Research Article Sickle Cell Anemia Patients in Use Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fetal and Embryonic Haemoglobins P
Review Article J Med Genet: first published as 10.1136/jmg.10.1.50 on 1 March 1973. Downloaded from Journal of Medical Genetics (1973). 10, 50. Fetal and Embryonic Haemoglobins P. A. LORKIN MRC Abnormal Haemoglobin Unit, University Department of Biochemistry, Cambridge Haemoglobin has been the subject of intensive form a nearly spherical molecule with extensive research for many years and is one of the most areas of contact between unlike chains; the two thoroughly understood of all protein molecules. main types of contact are denoted alp, and alg2 The amino-acid sequences of haemoglobins from The tetramer exhibits cooperative behaviour or many species of animals have been determined haem-haem interaction. As each haem combines (tabulated by Dayhoff, 1969) and the molecular with oxygen the affinity of successive haems in- structures of horse and human haemoglobins have creases. The oxygen affinity curve of the tetramer been determined in great detail by x-ray crystallo- is sigmoidal and may be represented approximately graphy (Perutz et al, 1968a and b; Perutz 1969). A by the Hill equation:* mechanism of action of haemoglobin has been pro- = kpo2n posed (Perutz, 1970a and b and 1972). The y haemoglobins of higher organisms share a common +kpo2n tetrameric structure built up of two pairs of unlike Oxygen affinity data are usually presented in copyright. chains; the a chains containing 141 amino-acid terms of P102, the partial pressure of oxygen re- residues and the non-a chains containing generally quired to attain half saturation with oxygen, and of 145 or 146 amino acids. In man, five types of n, the exponent of the Hill equation. -

ZNF410 Represses Fetal Globin by Devoted Control of CHD4/Nurd
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.31.272856; this version posted August 31, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Title ZNF410 represses fetal globin by devoted control of CHD4/NuRD Authors Divya S. Vinjamur1, Qiuming Yao1,2, Mitchel A. Cole1, Connor McGuckin1, Chunyan Ren1, Jing Zeng1, Mir Hossain1, Kevin Luk3, Scot A. Wolfe3, Luca Pinello2, Daniel E. Bauer1,4 1Division of Hematology/Oncology, Boston Children’s Hospital, Department of Pediatric Oncology, Dana-Farber Cancer Institute, Harvard Stem Cell Institute, Broad Institute, Department of Pediatrics, Harvard Medical School, Boston, Massachusetts 02115, USA 2Molecular Pathology Unit, Center for Cancer Research, and Center for Computational and Integrative Biology, Massachusetts General Hospital, Department of Pathology, Harvard Medical School, Boston, Massachusetts 02129, USA 3Department of Molecular, Cell and Cancer Biology, Li Weibo Institute for Rare Diseases Research, University of Massachusetts Medical School, Worcester, Massachusetts 01605, USA 4Correspondence: [email protected] bioRxiv preprint doi: https://doi.org/10.1101/2020.08.31.272856; this version posted August 31, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Abstract Major effectors of adult-stage fetal globin silencing include the transcription factors (TFs) BCL11A and ZBTB7A/LRF and the NuRD chromatin complex, although each has potential on- target liabilities for rational �-hemoglobinopathy therapeutic inhibition. -

Analysis of Genetic Determinants Associated with Persistent Synthesis of Fetal Hemoglobin
