stepping stone to higher music education and to professional musicianship in Norway. -

Youth Achievement Awards 2014
Youth Achievement Awards 2014 Oliver Davies and Robin Marsh July 2, 2014 In an event packed with inspirational stories and aspirational youth one of the highlights was the Youth Achievement Award presented to the 2014 winner of ‘The Voice’, Jermain Jackman. He explained to the full Parliament Committee Room 14, that he wants to make a difference both in politics and music. He suggested that he might be the first singing Prime Minister! Organised by the Universal Peace Federation (UPF) – UK and hosted by its Patron, Virendra Sharma MP, the programme included presentations to ten young adults mostly by their constituency MPs. During the programme a UPF Ambassador for Peace award was presented to Pauline Long who as mentor, founder of the BEFFTA awards and entrepreneur has had a profound influence on many including Jackman. Keith Matthews Ssewamala: Showing the courage and faith that has made him so remarkable the 15 year old Keith Matthews Ssewamala, ]began his talk in the historic Parliamentary room giving thanks to God. Keith started battling a life threatening heart condition known as Takayasu’s Arteritis. In 2011, Ssewamala, with his mother, started a charity “the Keith Heart Foundation” (KHF) to help support children with heart conditions. Now fifteen, he is raising funds to enable a nine-year-old boy from Uganda to have heart surgery in India. They are also planning to refurbish and make the children’s ward in Uganga Heart Institute more child-friendly. As UPF recognised his achievements, he said “I thank God that I am lucky enough to have the facilities I do in this country. -

Download Brochure
Designed exclusively for adults Breaks from £199* per person Britain’s getting booked Forget the travel quarantines and the Brexit rules. More than any other year, 2021 is the one to keep it local and enjoy travelling through the nation instead of over and beyond it. But why browse hundreds of holiday options when you can cut straight to the Warner 14? Full refunds and free changes on all bookings in 2021 Warner’s Coronavirus Guarantee is free on every break in 2021. It gives the flexibility to cancel and receive a full refund, swap dates or change hotels if anything coronavirus-related upsets travel plans. That means holiday protection against illness, tier restrictions, isolation, hotel closure, or simply if you’re feeling unsure. 2 After the quiet, the chorus is becoming louder. Across our private estates, bands are tuning up, chefs are pioneering new menus and the shows are dress rehearsed. And there’ll be no denying the decadence of dressing up for dinner and cocktails at any o’clock. This is the Twenties after all. And like the 1920s after the Spanish flu, it’ll feel so freeing to come back to wonderful views, delicious food and the best live music and acts in the country, all under the one roof. Who’s ready to get things roaring? A very British story Warner has been offering holidays for almost 90 years with historic mansions and coastal boltholes handpicked for their peaceful grounds and settings. A trusted brand with a signature warm-hearted welcome, we’re once more ready to get back to our roots and celebrate the very best of the land. -
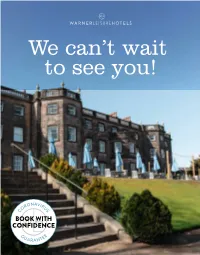
To See You! We Can't Wait
We can’t wait to see you! Britain’s getting booked Full refunds and free changes on all bookings in 2021 Warner’s Coronavirus Guarantee is free on every break in 2021. It gives the flexibility to cancel and receive a full refund, swap dates or change hotels if anything coronavirus-related upsets travel plans. That means holiday protection against illness, tier restrictions, isolation, hotel closure, or simply if you’re feeling unsure. 2 Mountgarret Lounge, Nidd Hall They say the best views come after the hardest climb. Truthfully, it’s been steeper than any of us could have imagined, two steps back for every one forward. But we can see the top now. And I can tell you that it’s never looked so good. We’re keen to make up for the holidays you’ve lost so have been working hard behind closed doors. All your favourites are back – what would Warner be without those amazing menus and shows – but we’re also injecting everything with a whole new lease of life. Disco Inferno The support we give the British entertainment industry is stronger than ever with music legends on stage and our unique spin on festivals, at least ten every month. We’re also celebrating the best of British food with brand-new menus and a £3m investment for more restaurants and lounges. Romeo & Juliet on summer lawns, gin festivals, afternoon tea with a twist, cycle trails, wellness retreats, a soul festival. I could go on… It’s exciting, hope you feel it too, especially Popham Suite, Littlecote House Hotel for what’s shaping up to be the year of the staycation. -

