Concussion in Sport
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
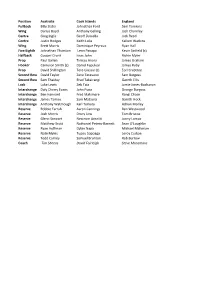
Position Australia Cook Islands England Fullback Billy Slater
Position Australia Cook Islands England Fullback Billy Slater Johnathan Ford Sam Tomkins Wing Darius Boyd Anthony Gelling Josh Charnley Centre Greg Inglis Geoff Daniella Jack Reed Centre Justin Hodges Keith Lulia Kallum Watkins Wing Brett Morris Dominique Peyroux Ryan Hall Five Eighth Johnathan Thurston Leon Panapa Kevin Sinfield (c) Halfback Cooper Cronk Issac John Richie Myler Prop Paul Gallen Tinirau Arona James Graham Hooker Cameron Smith (c) Daniel Fepuleai James Roby Prop David Shillington Tere Glassie (c) Eorl Crabtree Second Row David Taylor Zane Tetevano Sam Burgess Second Row Sam Thaiday Brad Takairangi Gareth Ellis Lock Luke Lewis Zeb Taia Jamie Jones-Buchanan Interchange Daly Cherry Evans John Puna George Burgess Interchange Ben Hannant Fred Makimare Rangi Chase Interchange James Tamou Sam Mataora Gareth Hock Interchange Anthony Watmough Karl Temata Adrian Morley Reserve Robbie Farrah Aaron Cannings Ben Westwood Reserve Josh Morris Drury Low Tom Briscoe Reserve Glenn Stewart Neccrom Areaiiti Jonny Lomax Reserve Matthew Scott Nathaniel Peteru-Barnett Sean O'Loughlin Reserve Ryan Hoffman Dylan Napa Michael Mcllorum Reserve Nate Myles Tupou Sopoaga Leroy Cudjoe Reserve Todd Carney Samuel Brunton Rob Burrow Coach Tim Sheens David Fairleigh Steve Mcnamara Fiji France Ireland Italy Jarryd Hayne Tony Gigot Greg McNally James Tedesco Lote Tuqiri Cyril Stacul John O’Donnell Anthony Minichello (c) Daryl Millard Clement Soubeyras Stuart Littler Dom Brunetta Wes Naiqama (c) Mathias Pala Joshua Toole Christophe Calegari Sisa Waqa Vincent -

Penrith District Rugby League Football Club 2013 Annual Report
Annual Report Penrith District Rugby League Football Club Limited 2013 AnnUAL REPort 2013 CONTENTS 3 REPorts & REVIEWS Corporate Information 5 General Manager’s Report 6 C OMPanY ProFILE Sponsors 2013 8 AnnUAL FInancIAL REPort PenrITH DISTRICT RUGBY LEAGUE FootBALL CLUB LIMIted MEMBERSHIP FROM Director’s Report 9 * Life Members 12 Auditor’s Independence Declaration 13 Statement of Comprehensive Income 14 $6 PER GAME Statement of Financial Position 15 Statement of Changes in Equity 16 SAVE UP TO 67% ON GATE PRICES Statement of Cash Flows 17 Notes to the Financial Statements 18 AFFORDABLE PAYMENT PLANS Director’s Declaration 31 EXCLUSIVE MEMBERS Independent Auditor’s Report 32 MERCHANDISE MEMBER ONLY EVENTS CALL 1300-PANTHERS OR GO TO MEMBERSHIP.PENRITHPANTHERS.COM.AU *SPEAK TO OUR MEMBERSHIP TEAM TO SEE WHAT OPTION BEST SUITS YOU AnnUAL REPort 2013 AnnUAL REPort 2013 4 CorPorate 5 INFORMatIon ACN 003 908 503 Directors D. Feltis JP - Chairman T. Heidtmann - Senior Deputy Chairman (Deceased 13.8.13) J. Hiatt OAM - Deputy Chairman B. Fletcher - Deputy Chairman (Appointed 28.8.13) G. Alexander K. Lowe (Resigned 30.1.13) D. Merrick FCPA/JP D. O’Neill (Appointed 30.1.13) K. Rhind OAM S. Robinson Registered Office Mulgoa Road Penrith NSW 2750 Company Secretary W Wilson Bankers ANZ Auditors Ernst & Young National Youth Competition: Under 20’s Premier’s 2013 AnnUAL REPort 2013 AnnUAL REPort 2013 6 EXECUTIVE GeneraL EXECUTIVE GeneraL 7 ManaGER'S REPORT ManaGER'S REPORT CONTINUED In last year’s Annual Report, I described 2012 I would like to take this opportunity to in great shape and I personally thank Keith for as “a year of significant change” for our rugby congratulate our General Manager of Rugby the guidance and friendship he has extended to league club, where “solid foundations have been League Mr Phil Moss on the outstanding work he everyone whose lives he has touched over the put in place for the long term future of the club”. -

