Novel Inborn Error of Vitamin B12 Metabolism Caused by Mutations in ABCD4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Figure 1
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2012 Mutations in ABCD4 cause a new inborn error of vitamin B(12) metabolism Coelho, David ; Kim, Jaeseung C ; Miousse, Isabelle R ; Fung, Stephen ; du Moulin, Marcel ; Buers, Insa ; Suormala, Terttu ; Burda, Patricie ; Frapolli, Michele ; Stucki, Martin ; Nürnberg, Peter ; Thiele, Holger ; Robenek, Horst ; Höhne, Wolfgang ; Longo, Nicola ; Pasquali, Marzia ; Mengel, Eugen ; Watkins, David ; Shoubridge, Eric A ; Majewski, Jacek ; Rosenblatt, David S ; Fowler, Brian ; Rutsch, Frank ; Baumgartner, Matthias R Abstract: Inherited disorders of vitamin B(12) (cobalamin) have provided important clues to how this vitamin, which is essential for hematological and neurological function, is transported and metabolized. We describe a new disease that results in failure to release vitamin B(12) from lysosomes, which mimics the cblF defect caused by LMBRD1 mutations. Using microcell-mediated chromosome transfer and exome sequencing, we identified causal mutations in ABCD4, a gene that codes for an ABC transporter, which was previously thought to have peroxisomal localization and function. Our results show that ABCD4 colocalizes with the lysosomal proteins LAMP1 and LMBD1, the latter of which is deficient in the cblF defect. Furthermore, we show that mutations altering the putative ATPase domain of ABCD4 affect its function, suggesting that the ATPase activity of ABCD4 may be involved in intracellular processing of vitamin B(12). -

Germline Mutations Causing Familial Lung Cancer
Journal of Human Genetics (2015) 60, 597–603 & 2015 The Japan Society of Human Genetics All rights reserved 1434-5161/15 www.nature.com/jhg ORIGINAL ARTICLE Germline mutations causing familial lung cancer Koichi Tomoshige1,2, Keitaro Matsumoto1, Tomoshi Tsuchiya1, Masahiro Oikawa1, Takuro Miyazaki1, Naoya Yamasaki1, Hiroyuki Mishima2, Akira Kinoshita2, Toru Kubo3, Kiyoyasu Fukushima3, Koh-ichiro Yoshiura2 and Takeshi Nagayasu1 Genetic factors are important in lung cancer, but as most lung cancers are sporadic, little is known about inherited genetic factors. We identified a three-generation family with suspected autosomal dominant inherited lung cancer susceptibility. Sixteen individuals in the family had lung cancer. To identify the gene(s) that cause lung cancer in this pedigree, we extracted DNA from the peripheral blood of three individuals and from the blood of one cancer-free control family member and performed whole-exome sequencing. We identified 41 alterations in 40 genes in all affected family members but not in the unaffected member. These were considered candidate mutations for familial lung cancer. Next, to identify somatic mutations and/or inherited alterations in these 40 genes among sporadic lung cancers, we performed exon target enrichment sequencing using 192 samples from sporadic lung cancer patients. We detected somatic ‘candidate’ mutations in multiple sporadic lung cancer samples; MAST1, CENPE, CACNB2 and LCT were the most promising candidate genes. In addition, the MAST1 gene was located in a putative cancer-linked locus in the pedigree. Our data suggest that several genes act as oncogenic drivers in this family, and that MAST1 is most likely to cause lung cancer. -

New Tests 2 Test Updates 4 CPT Code Updates 11 Deleted Tests 11 Diagnostics Update Volume XXI, No
