Safety and Efficacy of Convalescent Plasma to Treat Severe COVID-19: Protocol for the Saudi Collaborative Multicenter Phase II Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Country City Sitename Street Name Saudi Arabia Jeddah Arabian Solutions - Saudi Arabia Barom Center Saudi Arabia Jeddah Arabian Solutions Hial St
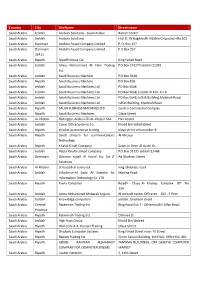
Country City SiteName Street name Saudi Arabia Jeddah Arabian Solutions - Saudi Arabia Barom Center Saudi Arabia Jeddah Arabian Solutions Hial St. W.Bogddadih AlZabin Cmpound villa 102 Saudi Arabia Damman Abdulla Fouad Company Limited P. O. Box 257 Saudi Arabia Dammam Abdulla Fouad Company Limited P O Box 257 31411 Saudi Arabia Riyadh Riyadh House Est. King Fahad Road Saudi Arabia Jeddah Idress Mohammed Ali Fatni Trading P.O.Box 132270 Jeddah 21382 Est. Saudi Arabia Jeddah Saudi Business Machine P.O.Box 5648 Saudi Arabia Riyadh Saudi Business Machine P.O Box 818 Saudi Arabia Jeddah Saudi Business Machines Ltd PO Box 5648 Saudi Arabia Jeddah Saudi Business Machines Ltd. PO Box 5648, Jeddah 21432, K S A Saudi Arabia Jeddah Saudi Business Machines Ltd. PO Box 5648, Juffali Building,Madinah Road Saudi Arabia Jeddah Saudi Business Machines Ltd. Juffali Building, Madinah Road Saudi Arabia Riyadh SAUDI BUSINESS MACHINES LTD. Centria Commercial Complex Saudi Arabia Riyadh Saudi Business Machines Olaya Street Saudi Arabia Al-Khobar Redington Arabia LTD AL-Khobar KSA Hail Center Saudi Arabia Jeddah Canar Office Systems Co Khalid Bin Walid Street Saudi Arabia Riyadh shrakat partnerships trading olaya street villa number 8 Saudi Arabia Riyadh Saudi Unicom for communications Al-Mrouje technology Saudi Arabia Riyadh Khalid Al Safi Company Salah Al-Deen Al-Ayubi St., Saudi Arabia Jeddah Azizia Panda United Company P.O.Box 33333 Jeddah 21448 Saudi Arabia Dammam Othman Yousif Al Yousif Est. for IT Ad Dhahran Street Solutions Saudi Arabia Al Khober al hasoob al asiavy est. king abdulaziz road Saudi Arabia Jeddah EchoServe-Al Sada Al Shamila for Madina Road Information Technology Co. -

Travel Medicine and Infectious Disease 38 (2020) 101901
Travel Medicine and Infectious Disease 38 (2020) 101901 Contents lists available at ScienceDirect Travel Medicine and Infectious Disease journal homepage: www.elsevier.com/locate/tmaid Original article Incidence of COVID-19 among returning travelers in quarantine facilities: A longitudinal study and lessons learned Jaffar A. Al-Tawfiq a,b,c,*, Amar Sattar d, Husain Al-Khadra d, Saeed Al-Qahtani d, Mobarak Al-Mulhim e, Omar Al-Omoush d, Hatim O. Kheir d a Specialty Internal Medicine and Quality Department, Johns Hopkins Aramco Healthcare, Dhahran, Saudi Arabia b Infectious Disease Division, Department of Medicine, Indiana University School of Medicine, Indianapolis, IN, USA c Infectious Disease Division, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, USA d Primary Care Division, Johns Hopkins Aramco Healthcare, Dhahran, Saudi Arabia e King Fahd Specialist Hospital Dammam, Saudi Arabia ARTICLE INFO ABSTRACT Keywords: Introduction: The emergence of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) had resulted SARS-CoV-2 in an unpresented global pandemic. In the initial events, the Kingdom of Saudi Arabia implemented mandatory COVID-19 quarantine of returning travelers in order to contain COVID-19 cases. Quarantine Materials and methods: This is a longitudinal study of the arriving travelers to Quarantine facilities and the Travelers prevalence of positive SARS-CoV-2 as detected by RT-PCR. Results: During the study period, there was a total of 1928 returning travelers with 1273 (66%) males. The age range was 28 days–69 years. Of all the travelers, 23 (1.2%) tested positive for SARS-CoV-2. Of the firstswab, 14/ 1928 (0.7%) tested positive. -