UNIVERSITÀ DEGLI STUDI DI SASSARI PhD School in Biomolecular and Biotechnological Sciences Curriculum: Biochemistry and Molecular Biology Director: Prof. Claudia Crosio “XXVI Ciclo” Analysis of genetic determinants associated with Persistent Synthesis of Fetal Hemoglobin Supervisor: Monica Pirastru, PhD Director: Prof. Claudia Crosio PhD Student: Sandro Trova ................................................................................................................................................. INDEX INDEX ABSTRACT ................................................................................... 3 INTRODUCTION ......................................................................... 4 1. Hemoglobin .......................................................................................... 4 1.1 Structure and function of Hemoglobin ........................................ 4 1.2 Structure of globin genes and their cluster organization ............. 5 1.3 Genomic context of the α– and β–globin gene clusters .............. 9 2. Globin gene switching ....................................................................... 12 2.1 Regulatory regions and transcription factors of globin genes ... 13 2.2 The β–Globin Locus Control Region (β–LCR) role in globin expression ....................................................................... 20 2.3 Chromatin role in β–like globin gene expression: the PYR role .............................................................................. 25 2.4 Summary on the fetal to adult switch ....................................... -

Iron and Chelation in Biochemistry and Medicine: New Approaches to Controlling Iron Metabolism and Treating Related Diseases
cells Review Iron and Chelation in Biochemistry and Medicine: New Approaches to Controlling Iron Metabolism and Treating Related Diseases George J. Kontoghiorghes * and Christina N. Kontoghiorghe Postgraduate Research Institute of Science, Technology, Environment and Medicine, CY-3021 Limassol, Cyprus * Correspondence: [email protected]; Tel./Fax: +357-2627-2076 Received: 7 May 2020; Accepted: 5 June 2020; Published: 12 June 2020 Abstract: Iron is essential for all living organisms. Many iron-containing proteins and metabolic pathways play a key role in almost all cellular and physiological functions. The diversity of the activity and function of iron and its associated pathologies is based on bond formation with adjacent ligands and the overall structure of the iron complex in proteins or with other biomolecules. The control of the metabolic pathways of iron absorption, utilization, recycling and excretion by iron-containing proteins ensures normal biologic and physiological activity. Abnormalities in iron-containing proteins, iron metabolic pathways and also other associated processes can lead to an array of diseases. These include iron deficiency, which affects more than a quarter of the world’s population; hemoglobinopathies, which are the most common of the genetic disorders and idiopathic hemochromatosis. Iron is the most common catalyst of free radical production and oxidative stress which are implicated in tissue damage in most pathologic conditions, cancer initiation and progression, neurodegeneration and many other diseases. The interaction of iron and iron-containing proteins with dietary and xenobiotic molecules, including drugs, may affect iron metabolic and disease processes. Deferiprone, deferoxamine, deferasirox and other chelating drugs can offer therapeutic solutions for most diseases associated with iron metabolism including iron overload and deficiency, neurodegeneration and cancer, the detoxification of xenobiotic metals and most diseases associated with free radical pathology. -

Arizona Hemoglobin Bart's Fact Sheet for Health Care Providers
Arizona Hemoglobin Bart’s Fact Sheet for Health Care Providers Hemoglobin Barts Your patient has been found on the Arizona Newborn Genetic Screen to have a hemoglobin electrophoresis pattern consistent with "FA Bart’s". The acronym stands for the hemoglobin species present in the baby's blood in descending order of prevalence. The F designates fetal hemoglobin (a2 y2), A denotes hemoglobin A (a2ß2) and Bart’s represents hemoglobin Bart's, a tetramer of y-globin molecules (y4). Hemoglobin Barts (y4) appears in the newborn when one or more of the 4 human a-globin genes are missing. The relative over abundance of y-globin molecules leads to y4 production and the diagnosis of Hemoglobin Barts. Alpha thalassemia is caused by deletions of the alpha globin genes on chromosome 16. Normal individuals have 4 copies of the gene with 2 on each chromosome. It