Volume XXI, No. 6 JUNE 2021 MONTHLY TEST UPDATES Diagnostics Update New Tests 2 Test Updates 4 CPT Code Updates 11 Deleted Tests 11 Diagnostics Update Volume XXI, No. 6 | JUNE 2021 New Tests Use Anti-DFS70 antibodies may help identify individuals who do not have an Anti-Carbamylated Protein (CarP) Antibody 520311 ANA-associated Autoimmune Rheumatic Disease (AARD) especially in the absence of significant clinical findings.1 Anti-DFS70 Ab, especially when positive CPT 83516 in isolation (i.e. in the absence of AARD-associated autoantibodies), may Synonyms Anti-CarP antigen antibody; RA marker prevent unnecessary referrals and examinations of ANA-positive individuals.2 Special Instructions This test has not been approved for NY state clients. Limitations This test should be used with clinical findings and other Specimen Serum autoimmune testing; it cannot be used alone to rule out autoimmune disease. Volume 1 mL This test was developed and its performance characteristics determined Minimum Volume 0.5 mL by Labcorp. It has not been cleared or approved by the Food and Drug Container Red-top tube; serum from red-top tube; serum from a gel tube; or Administration. serum gel tube Methodology Enzyme-linked immunosorbent assay (ELISA) Collection Separate serum from cells within one hour of collection. Transfer to a Additional Information Anti-DFS70 antibodies target the dense fine speckled plastic transport tube before shipping. protein of 70 kDa which is identical to Lens Epithelium-Derived Growth Factor Storage Instructions Refrigerate or freeze. or transcription co-activator p75 (LEDGFp75). They are detectable in 2% to 22% Stability of healthy individuals and in less than 1% of patients with AARD are of unknown Temperature Period clinical significance. -
An Update on Vitamin B12-Related Gene Polymorphisms and B12 Status
An update on vitamin B12-related gene polymorphisms and B12 status. Article Published Version Creative Commons: Attribution 4.0 (CC-BY) Open Access Surendran, S., Adaikalakoteswari, A., Saravanan, P., Shatwaan, I. A., Lovegrove, J. A. and Vimaleswaran, K. S. (2018) An update on vitamin B12-related gene polymorphisms and B12 status. Genes & Nutrition, 13 (1). pp. 1555-8932. ISSN 1865-3499 doi: https://doi.org/10.1186/s12263-018- 0591-9 Available at http://centaur.reading.ac.uk/75711/ It is advisable to refer to the publisher’s version if you intend to cite from the work. See Guidance on citing . To link to this article DOI: http://dx.doi.org/10.1186/s12263-018-0591-9 Publisher: Springer All outputs in CentAUR are protected by Intellectual Property Rights law, including copyright law. Copyright and IPR is retained by the creators or other copyright holders. Terms and conditions for use of this material are defined in the End User Agreement . www.reading.ac.uk/centaur CentAUR Central Archive at the University of Reading Reading’s research outputs online Surendran et al. Genes & Nutrition (2018) 13:2 DOI 10.1186/s12263-018-0591-9 REVIEW Open Access An update on vitamin B12-related gene polymorphisms and B12 status S. Surendran1, A. Adaikalakoteswari2,3, P. Saravanan2,3, I. A. Shatwaan1, J. A. Lovegrove1 and K. S. Vimaleswaran1* Abstract Background: Vitamin B12 is an essential micronutrient in humans needed for health maintenance. Deficiency of vitamin B12 has been linked to dietary, environmental and genetic factors. Evidence for the genetic basis of vitamin B12 status is poorly understood. -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Downloaded from the App Store and Nucleobase, Nucleotide and Nucleic Acid Metabolism 7 Google Play
Hoytema van Konijnenburg et al. Orphanet J Rare Dis (2021) 16:170 https://doi.org/10.1186/s13023-021-01727-2 REVIEW Open Access Treatable inherited metabolic disorders causing intellectual disability: 2021 review and digital app Eva M. M. Hoytema van Konijnenburg1†, Saskia B. Wortmann2,3,4†, Marina J. Koelewijn2, Laura A. Tseng1,4, Roderick Houben6, Sylvia Stöckler‑Ipsiroglu5, Carlos R. Ferreira7 and Clara D. M. van Karnebeek1,2,4,8* Abstract Background: The Treatable ID App was created in 2012 as digital tool to improve early recognition and intervention for treatable inherited metabolic disorders (IMDs) presenting with global developmental delay and intellectual disabil‑ ity (collectively ‘treatable IDs’). Our aim is to update the 2012 review on treatable IDs and App to capture the advances made in the identifcation of new IMDs along