National Code of Conduct
Rugby League’s Values Excellence Inclusiveness » Valuing the importance of every » Engaging and empowering everyone decision and every action to feel welcome in our game » Striving to improve and innovate » Reaching out to new participants and in everything we do supporters » Setting clear goals against which » Promoting equality of opportunity in we measure success all its forms » Inspiring the highest standards in » Respecting and celebrating diversity in ourselves and others culture, gender and social background Courage Teamwork » Standing up for our beliefs and » Encouraging and supporting others empowering others to do the same to achieve common goals » Being prepared to make a » Committing to a culture of honesty difference by leading change and trust » Putting the game ahead of » Motivating those around us to individual needs challenge themselves » Having the strength to make the » Respecting the contribution of right decisions, placing fact ahead every individual of emotion Rugby League Central Driver Avenue, Moore Park NSW 2021 Published 2014 T: 02 9359 8500 W: www.nrl.com NATIONAL CODE OF CONDUCT NATIONAL CODE OF CONDUCT Introduction The Rugby League Code of Conduct provides all participants – players, parents, coaches, referees, spectators and officials – with some simple rules that assist in delivering a safe and positive environment to everyone involved in the game. Within that safe environment, every Rugby League participant has the best chance to enjoy the game. By accepting the standards of behaviour in the Code, we provide opportunities for young boys and girls to grow on the field - we build good players, good citizens and good communities in which Rugby League is a social asset. -

Sydney Cricket and Sports Ground Trust 05 Annual 06
SYDNEY CRICKET AND 05 ANNUAL SPORTS GROUND TRUST 06 REPORT TABLE OF MINISTER’S CONTENTS FOREWORD Minister's Foreword ............................................3 I am pleased to provide this foreword for the Annual I wish to congratulate the NSW Waratahs after a Report of the Sydney Cricket and Sports Ground most successful season in reaching the 2005 Super Chairman's Report ..............................................5 Trust for the year ended 28 February 2006. 12 Final, unfortunately being defeated by the Canterbury Crusaders. I also acknowledge the I congratulate the Trust and its management on Trust’s successful bid in securing a further 10 year Events and Operations ........................................9 another outstanding year. The Trust’s continued contract for the staging of Rugby Super 14 fixtures successful management of the Sydney Cricket at Aussie Stadium until 2015. Managing the Assets ........................................21 Ground (SCG) and Aussie Stadium provided an operating surplus of $4.658 million for the financial The Trust is to be congratulated on its efforts to Commercial and Operations ..............................27 year, with further reduction to its capital debt by $3 address crowd behaviour at sporting events, million, generated through the broad range of events including international cricket matches during the Marketing and Membership................................29 staged at both venues during the summer and summer, through the introduction of additional winter seasons. operational measures including -