READ Middle East Brief 101 (PDF)
Judith and Sidney Swartz Director and Professor of Politics Repression and Protest in Saudi Arabia Shai Feldman Associate Director Kristina Cherniahivsky Pascal Menoret Charles (Corky) Goodman Professor of Middle East History and Associate Director for Research few months after 9/11, a Saudi prince working in Naghmeh Sohrabi A government declared during an interview: “We, who Senior Fellow studied in the West, are of course in favor of democracy. As a Abdel Monem Said Aly, PhD matter of fact, we are the only true democrats in this country. Goldman Senior Fellow Khalil Shikaki, PhD But if we give people the right to vote, who do you think they’ll elect? The Islamists. It is not that we don’t want to Myra and Robert Kraft Professor 1 of Arab Politics introduce democracy in Arabia—but would it be reasonable?” Eva Bellin Underlying this position is the assumption that Islamists Henry J. Leir Professor of the Economics of the Middle East are enemies of democracy, even if they use democratic Nader Habibi means to come to power. Perhaps unwittingly, however, the Sylvia K. Hassenfeld Professor prince was also acknowledging the Islamists’ legitimacy, of Islamic and Middle Eastern Studies Kanan Makiya as well as the unpopularity of the royal family. The fear of Islamists disrupting Saudi politics has prompted very high Renée and Lester Crown Professor of Modern Middle East Studies levels of repression since the 1979 Iranian revolution and the Pascal Menoret occupation of the Mecca Grand Mosque by an armed Salafi Neubauer Junior Research Fellow group.2 In the past decades, dozens of thousands have been Richard A. -

The Following Lawyers in the Dhahran / Al-Khobar / Dammam Area Have Expressed Interest in Providing Legal Services and Advice to U.S
The following lawyers in the Dhahran / Al-Khobar / Dammam area have expressed interest in providing legal services and advice to U.S. citizens. Law offices are generally open during Saudi working hours of approximately 9:00 a.m. to 1:00 p.m. and 5:00 p.m. to 8:00 p.m. 1. Abdulaziz Alassaf & Partners in association with Shearman & Sterling LLP Firm size: 20 attorneys Mailing Address: P.O. Box 30572, Al-Khobar 31952 Physical Address: : SUMO Tower, 6th Floor, Unit 6140,Prince Turki Street (Corniche), Al- Khobar Phone(s): +966 (01) 3 830 6554 Fax: +966 (01) 3 830 4949 Email: [email protected] Website: http://www.shearman.com/en/offices/saudi-arabia Languages: Arabic, English, French, Russian Law School: Various Saudi and foreign law schools Geographic Area: All provinces Areas of Practice: Employment / Labor Disputes Contract Mergers and acquisitions Private equity Joint ventures Corporate restructuring Capital markets and regulatory advice Company law and corporate governance Structuring foreign investments Formation of Saudi, GCC and foreign owned companies Agency, distribution and franchises Procurement contracts Litigation Arbitration and mediation Risk management Enforcement and debt recovery Regulatory enforcement Alternative dispute resolution Fees: Fixed Rates, Hourly Rates, Contingency depending upon the nature of the case Ex-Pat Clients: Previous representation of Americans and other Westerners Additional: Headquarters in Riyadh, branch offices in Jeddah and Al-Khobar. No criminal matters. 2.Abdulateef Abdalla Ahmed -