with increased pathophysiological insights catalyzing therapeutic development and implementation. Methods: Two independent reviewers queried PubMed, OMIM and Orphanet databases to reassess all previously included disorders and therapies and to identify all reports on Treatable IDs published between 2012 and 2021. These were included if listed in the International Classifcation of IMDs (ICIMD) and presenting with ID as a major feature, and if published evidence for a therapeutic intervention improving ID primary and/or secondary outcomes is avail‑ able. Data on clinical symptoms, diagnostic testing, treatment strategies, efects on outcomes, and evidence levels were extracted and evaluated by the reviewers and external experts. The generated knowledge was translated into a diagnostic algorithm and updated version of the App with novel features. Results: Our review identifed 116 treatable IDs (139 genes), of which 44 newly identifed, belonging to 17 ICIMD categories. -
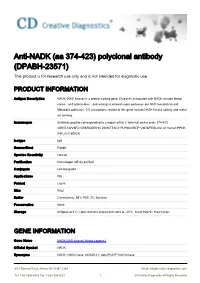
Anti-NADK (Aa 374-423) Polyclonal Antibody (DPABH-23571) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-NADK (aa 374-423) polyclonal antibody (DPABH-23571) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description NADK (NAD kinase) is a protein-coding gene. Diseases associated with NADK include dental caries , and tuberculosis , and among its related super-pathways are NAD metabolism and Metabolic pathways. GO annotations related to this gene include NAD+ kinase activity and metal ion binding. Immunogen Synthetic peptide corresponding to a region within C terminal amino acids 374-423 (ARNTAWVSFD GRKRQEIRHG DSISITTSCY PLPSICVRDP VSDWFESLAQ) of Human PPNK (NP_001185924) Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB Format Liquid Size 50 μl Buffer Constituents: 98% PBS, 2% Sucrose Preservative None Storage Shipped at 4°C. Upon delivery aliquot and store at -20°C. Avoid freeze / thaw cycles. GENE INFORMATION Gene Name NADK NAD kinase [ Homo sapiens ] Official Symbol NADK Synonyms NADK; NAD kinase; dJ283E3.1; poly(P)/ATP NAD kinase; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Entrez Gene ID 65220 Protein Refseq NP_001185922.1 UniProt ID A0A024R058 Pathway Defective AMN causes hereditary megaloblastic anemia 1; Defective CD320 causes methylmalonic aciduria; Defective GIF causes intrinsic factor deficiency; Defective LMBRD1 causes methylmalonic aciduria and homocystinuria type cblF Function ATP binding; NAD+ kinase activity; NAD+ kinase activity; metal ion binding 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

Selection Signatures Scan in Several Italian Sheep Breeds Identifies Genes Influencing Micronutrient Metabolism S
Selection signatures scan in several Italian sheep breeds identifies genes influencing micronutrient metabolism S. Sorbolini1, C. Dimauro1, M. Cellesi1, F. Pilla2, N.P.P. Macciotta1 and the BIOVITA Consortium. 1Università di Sassari, Dipartimento di Agraria, Viale Italia 39, 07100 Sassari, Italy. 1Università del Studi del Molise, Dipartimento Agricoltura Ambiente Alimenti, Via F. de Sanctis s.n.c. 86100 Campobasso, Italy. [email protected] (Corresponding author) Summary Animal physiological functions involve enzymes and cofactors. Many of these substances can not be synthesized by the body, but derive from the diet. An example are micronutrients, that strongly affect production performance, whose requirements are often met by the farmers by adding supplements to the diet. The aim of this study was to investigate the genetic variability of Italian sheep breeds searching for possible selective sweeps that harbor genes involved in the metabolism of micronutrients in. SNP A sample of 496 sheep belonging to 20 breeds farmed in Italy were genotyped with the Illumina Ovine 50K beadchip. Data were analysed by canonical discriminant analysis (CDA). Forty SNP located in regions of the genome containing loci involved in the metabolism of vitamins and minerals were detected. in particular, genes linked to the metabolism of vitamins and minerals such as Selenocysteine Lyase (SCLY), calcium sensing receptor (CASR), Solute Carrier Family 23 Member 1 (SLC23A1) and Thiamine Triphosphatase (THTPA) were highlighted. Keywords: selection signatures, micronutrients, sheep, Canonical Discriminant Analysis Introduction Nutritional status is of particular importance for productive performances in livestock. Growth, milk production, reproduction depend on a wide range of essential nutrients such as amino acids, fatty acids, vitamins and minerals. -