is possible to lose 1 to 4 of these genes. The presence of hemoglobin Bart’s on newborn screen usually suggests that the infant is missing at least 1 alpha gene. The silent carrier: One deleted Alpha Gene Neonates and children with three functional alpha genes have a complete or nearly completely silent phenotype. The red cell indices are normal and remain so for life. When only one a gene is non- functional, the hemoglobin Barts percentage is usually 1-2% in the newborn, and is not detectable when the fetal hemoglobin synthesis stops at 6 months of age. As the newborn matures, the red cells can rarely exhibit a reduced MCV, MCH, but will show normal HBA2 and F levels if the hemoglobin electrophoresis is repeated. -

Hemoglobin/Myoglobin Robert F.Diegelmann, Ph.D
Hemoglobin/Myoglobin Robert F.Diegelmann, Ph.D. OBJECTIVES 1. Describe the interactions of heme, globins and oxygen. 2. Discuss the mechanism responsible for SickleCell Anemia. 3. Understand the clinical significance of A1C hemoglobin. 4. Describe the basic biochemical mechanisms of O2 delivery & CO2 removal. RECOMMENDED RESOURCES Lehninger, Principles of Biochemistry, 5th edition, Chapter 5 Molecular Cell Biology, 5th edition; Lodish et al., page 67 http://web.indstate.edu/thcme/mwking/hemoglobinmyoglobin.html#hemoglobin Myoglobin (muscle) & Hemoglobin (Red Blood Cells) were the first proteins for which three dimensional structures were determined. Professor Max Perutz and his colleagues at Cambridge University determined Hemoglobin’s three dimensional structure in the late 1950s Therefore Hemoglobin is one of the most studied & best understood proteins. Figure 1. The Evolution of the Globin protein family Figure 2. Structural similarity of the Globin proteins Figure 3 Below is the basic heme group structure. It consists of a complex organic ring structure named Protoporphyrin. NOTE: Heme metabolism will be covered in more detail in another lecture. Protoporphyrin prosthetic group Porphyrin ring Fe binding site Methene bridge Substitution sites Figure 4 Oxygen is not very soluble in aqueous solutions and therefore needs a special molecule to be carried to tissues and cells. The Protoporphyrin ring structure of Heme binds a single iron atom in its ferrous (Fe 2+) . The iron atom has six coordination bonds, four are found bound to the nitrogens in the Porphyrin ring system and two additional sites perpendicular to the Porphyrin. The Cytochromes (a, b & c) are proteins that also consist of porphyrin structures. -

Research Article Association Between HBA Locus Copy Number Gains And
INTERNATIONAL JOURNAL OF MEDICAL BIOCHEMISTRY DOI: 10.14744/ijmb.2021.65477 Int J Med Biochem 2021;4(2):91-6 Research Article Association between HBA locus copy number gains and pathogenic HBB gene variants Guven Toksoy1, Nergis Akay2, Agharza Aghayev1, Volkan Karaman1, Sahin Avci1, Tugba Kalayci1, Umut Altunoglu1, Zeynep Karakas2, Zehra Oya Uyguner1 1Department of Medical Genetics, Istanbul University Istanbul Faculty of Medicine, Istanbul, Turkey 2Department of Pediatric Hematology-Oncology, Istanbul University Istanbul Faculty of Medicine, Istanbul, Turkey Abstract Objectives: Alpha (α) and beta (β) thalassemia are the most prevalent genetic hematological disorders. The co-occur- rence of silent β-thalassemia with excess α-globin gene copies is associated with the thalassemia intermedia pheno- type. This study was an investigation of the α-globulin gene dosage and sequence variations in thalassemia patients. Methods: Multiplex ligation-dependent probe amplification and Sanger sequencing were used to identify the hemo- globin subunit alpha 1 (HBA1) and HBA2 gene alterations in 32 patients. Deletion, duplication, and other findings were analyzed in the index cases and family members. Results: Four of the 32 cases (12.5%) were found to have gross duplications. Two cases demonstrated α-globin triplica- tion, and 2 had a quadruplicated HBA1/2 genes. Affected family members revealed genotype-phenotype correlation. In 1 patient, it was observed that quadruplicated HBA genes co-occurrence with hemoglobin subunit beta (HBB) mu- tation was inherited from his mother. Notably, the mother did not demonstrate any thalassemia phenotype. Further investigation showed that the mother was carrying a single copy HBA gene deletion in the trans allele that explained her clinical condition. -