Risk Perceptions of Cardiovascular Disease Among Saudi Arabian Women in Relation to Home Cooking and Intentions to Cook Low Fat Meals
RISK PERCEPTIONS OF CARDIOVASCULAR DISEASE AMONG SAUDI ARABIAN WOMEN IN RELATION TO HOME COOKING AND INTENTIONS TO COOK LOW FAT MEALS A dissertation submitted to the Kent State University College of Education, Health, and Human Services in partial fulfillment of the requirements for the degree of Doctor of Philosophy By Nawal Alissa May 2017 © Copyright, 2017 by Nawal Alissa All Rights Reserved ii A dissertation written by Nawal Alissa B.S., King Saud University, 1996 M.P.A., Eastern Washington University, 2001 M.Ed., Kent State University, 2017 Ph.D., Kent State University, 2017 Approved by _____________________________, Co-director, Doctoral Dissertation Committee Dianne Kerr _____________________________, Co-director, Doctoral Dissertation Committee Kele Ding _____________________________, Member, Doctoral Dissertation Committee Kimberly Schimmel Accepted by _____________________________, Director, School of Health Sciences Lynne E. Rowan _____________________________, Interim Dean, College of Education, Health and Mark A. Kretovics Human Services iii ALISSA, NAWAL, Ph.D., May 2017 HEALTH EDUCATION AND PROMOTION RISK PERCEPTIONS OF CARDIOVASCULAR DISEASE AMONG SAUDI ARABIAN WOMEN IN RELATION TO HOME COOKING AND INTENTIONS TO COOK LOW FAT MEALS (178 pp.) Co-Directors of Dissertation: Dianne Kerr, Ph.D. Kele Ding, Ph.D. The purpose of this study was to investigate the risk perceptions and cooking behaviors of Saudi Arabian women in relation to cardiovascular disease (CVD) and intentions to cook low fat meals. Participants were Saudi Arabian women (ages 22-55). Data were collected through self-administered paper-pencil surveys in the summer of 2016. This study was conducted in a primary care clinic’s waiting room in a single hospital (King Khalid University Hospital) providing services to patients mainly from the Riyadh district of Saudi Arabia. -

Economic Development Prospects for the Eastern Province
Economic Development Prospects for the Eastern Province Economic Development Prospects for the Eastern Province www.chamber.org.sa Eastern Province in Brief 02 Section One: 04 Eastern Province’s Key Economic Development Section Two: 06 Industrial Activity in Eastern Province Contents Section Three: 15 Infrastructure Development in Eastern Province Section Four: 18 Tourism Activity in Eastern Province Section Five: 22 Population in Eastern Province Section Six: 24 Work Force in Eastern Province Section Seven: 26 Housing Units in Eastern Province Section Eight: 28 Hospital & Beds in Eastern Province Section Nine: 32 Agriculture & Livestock Resources in Eastern Province Section Ten: 38 Water Production in Eastern Province Conclusion and References 42-45 Eastern Province in Brief ASH SHARQIYAH Eastern Province The Eastern Province of Saudi Arabia is the place where Kingdom’s first oil was extracted in 1938 and subsequently this region has become the center of world-class oil, gas and petrochemical industries with the presence of global giants in these sectors. Today, the Eastern Province is dubbed “The Industrial Capital of the Entire Gulf” for its enormous industrial activities. And it is evident when this region has become the biggest recipient of industrial capital investments of the Kingdom. 22 Economic Development Prospects for the Eastern Province With the support from the recently launched “Saudi Vision 2030”, the Eastern Province has taken a key role in the Kingdom’s drive to diversify its income away from oil. Most of the manufacturing industries such as petrochemicals, chemicals, steel, cement, aluminum and plastics are located in the region. These industries are mainly based in the Dammam-I, II and III industrial estates, Al Ahsa-I and II industrial estates, Hafr Al-Batin industrial estate and Jubail-I and II industrial cities. -