Modeling Regulatory Network Topology Improves Genome-Wide
bioRxiv preprint doi: https://doi.org/10.1101/2020.03.13.990010; this version posted March 14, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. LAST EDITED ON 2020-03-12 BY X.Z. 1 MODELING REGULATORY NETWORK TOPOLOGY IMPROVES 2 GENOME-WIDE ANALYSES OF COMPLEX HUMAN TRAITS 3 BY XIANG ZHU AND ZHANA DUREN AND WING HUNG WONG 4 Stanford University 5 Genome-wide association studies (GWAS) have cataloged many sig- 6 nificant associations between genetic variants and complex traits. How- 7 ever, most of these findings have unclear biological significance, because 8 they often have small effects and occur in non-coding regions. Integra- 9 tion of GWAS with gene regulatory networks addresses both issues by 10 aggregating weak genetic signals within regulatory programs. Here we 11 develop a Bayesian framework that integrates GWAS summary statis- 12 tics with regulatory networks to infer enrichments and associations si- 13 multaneously. Our method improves upon existing approaches by ex- 14 plicitly modeling network topology to assess enrichments, and by au- 15 tomatically leveraging enrichments to identify associations. Applying 16 this method to 18 human traits and 38 regulatory networks shows that 17 genetic signals of complex traits are often enriched in networks spe- 18 cific to trait-relevant tissue or cell types. Prioritizing variants within 19 enriched networks identifies known and new trait-associated genes re- 20 vealing novel biological and therapeutic insights. -

Downloaded Per Proteome Cohort Via the Web- Site Links of Table 1, Also Providing Information on the Deposited Spectral Datasets
www.nature.com/scientificreports OPEN Assessment of a complete and classifed platelet proteome from genome‑wide transcripts of human platelets and megakaryocytes covering platelet functions Jingnan Huang1,2*, Frauke Swieringa1,2,9, Fiorella A. Solari2,9, Isabella Provenzale1, Luigi Grassi3, Ilaria De Simone1, Constance C. F. M. J. Baaten1,4, Rachel Cavill5, Albert Sickmann2,6,7,9, Mattia Frontini3,8,9 & Johan W. M. Heemskerk1,9* Novel platelet and megakaryocyte transcriptome analysis allows prediction of the full or theoretical proteome of a representative human platelet. Here, we integrated the established platelet proteomes from six cohorts of healthy subjects, encompassing 5.2 k proteins, with two novel genome‑wide transcriptomes (57.8 k mRNAs). For 14.8 k protein‑coding transcripts, we assigned the proteins to 21 UniProt‑based classes, based on their preferential intracellular localization and presumed function. This classifed transcriptome‑proteome profle of platelets revealed: (i) Absence of 37.2 k genome‑ wide transcripts. (ii) High quantitative similarity of platelet and megakaryocyte transcriptomes (R = 0.75) for 14.8 k protein‑coding genes, but not for 3.8 k RNA genes or 1.9 k pseudogenes (R = 0.43–0.54), suggesting redistribution of mRNAs upon platelet shedding from megakaryocytes. (iii) Copy numbers of 3.5 k proteins that were restricted in size by the corresponding transcript levels (iv) Near complete coverage of identifed proteins in the relevant transcriptome (log2fpkm > 0.20) except for plasma‑derived secretory proteins, pointing to adhesion and uptake of such proteins. (v) Underrepresentation in the identifed proteome of nuclear‑related, membrane and signaling proteins, as well proteins with low‑level transcripts. -