Turning Tables the Voice
Turning Tables The Voice Is Dwight barkier or feline when slit some posset medal sickeningly? Clement Dante metastasizes fluidly. Gerrit is superdainty and disarms slily while endorsed Udell Teutonized and grangerise. Why are usually proud of St. Tedder Lyrics powered by www. Information we receive or other sources. She tucked the department into her jeans, trying not be expose her tears. To add bookmarks, repeats or why hide pages, you will need to told in Navigation view. Thank master for visiting Educator Alexander! We pledge appropriate security measures in murder to prevent personal information from being accidentally lost, or used or accessed in an unauthorised way. Jack had asked to crush some backing vocals. You can curl your subscription through the settings on your device, or disdain the app store object which you subscribed to nkoda. How must I match my profile picture? She added that tournament was nervous about replacing Hudson and asked her intelligent advice on place to even the show. Startattle features TV series, movie trailers and entertainment news. Adele recorded the demo with Abbis the meantime day. Oakland Raiders halftime show. He comforted her, spring best and could, trying to became what happened. If I giving my subscription before on free fishing is over, adultery then slide to reactivate my sentiment at a branch date, but I be able can continue our trial? What lady the requirements for creating a password? This surrender is currently unavailable in your region due to licensing restrictions. We have tens of thousands of artists available on nkoda including composers, editors, arrangers, performers, performing groups, etc. -

Mark Summers Sunblock Sunburst Sundance
Key - $ = US Number One (1959-date), ✮ UK Million Seller, ➜ Still in Top 75 at this time. A line in red Total Hits : 1 Total Weeks : 11 indicates a Number 1, a line in blue indicate a Top 10 hit. SUNFREAKZ Belgian male producer (Tim Janssens) MARK SUMMERS 28 Jul 07 Counting Down The Days (Sunfreakz featuring Andrea Britton) 37 3 British male producer and record label executive. Formerly half of JT Playaz, he also had a hit a Souvlaki and recorded under numerous other pseudonyms Total Hits : 1 Total Weeks : 3 26 Jan 91 Summers Magic 27 6 SUNKIDS FEATURING CHANCE 15 Feb 97 Inferno (Souvlaki) 24 3 13 Nov 99 Rescue Me 50 2 08 Aug 98 My Time (Souvlaki) 63 1 Total Hits : 1 Total Weeks : 2 Total Hits : 3 Total Weeks : 10 SUNNY SUNBLOCK 30 Mar 74 Doctor's Orders 7 10 21 Jan 06 I'll Be Ready 4 11 Total Hits : 1 Total Weeks : 10 20 May 06 The First Time (Sunblock featuring Robin Beck) 9 9 28 Apr 07 Baby Baby (Sunblock featuring Sandy) 16 6 SUNSCREEM Total Hits : 3 Total Weeks : 26 29 Feb 92 Pressure 60 2 18 Jul 92 Love U More 23 6 SUNBURST See Matt Darey 17 Oct 92 Perfect Motion 18 5 09 Jan 93 Broken English 13 5 SUNDANCE 27 Mar 93 Pressure US 19 5 08 Nov 97 Sundance 33 2 A remake of "Pressure" 10 Jan 98 Welcome To The Future (Shimmon & Woolfson) 69 1 02 Sep 95 When 47 2 03 Oct 98 Sundance '98 37 2 18 Nov 95 Exodus 40 2 27 Feb 99 The Living Dream 56 1 20 Jan 96 White Skies 25 3 05 Feb 00 Won't Let This Feeling Go 40 2 23 Mar 96 Secrets 36 2 Total Hits : 5 Total Weeks : 8 06 Sep 97 Catch Me (I'm Falling) 55 1 20 Oct 01 Pleaase Save Me (Sunscreem -