Pediatric Viral Respiratory Infections in Saudi Arabia: Narrative and Descriptive Revisits for the Etiology, Epidemiology and Cl
June 2020 KUWAIT MEDICAL JOURNAL 118 Review Article Pediatric viral respiratory infections in Saudi Arabia: Narrative and descriptive revisits for the etiology, epidemiology and clinical phenotypes with diagnostic challenges highlights Ayed A Shati1, Abdelwahid S Ali2, Ahmed M Al-Hakami2, Ali A Asseri1, Saleh M Al-Qahatani1 1Department of Child Health, College of Medicine, King Khalid University, Abha, Saudi Arabia 2Department of Microbiology and Clinical Parasitology, College of Medicine, King Khalid University, Abha, Saudi Arabia Kuwait Medical Journal 2020; 52 (2): 118 - 128 ABSTRACT Objective: To review, describe and narrate the etiology, Up to 2019, 35 studies were published in the topic. The epidemiology and clinical phenotypes of pediatric viral highest number of reports was for respiratory syncytial respiratory infections (PVRIs) in Saudi Arabia (KSA) viruses (n=17, 48.6%), while bocaviruses are the least Design: A comprehensive electronic search of the reported viruses (n=3, 8.6%). Clinical presentations literature for PVRIs in KSA reported suggested both upper and lower respiratory Setting:An electronic search in PubMed, SCOPUS, Google tract infections. PVRIs were reported from Riyadh, Al- Scholar and MEDLINE Qassim, Jazan, Jeddah, Dammam, Najran, Taif and Subjects: Articles published up till 2019 and those that Abha. Immunofluorescence assays, enzyme-linked dealt with the detection of viruses from clinical specimens immunosorbent assay, polymerase chain reaction and Interventions: Retrieved articles were subtly studied. Data virus isolation were employed. obtained included the virus reported, year of publication, Conclusion(s): In this review communication, we diagnostics, region or city, research purpose, the season of described the etiology, epidemiology and clinical infection and hospital of admission (if any). -

The Ismailis of Najran RIGHTS Second-Class Saudi Citizens WATCH
Saudi Arabia HUMAN The Ismailis of Najran RIGHTS Second-class Saudi Citizens WATCH The Ismailis of Najran Second-class Saudi Citizens Copyright © 2008 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 1-56432-376-5 Cover design by Rafael Jimenez Human Rights Watch 350 Fifth Avenue, 34th floor New York, NY 10118-3299 USA Tel: +1 212 290 4700, Fax: +1 212 736 1300 [email protected] Poststraße 4-5 10178 Berlin, Germany Tel: +49 30 2593 06-10, Fax: +49 30 2593 0629 [email protected] Avenue des Gaulois, 7 1040 Brussels, Belgium Tel: + 32 (2) 732 2009, Fax: + 32 (2) 732 0471 [email protected] 64-66 Rue de Lausanne 1202 Geneva, Switzerland Tel: +41 22 738 0481, Fax: +41 22 738 1791 [email protected] 2-12 Pentonville Road, 2nd Floor London N1 9HF, UK Tel: +44 20 7713 1995, Fax: +44 20 7713 1800 [email protected] 27 Rue de Lisbonne 75008 Paris, France Tel: +33 (1)43 59 55 35, Fax: +33 (1) 43 59 55 22 [email protected] 1630 Connecticut Avenue, N.W., Suite 500 Washington, DC 20009 USA Tel: +1 202 612 4321, Fax: +1 202 612 4333 [email protected] Web Site Address: http://www.hrw.org September 2008 1-56432-376-5 The Ismailis of Najran Second-class Saudi Citizens I. Summary and Recommendations ..................................................................................... 