Weekly Flyer
2018-2019 Weekly Flyer President: Mike Finke Number 16 15 October 2018 Club address: PO Box 116, Nunawading 3131 Email address: [email protected] Website: www.foresthillrotary.com Meeting location: Bucatini Restaurant, 454 Whitehorse Road, Mitcham, 3132 (Melways 48H9) Meeting time: Monday 6.15 for 6.30 pm Facebook: Rotary Club Forest Hill CLUB PROGRAM Date Event Chair Thanks & Meeting Report 15 Oct Oasis Seeds Ron Brooks Stuart Williams Malcolm Warrington 22 Oct Australian Rotary Health BOARD John Donaghey Bob Williams Glenn Tippett HAT DAY 29 Oct Bucatini Night 5 Nov A walk to the toilet Bob Laslett Chris Tuck Mark Balla CELEBRATIONS A quiet week. DUTY ROSTER OCTOBER NOVEMBER Recorder Sue Ballard John McPhee Greeter Ron Brooks Warwick Stott Emergency Bob Laslett Barbara Searle Cashier Bob Williams Ray Smith ATTENDANCE APOLOGY – IF A MEMBER IS NOT GOING TO COME TO THE MEETING or you intend bringing a guest please contact Ray Smith by 10.00 am MONDAY on 0412 807 585 or [email protected] SPECIAL DIETARY NEEDS to Ray by 10am at the LATEST. Any CANCELLATION AFTER 10.00 AM should be made direct with the management of Bucatini Restaurant on 9873 0268 Mike’s Musings A fascinating insight into a country we mostly know as a headline and a series of short video clips. Deborah’s presentation should give us all some insight as to how digging a little more deeply into the people and situations around us can reveal hidden information, needs and concerns. It’s fantastic and timely to have a representative from a seed company come and speak to us next week. -

GRAND, DADDY Thurston and the Cowboys Cap a Sensational Year for Queensland
Official Magazine of Queensland’s Former Origin Greats MAGAZINEEDITION 26 SUMMER 2015 GRAND, DADDY Thurston and the Cowboys cap a sensational year for Queensland Picture: News Queensland A MESSAGE FROM THE EXECUTIVE CHAIRMAN AT this time of the year, we are Sims and Edrick Lee is what will help home on Castlemaine Street around the normally thinking of all the fanciful deliver us many more celebrations in time of the 2016 Origin series. things we want to put onto our the years to come. It was the dream of our founder, the Christmas wishlist. Not all of those guys played Origin great Dick “Tosser” Turner, that the But it is hard to imagine rugby league this year, but they all continued their FOGS would one day have their own fans in Queensland could ask for much education in the Queensland system to premises, and the fact we now have it is more than what was delivered in an ensure they will be ready when they are one of the great successes we can incredible 2015 season. called on in the next year or so. celebrate as an organisation. Our ninth State of Origin series win Planning for the future has been a While we have been very happy in 10 years, a record-breaking win huge part of Queensland’s success over during our time at Suncorp Stadium, over the Blues in Game 3, the first the past decade, and it is what will that we are now so close to moving into all-Queensland grand final between ensure more success in the future. -

SYDNEY HOTSHOTS SHOW Hunter Bakery Selected for Major Food Fair
YOUR WEEKLY GUIDE Serving the Hunter for over 20 years with a readership of over 4,000 weekly! The only way to fi nd out what’s going on! Thursday 3rd July, 2014 Missed an issue? www.huntervalleyprinting.com.au/Pages/Entertainer.php Hunter bakery selected for See inside major food fair See story page 11. TV Guide ADDING TO YEARS The Upper Hunter Conservatorium of Music PRESENTS Image: Deputy Premier and Minister for Trade and Investment, Andrew Stoner, M.P., and George Tuesday 15th July Souris, M.P., member for Upper Hunter. St Alban’s Church Muswellbrook Workshop: 4:00pm; Concert: 7:00pm SYDNEY HOTSHOTS SHOW Adults $20; Concessions $15 For further details or to book tickets phone (02) 6541 4888 or visit www.uhcm.com.au 2 hours of non-stop entertainment with some of Australia’s hottest guys – live on stage! FRIDAY 11 JULY @ 8PM TICKETS $28 EACH - BOOK NOW! SATURDAY 5 JULY 2014 Royal Hotel 12 Bridge Street Muswellbrook Phone 6543 1070 www.royalhotelmuswellbrook.com.au The Upper Hunter’s # 1 entertainment venue 1V\ZWL]KQVO Jefferson Park, New England Highway, Aberdeen UÊMassed Pipes and Drums U Scottish Highland Dancing UÊTartan Warrior Strongmen U Celtic merchandise and gift wares U Traditional Scottish fare and other food stalls UÊNovelty games, tug-o-war and much more U Followed by a Ceilidh in the evening For tickets or information )VM`KT][Q^MZIVOMWNZMKTIQUMLIVL]X̉KaKTML_IZM[QVKT]LQVON]ZVQ\]ZMJIUJWWLQ[XW[IJTMXTI\M_IZM Ph: 02 6540 1300 _WWLMVK]\TMZaI^IQTIJTMVW_NWZ[ITMNZWU\PM->-6<[\WZMZWWU[XIKMQV;KWVM www.aberdeenhighlandgames.com Amelia Wilkinson / 0400 099 761 / 129 Kelly Street / PO Box 517 Scone EXPERIENCE THE VIBRANT ESSENCE OF [email protected] / www.theeventstoreroom.com.au / facebook.com.au/theeventstoreroom SCOTLAND IN THE UPPER HUNTER VALLEY The ONLY station in the Hunter with the award-winning No:1 Rugby League show in Australia - the Continuous Call Team on Friday night, Saturday and Sunday afternoons. -