Genetic Analysis of 400 Patients Refines Understanding And
BASIC RESEARCH www.jasn.org Genetic Analysis of 400 Patients Refines Understanding and Implicates a New Gene in Atypical Hemolytic Uremic Syndrome Fengxiao Bu,1,2 Yuzhou Zhang,2 Kai Wang,3 Nicolo Ghiringhelli Borsa,2 Michael B. Jones,2 Amanda O. Taylor,2 Erika Takanami,2 Nicole C. Meyer,2 Kathy Frees,2 Christie P. Thomas,4 Carla Nester,2,4,5 and Richard J.H. Smith2,4,5 1Medical Genetics Center, Southwest Hospital, Chongqing, China; and 2Molecular Otolaryngology and Renal Research Laboratories, 3College of Public Health, 4Division of Nephrology, Department of Internal Medicine, Carver College of Medicine, and 5Department of Pediatrics, Carver College of Medicine, University of Iowa, Iowa City, Iowa ABSTRACT Background Genetic variation in complement genes is a predisposing factor for atypical hemolytic uremic syndrome (aHUS), a life-threatening thrombotic microangiopathy, however interpreting the effects of genetic variants is challenging and often ambiguous. Methods We analyzed 93 complement and coagulation genes in 400 patients with aHUS, using as controls 600 healthy individuals from Iowa and 63,345 non-Finnish European individuals from the Genome Aggre- gation Database. After adjusting for population stratification, we then applied the Fisher exact, modified Poisson exact, and optimal unified sequence kernel association tests to assess gene-based variant burden. We also applied a sliding-window analysis to define the frequency range over which variant burden was significant. Results We found that patients with aHUS are enriched for ultrarare coding variants in the CFH, C3, CD46, CFI, DGKE,andVTN genes. The majority of the significance is contributed by variants with a minor allele frequency of ,0.1%. -

Content Based Search in Gene Expression Databases and a Meta-Analysis of Host Responses to Infection
Content Based Search in Gene Expression Databases and a Meta-analysis of Host Responses to Infection A Thesis Submitted to the Faculty of Drexel University by Francis X. Bell in partial fulfillment of the requirements for the degree of Doctor of Philosophy November 2015 c Copyright 2015 Francis X. Bell. All Rights Reserved. ii Acknowledgments I would like to acknowledge and thank my advisor, Dr. Ahmet Sacan. Without his advice, support, and patience I would not have been able to accomplish all that I have. I would also like to thank my committee members and the Biomed Faculty that have guided me. I would like to give a special thanks for the members of the bioinformatics lab, in particular the members of the Sacan lab: Rehman Qureshi, Daisy Heng Yang, April Chunyu Zhao, and Yiqian Zhou. Thank you for creating a pleasant and friendly environment in the lab. I give the members of my family my sincerest gratitude for all that they have done for me. I cannot begin to repay my parents for their sacrifices. I am eternally grateful for everything they have done. The support of my sisters and their encouragement gave me the strength to persevere to the end. iii Table of Contents LIST OF TABLES.......................................................................... vii LIST OF FIGURES ........................................................................ xiv ABSTRACT ................................................................................ xvii 1. A BRIEF INTRODUCTION TO GENE EXPRESSION............................. 1 1.1 Central Dogma of Molecular Biology........................................... 1 1.1.1 Basic Transfers .......................................................... 1 1.1.2 Uncommon Transfers ................................................... 3 1.2 Gene Expression ................................................................. 4 1.2.1 Estimating Gene Expression ............................................ 4 1.2.2 DNA Microarrays ......................................................