1 Recommendations to the Saudi Government .................................................................. 4 Methodology .................................................................................................................. 6 II. Background .................................................................................................................... 8 III. Relevant International Standards .................................................................................14 IV. The Clash and Crackdown of April 2000 ....................................................................... 19 Background: The Ministry of Interior plan to shut Ismaili mosques ............................... -

Trade Information of Country Saudi Arab
List of Saudi importers of food products Sl. No.Name of Importer Address Phone/ Fax E-mail/ website 01 A.H. AL Muhanna PO Box: 1945, Tel. 00966-13- Trading & Contracting Dammam 31441 8422969/ 8422454 Est. Fax: 00966-13- 8423221 02 A.K. Almuhaidib & PO Box:30, Tel. 00966-13- [email protected] Sons Dammam 31411 8328888/ 8322033 a Fax: 8336082 03 Abdullehah Ali Athawi PO Box: 4221, Tel. 00966-12- Jeddah 21491 6440219/ 6424508 Fax: 6479398 04 Abdulkarim ElkhreijiPO Box: 276, Tel. 00966-13- ictcs@ace- Group Dammam 31411 8324441 / 8329080 dmm.khereiji.com /8342326 Fax: 8349389 05 Abdullah A. AlPO Box:2395, Tel. 00966-11- [email protected] Munajem Sons Co. Riyadh 11451 4787933 Fax: 4764318 06 Abdullah Abbar &PO Box: 5700, Tel. 00966-12- [email protected] Ahemed Zainy Jeddah -21432 6474000 Fax: 6475542 07 Abdulla Abduljalil Est. PO Box: 5309, Tel. 00966-12- Jeddah -21422 6477092 / 6435175 Fax: 6473375 08 Abdullah AhemdPO Box: 4500, Tel. 00966-12- [email protected] Balubadi Est. Jeddah -21491 6470615/ 6470870 t.sa Fax: 6481728 09 Abdullah Bahkim Est.PO Box: 16538, Tel. 00966-12- bahakim_sat@hotmail for Trade Jeddah -21474 6480993 .com Fax: 6481426 10 Abdullah Balsharaf Est.PO Box: 7748, Tel. 00966-12- [email protected] Jeddah -21472 6482642 Fax: 6479060 11 Abdullah Bin Saeed BinPO Box: 26212 Tel. 00966-11- Shaea Trading &Riyadh 11486 4763138/ 4732231 Contracting Est. Fax: 4763149 12 Abdullah EstablishmentPO Box:7778 Tel. 00966-12- jed.office@messinalin for Trading & Industry Jeddah -21472 6424879/ 6426998/ e.com.sa 6426999 Fax: 6432645 13 Abdulmohsen andPO Box: 884, Tel. -
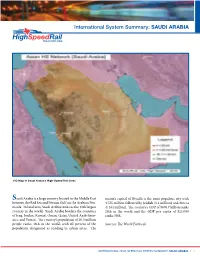
International System Summary: SAUDI ARABIA
International System Summary: SAUDI ARABIA UIC Map of Saudi Arabia’s High-Speed Rail Lines Saudi Arabia is a large country located in the Middle East nation’s capital of Riyadh is the most populous city with between the Red Sea and Persian Gulf on the Arabian Pen- 4.725 million followed by Jeddah (3.2 million) and Mecca insula. In land area, Saudi Arabia ranks as the 13th largest (1.484 million). The country’s GDP of $676.7 billion ranks country in the world. Saudi Arabia borders the countries 24th in the world and the GDP per capita of $24,000 of Iraq, Jordan, Kuwait, Oman, Qatar, United Arab Emir- ranks 55th. ates, and Yemen. The country’s population of 26.5 million people ranks 46th in the world, with 82 percent of the Sources: The World Factbook population designated as residing in urban areas. The INTERNATIONAL HIGH-SPEED RAIL SYSTEM SUMMARY: SAUDI ARABIA | 1 SY STEM DESCRIPTION AND HISTORY The Saudi Railway Master Plan for the period of 2010 to 2040 calls for the strategic development of 19 individual rail lines with a total length of approximately 9,900 km (6,150 miles). These projects are classified into three stages of development, with the first stage covering the years 2010 to 2025; second stage covering the years 2026 to 2033; and the third stage covering the years 2034 to 2040. The first stage projects are considered high-priority and include the following projects according to the Saudi Railways Orga- nization: • The double line upgrade of the existing two conven- tional rail lines between Dammam and Riyadh. -