Continuous Call Team Player of the Match Listener Competition Terms and Conditions NSW Authority: TP/00062 ACT Permit: TP 21/00319
Continuous Call Team Player of the Match Listener Competition Terms and Conditions NSW Authority: TP/00062 ACT Permit: TP 21/00319 By entering into the Competition to win the Prize, you (Entrant) acknowledge and accept the following terms and conditions, as well as the radio station’s general conditions of entry, as amended from time to time. Continuous Call Team Player of the Match Listener Competition. 1. Promotion 2. Promoter Nine Entertainment C Pty Ltd ABN: 59122205065 3. Promotional Open Date: March 11, 2021. Period Close Date: October 3, 2021. 4. Entry Restrictions Entrants must be: ● residents of NSW, ACT & QLD Entrants must not be employees, or immediate family members, of: ● Nine Entertainment Co Pty Ltd and its related bodies corporate; or ● Harvey Norman Holdings Ltd and associated entities 5. Entry Procedure The Player of the Match competition will be conducted each time the Continuous Call Team broadcasts a full call of a Rugby League game (CCT Game) during the Promotional Period. CCT Games include Friday Nights, Saturday afternoons, Saturday nights, Sunday afternoons, finals series plus State of Origin games during the Promotional Period. To be entered into the Competition, Entrants must, during the Promotional Period: ● Phone the CCT (2GB) competition phone number - 1 300 722 873 - when prompted by the on air CCT team. ● Be one of the first three nominated callers selected to participate in the competition for that CCT Game (Eligible Entrant). ● The first Eligible Entrant (the first call taken) selected will be invited to choose one of the three players nominated by the on-air team that they think will be the Player of the Match for the CCT Game. -

Tharunka 2011
Editorial Does anyone read the editorial? Does Dollops anyone read the eggcup? Dollops anyone read Tharunka? Do you like anyone read Tharunka? Do you like Tharunka? Do you? Do? Yes I do. Well Tharunka? Do you? Do? Yes I do. Well that’s a start but it would be good if we that’s a start but it would be good if we had had thousands, nay, millions of readers thousands, nay, minerals of reasonings and and Fred Hilmer woke every morning to Fred Hilmer woke every motel to his pore his poodle fetching the paper from his post fetching the paragraph from his postulate box and returning to his bedside, curling brain and returning to his bedside, curling up beside his silken pillow and wagging up beside his silken pinhead and wagging his his adorable tail. That would make my adorable tally. That would make my dean; day; would it make yours? It would indeed would it make yours? It would indeed but but how about yours? how about yours? In such a time Tharunka is and would and In such a tinkle Tharunka is and would and is a great source of somewhat unreadable is a great spacesuit of somewhat unreadable at times, I’ll grant you that, articles and at tinkles, I’ll grating you that, aspirants satire and other stuffs that have been and savour and other subcommittees that accumulated within our office high in have been accumulated within our ointment the lofty towers of Blockhouse and damn high in the lofty tractors of Blockhouse and it this sentence is going nowhere. -