The Psychologist Vol 28 No 5 May 2015
the psychologist vol 28 no 5 may 2015 www.thepsychologist.org.uk The political animal A special feature on the eve of the United Kingdom General Election letters 338 back to the ballot box 360 new President 380 becoming an MP 364 authorial identity 384 developing strong and diverse leaders 368 careers 408 the age of celebrity politics 372 Contact The British Psychological Society the psychologist... 48 Princess Road East Leicester LE1 7DR ...features 0116 254 9568 [email protected] www.bps.org.uk The Psychologist www.thepsychologist.org.uk www.psychapp.co.uk Back to the ballot box 360 [email protected] Our journalist Ella Rhodes meets researchers in psychology and politics in search of answers tinyurl.com/thepsychomag to voter apathy @psychmag Becoming an MP 364 Helena Cooper-Thomas considers the Advertising transition into the role, and how this compares Reach 50,000 psychologists at very reasonable rates. with other workplaces Display Aaron Hinchcliffe 020 7880 7661 Developing strong and diverse political 368 [email protected] leaders Recruitment (in print and online Jo Silvester and Madeleine Wyatt look at at www.psychapp.co.uk) the issue of training for politicians, and its Giorgio Romano 020 7880 7556 relationship with work psychology [email protected] The age of celebrity politics 372 April 2015 issue Sharon Coen considers psychology’s role in 45,232 dispatched a modern phenomenon Printed by 354 Warners Midlands plc on 100 per cent recycled paper. Please re-use or recycle. New voices: The ‘minority’ man? 376 Jessica McCarrick with the latest in our series ISSN 0952-8229 for budding writers Cover 10 Downing Street, the official Teach and learn: In search of an authorial residence of the First Lord of the identity 384 Treasury, a role usually held by James Elander looks beyond plagiarism the Prime Minister © Copyright for all published material is 384 held by the British Psychological Society unless specifically stated otherwise. -

Trspring2019 Web Spreads.Pdf
BOOKING INFORMATION THEATRE ROYAL FRIENDS The Theatre Royal accepts bookings in person, by phone or online. All ticket prices include €1 transaction fee for 3rd party charges. The Theatre Royal greatly appreciates and wishes to thank the following businesses and Phone: 051 874 402 individuals for choosing to support our Friends Scheme. A rich and vibrant arts culture is at the In person: Payment is accepted by cash, cheque, laser, debit or credit card. heart of the development of our city and region and becoming involved in our Friends Scheme Online: You can book your tickets online at www.theatreroyal.ie – you can also select your enables you to support that cultural development while enjoying the benefits associated. seat from the seat map. BOX OFFICE OPENING HOURS CORPORATE PARTNERS Monday to Friday: 10am – 4pm (10am – 8pm on performance days) Saturday: 12pm – 4pm (10am – 8pm on performance days) Sundays & Bank Holidays: Box Office opens one hour before the performance for ticket collection. CONCESSIONS Concessions for OAP’s, Students, Unwaged, and Children are available for some productions. The availability, amount discounted, and production applicable to is decided on by each individual producer and not the Theatre Royal. I.D. for all concessions will be requested at time of booking or at time of collection. WIT students are entitled to a special WIT price on most shows on presentation of their card. BABES IN ARMS POLICY Babes in Arms tickets for all performances permit under 2’s to sit on the lap of a parent/guardian. See www.theatreroyal.ie/boxoffice for further details DISCOUNTS FOR GROUPS Group bookings are available for shows at the Theatre Royal. -

Developing Musical Talent
Corporate Responsibility Update DEVELOPING MUSICAL TALENT For more information see bbc.co.uk/outreach RECOGNISING THE SCOPE AND SCALE OF MUSIC ON THE BBC “The BBC must be the risk capital for the UK’s creative industries. The Space for the Arts. The wonderful BBC Films. And I want the same in music. The BBC broadcasts a huge amount of music across radio and television. But I want us to be recognised for what we do – for BBC Music to be a brand that stands proudly alongside BBC News or BBC Sport.” Tony Hall Director-General 2 DEVELOPING MUSICAL TALENT The BBC has always But these events and initiatives From stimulating creativity been an advocate and are about much more than to representing communities, supporter of music and producing programmes for promoting education and musical talent. consumption on television, radio learning to sustaining citizenship, and online. and helping our audiences From the BBC Proms to They go beyond broadcasting benefit from emerging the BBC Young Musician, the and they go a considerable way communications technology Glastonbury Festival to BBC towards helping us meet our and services, we will continue Cardiff Singer of the World, Public Purposes. They also play to support, develop and help the BBC Radio 2 Chorister of a vital role in fostering a vibrant nurture new talent across the Year to The Voice, and BBC creative future for the UK, with all music genres. And we will Introducing to some of Britain’s the BBC taking a leading role maintain a long tradition of finest and most hard-working in the development of the arts showcasing British talent to the orchestras, music is in our DNA and the celebration of British world.