COMMUNITY CENTER in ALKHOBAR, SAUDI ARABIA By
COMMUNITY CENTER IN ALKHOBAR, SAUDIA ARABIA Item Type text; Master's Project-Reproduction (electronic) Authors ALNAIMI, IBRAHIM MUBARAK Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 29/09/2021 17:45:41 Link to Item http://hdl.handle.net/10150/555261 COMMUNITY CENTER IN ALKHOBAR, SAUDI ARABIA by IBRAHIM MUBARAK ALNAIMI For a A Master's Report Submitted to the Faculty of the COLLEGE OF ARCHITECTURE In Partial Fulfillment of the Requirements For the Degree of MASTER OF ARCHITECTURE 5-1985 Masters Project Committee: Professor Fred S. Matter % atzr Committee Chairman X Professor Kenneth Clark Committee Member Professor Larry Medlin Committee Member HErEhE.iZE ^ liec-e Or ^LZErfEC'rjy.E /rnei-r-/4 - ~ r..>■■ ; w'/ V- .< /Ujif-iJ / y g s a - P ACKN0V7LEDGMENTS This research would not have been possible without the help of God, and the encouragement and advice of the following people. Great thanks and respect are due the committee members: Professors Fred Matter, Kenneth Clark and R. Larry Medlin for their advice, guidance and encouragement. I appreciated their patience and the clarity of their comments. Special thanks are due King Faisal University for the financial support of this research from the early beginnings to the final stage. Great thanks are also due to the Saudi Arabian Educational Mission for their help. Great thanks are due my brother, Mohammed M. -

Addresses of Branches
Addresses of branches Section Neighborhood / street name the phone FAX 012- 012-6768834 1 Jeddah Palestine Street - next to Dallah Tower 2284000 next to the Cooperative Insurance. 2 --------- --------- Rsaifeh Abdullah Arif Street / Al Ahla Mecca Mall The seventh round Unit No.1-2. The second ring / after the towers of 3 Medina the relief - a glass building color Build . 014-8274458 To enter extension dial: 014- 108 8274469 4 Taif University of Taif Faculty of Medicine 012- 727-4438 / Building members 7274 Faculty. 408 5 Dammam Al-Safa neighborhood - King Saud Road - Teacher (Institute) 013-8538800 013-8337907 Marine Technical Studies. Al-Ahsa Al-Mulhim Tower, Al-Thurayat Street. 011- --------- 6 2905555 To enter extension di l Hafr Al Baten - Khalidiya District - 7 Hafr Al-batin King Abdulaziz Street 013-7295516 013-7295517 Versus community college. 8 Qassim Intersection of King Salman Road 016- 016- with Othman bin Affan Road Next 3835042 3835072 to Kairouan Roundabout. 1 Section Neighborhood / street name the phone FAX University of Prince Turki bin 011-2905555 9 Hail Abdulaziz Street To enter 016- 30 (opposite Salamat clinic). extension dial: 5657557 1602 10 Prince Mteeb Bin Abdul Aziz Hospital 014-6242579 To enter Aljawf (Al Sudairi) To enter extension dial - King Saud Road - old plan district Next to the extension 104 Emirate of Al-Jouf.. dial 103- Tabuk Muroj Al Amir District, Behind Al 11 Mahareb Supermarket, 014- 014-4281054 In the same building drugstore 4297038 To enter extension dial 104 12 Abha New Abha / next to Abha Palace 017- 017-2261106 Hotel. 2261 To enter 106 extension dial 106 13 Al-Bahah Al Hayya neighborhood - Prince Sultan bin Abdulaziz Street Behind Samba 017-7247460 017-7247462 Bank from the west.