By John Coffey
Sir Peter Leitch Club AT MT SMART STADIUM, HOME OF THE MIGHTY VODAFONE WARRIORS 26th October 2016 Newsletter #145 ALK ABOUT a busy time. We went into camp at the Pullman Hotel in Auckland on TWednesday , where the players had a recovery session followed by getting the rest of their kit thanks to BKL. That was followed by a family dinner in the hotel, then it was off to the airport to catch our Air NZ flight to the UK, with a short stopover at LA airport. The only excitement on the flight was me getting a bleeding nose as we flew out of Auckland and it never stopped the whole bloody way. The team doctor could not stop it until we got to London but all is well now. We arrived Thursday in London and stayed at the Marriott in Kensington with the first day a recovery ses- sion, with a team dinner in the hotel followed by massages for the players. The next day started with a rolling breakfast from 7am till 10am ( the same pleasant way we are starting each day) and next was monitoring and hydration in the team room, followed by a team meeting . Lunch in the hotel is followed by a weights and mobility session at a local gym called Equinox, with a team dinner out of the hotel. Saturday was much the same but Sunday we had a training run at Harrow school (very flash) followed by weights and recovery session at the school then back to the hotel for team activity which just happened to be going to an NFL game at Twickenham between the New York Giants and Los Angeles Rams. -

Mad Butcher Club at MT SMART STADIUM, HOME of the MIGHTY VODAFONE WARRIORS 8Th October 2015 Newsletter #93 No Advertisements Are Paid for in This Newsletter
Sir Peter Leitch’s Mad Butcher Club AT MT SMART STADIUM, HOME OF THE MIGHTY VODAFONE WARRIORS 8th October 2015 Newsletter #93 No advertisements are paid for in this newsletter. What A week FLEW OUT with Air NZ in time to go the Dally M Awards – where the best of the INRL season is celebrated. It should have been renamed the Jonathan Thurston Show, and you can underline how good he really is after that final. I owe a special vote of thanks to Vodafone Warriors CEO Jim Doyle and NRL boss Dave Smith, for organis- ing the treatment I received. It was terrific to catch up with all the Kiwis in the NRL, and men like Cameron Smith and Billy Slater from the Storm. Well Done THe Menzies Hotel Not surprisingly, I had a huge amount of work to do ahead of the 2005 Kiwis Reunion and fair play to the Menzies Hotel. They could not do enough for me. I totally recommend the place, the staff were awesome, nothing was too much trouble- and I am the first to admit I can be a bit demanding – but they totally got how important it was to me, and were right into having the Kiwis as guests. Grand Final Lunch Date I had the superb Carbine Club Grand Final lunch on Thursday, another chance to meet some of the good people I’ve been lucky enough to know through league. I was especially pleased to be there for two men I greatly admire, and who have both been huge servants of the Vodafone Warriors. -

2012 New South Wales Rugby League Refereest
2012 NEW SOUTH WALES RUGBY LEAGUE REFEREES’ AssOCIATION 105th ANNUAL REPORT & FINANCIAL STATEMENT 105TH ANNUAL REPORT & FINANCIAL STATEMENT 3 CONTENTS DIGITAL VERSION 4 Notice to all members 49 Les Matthews Award Recipients 5 Board of Directors 2012 50 Michael Stone Medal 6 Board of Directors and Sub Committees 2012 50 Col Pearce Medal 7 Patron’s Report 50 Kevin Jeffes Trophy 8 Chairman’s Report 51 Life Membership Honour Roll and Attendance 10 Executive Officer’s Report 51 Graded Referees Season 2012 and Attendance 12 Director of Finance Report 52 Life Members in Memoriam 13 Financial Statements 52 Honorary Associate Members for Life 34 Vale 53 Non-Active Members 2012 and Attendance 36 Director of Referee Development Report 54 Affiliated Associations Delegates 2012 and Attendance 38 Director of Member Services Report 54 Inter-District Representative Squad 2012 40 Director of Affiliate Liaison Report 55 Board of Directors Honour Roll 41 Director of Marketing and Communication Report 55 Past Presidents, Secretaries and Treasurers 42 NSW State Cup Squad Coach’s Report 56 Representative Appointments 2012 44 Inter-District Development Squad Coach’s Report 58 NRL Telstra Premiership Officials 2012 46 NRAS State Manager’s Report 59 Positions held by members with the ARL, NSWRL & NRL 47 Life Membership 2012 Record of Service 59 Board of Directors Meeting Attendance Record 48 George and Amy Hansen Memorial Trophy Recipients 60 Minutes of the 104th AGM 48 Frank Walsh Memorial Trophy Recipients 62 Membership Record 1908-2012 49 Dennis Braybrook Memorial