Myoglobin/Hemoglobin O2 Binding and Allosteric Properties
Myoglobin/Hemoglobin O2 Binding and Allosteric Properties of Hemoglobin •Hemoglobin binds and transports H+, O2 and CO2 in an allosteric manner •Allosteric interaction - a regulatory mechanism where a small molecule (effector) binds and alters an enzymes activity ‘globin Function O does not easily diffuse in muscle and O is toxic to biological 2 2 systems, so living systems have developed a way around this. Physiological roles of: – Myoglobin • Transports O2 in rapidly respiring muscle • Monomer - single unit • Store of O2 in muscle high affinity for O2 • Diving animals have large concentration of myoglobin to keep O2 supplied to muscles – Hemoglobin • Found in red blood cells • Carries O2 from lungs to tissues and removes CO2 and H+ from blood to lungs • Lower affinity for O2 than myoglobin • Tetrameter - two sets of similar units (α2β2) Myo/Hemo-globin • Hemoglobin and myoglobin are oxygen- transport and oxygen-storage proteins, respectively • Myoglobin is monomeric; hemoglobin is tetrameric – Mb: 153 aa, 17,200 MW – Hb: two α chains of 141 residues, 2 β chains of 146 residues X-ray crystallography of myoglobin – mostly α helix (proline near end of each helix WHY?) – very small due to the folding – hydrophobic residues oriented towards the interior of the protein – only polar aas inside are 2 histidines Structure of heme prosthetic group Protoporphyrin ring w/ iron = heme Oxygenation changes state of Fe – Purple to red color of blood, Fe+3 - brown Oxidation of Fe+2 destroys biological activity of myoglobin Physical barrier of protein -
Fetal Hemoglobin in Sickle Cell Anemia: Genetic Determinants of Response to Hydroxyurea
The Pharmacogenomics Journal (2007) 7, 386–394 & 2007 Nature Publishing Group All rights reserved 1470-269X/07 $30.00 www.nature.com/tpj ORIGINAL ARTICLE Fetal hemoglobin in sickle cell anemia: genetic determinants of response to hydroxyurea QMa1, DF Wyszynski1, The increase in fetal hemoglobin (HbF) in response to hydroxyurea (HU) 1 2 1 varies among patients with sickle cell anemia. Twenty-nine candidate genes JJ Farrell , A Kutlar , LA Farrer , within loci previously reported to be linked to HbF level (6q22.3–q23.2, 3,1 CT Baldwin and 8q11–q12 and Xp22.2–p22.3), involved in metabolism of HU and related to MH Steinberg1 erythroid progenitor proliferation were studied in 137 sickle cell anemia patients treated with HU. Three-hundred and twenty tagging single 1Department of Medicine, Boston University nucleotide polymorphisms (SNPs) for genotyping were selected based on School of Medicine, Boston, MA, USA; HapMap data. Multiple linear regression and the nonlinear regression 2Department of Medicine, Medical College of Georgia, Augusta, GA, USA and 3Center for Random Forest method were used to investigate the association between Human Genetics, Boston University School of SNPs and the change in HbF level after 2 years of treatment with HU. Both Medicine, Boston, MA, USA methods revealed that SNPs in genes within the 6q22.3–23.2 and 8q11–q12 linkage peaks, and also the ARG2, FLT1, HAO2 and NOS1 genes were Correspondence: Dr MH Steinberg, Center of Excellence in Sickle associated with the HbF response to HU. Polymorphisms in genes regulating Cell Disease, E248, Boston Medical Center, 88 HbF expression, HU metabolism and erythroid progenitor proliferation might E. -
Neonatal Anemia: Recognizing Thalassemia and Hemoglobin Variants
Neonatal Anemia: Recognizing Thalassemia and Hemoglobin Variants James H. Nichols, PhD, DABCC, FACB Professor of Pathology, Microbiology, and Immunology Medical Director, Clinical Chemistry Associate Medical Director of Clinical Operations Vanderbilt University School of Medicine Nashville, TN 37232‐5310 [email protected] Objectives • Describe hemoglobin genetics • Interpret hemoglobin chromatograms and IEF • Recognize common hemoglobin variants Case • 4 mo male, African American, abnormal newborn screen, seen for follow‐up testing • Newborn screen shows hemoglobin FS at birth HbF = 33.8% HbA = <1% HbA2 = 2.7% HbS = 62.5% SickleDex = Positive C S F A NB Audience Poll • What do these results indicate? A. Normal profile B. Abnormal amounts of hemoglobin F C. Sickle cell disease D. Sickle cell trait Hemoglobin Tetramer Chromosomal Organization of Globin Genes Normal Hemoglobins in Adults Hemoglobin Concentration Structure Hb A ~90% 2 2 Hb F ~1.0% 2 2 Hb A2 ~2.5% 2 2 Hb A1 ~7.0% Mixture of post- translational variants of Hb A Globin Chain Expression Reasons for Requesting Hemoglobin Variant Analysis • Follow‐up to abnormal newborn screen • Adoption • Prenatal screening –patients of ethnic origin • Anemia of unknown origin in ethnic patient • Athletic exam for competitive sports Hemoglobinopathies 1. Structural – substitution, addition or deletion of one or more AAs in the globin chain i.e HbS, HbC, HbE, HbD, HbO, etc… 2. Thalassemia‐ quantitative defect in globin chain production i.e. alpha and Beta Thalassemia 3. Combination -

CRISPR-Cas9 Interrogation of a Putative Fetal Globin Repressor in Human Erythroid Cells
bioRxiv preprint doi: https://doi.org/10.1101/335729; this version posted May 31, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. CRISPR-Cas9 interrogation of a putative fetal globin repressor in human erythroid cells. Jennifer Chung1,*, Wendy Magis2*, Jonathan Vu1, Seok-Jin Heo2, Kirmo Wartiovaara2,3,4, Mark C. Walters2,5, Ryo Kurita6, Yukio Nakamura6,7, Dario Boffelli2, David I. K. Martin2,**, Jacob E. Corn1,8,*, Mark A. DeWitt1,** 1Innovative Genomics Institute, University of California, Berkeley, 94720. 2Children’s Hospital Oakland Research Institute, UCSF Benioff Children’s Hospital, Oakland, CA 94609, USA. 3Research Programs Unit, Molecular Neurology and Biomedicum Stem Cell Centre, Faculty of Medicine, University of Helsinki, 00014 Helsinki, Finland 4Clinical Genetics, HUSLAB, Helsinki University Central Hospital, 00290 Helsinki, Finland 5Blood and Marrow Transplant Program, Division of Hematology, UCSF Benioff Children’s Hospital, Oakland, CA 94609, USA. 6Cell Engineering Division, RIKEN BioResource Center, Tsukuba, Ibaraki 305-0074, Japan. 7Faculty of Medicine, University of Tsukuba, Tsukuba, Ibaraki 305-8577, Japan. 6Department of Molecular and Cellular Biology, University of California, Berkeley, 94720. *These authors contributed equally to this work. **co-corresponding authors: Mark DeWitt: [email protected], Jacob Corn: [email protected], David Martin: [email protected] bioRxiv preprint doi: https://doi.org/10.1101/335729; this version posted May 31, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -
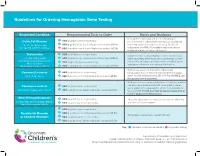
Guidelines for Ordering Hemoglobin Gene Testing
Guidelines for Ordering Hemoglobin Gene Testing Suspected Condition Recommended Tests to Order Notes and Guidance 1 Beta-globin sequencing and deletion mapping are Sickle Cell Disease HBB (β-globin) gene sequencing recommended to differentiate homozygous (e.g. Hb SS) 2 SS, SC, Sβ-thalassemia HBB (β-globin) locus deletion/duplication analysis (MLPA) and compound heterozygous states (e.g. Hb SC, Sβ- SE, SD, SO, S-HPFH, S-Other 3 HBA (α-globin) locus deletion/duplication analysis (MLPA) thalassemia, S-HPFH). Alpha-globin copy number can modify phenotype of sickle cell disease. 1 HBB (β-globin) gene sequencing Thalassemia Comprehensive testing is highly recommended because α, β, (δβ), (γδβ), (εγδβ) 2 HBB (β-globin) locus deletion/duplication analysis (MLPA) of the complexity of the thalassemia syndromes, and the α triplications/quadruplications 3 HBA (α-globin) genes sequencing fact that the phenotype of thalassemia is modified by the Hb E disorders genotypes of both the α-globin and β-globin loci. Hb Constant Spring, others 4 HBA (α-globin) locus deletion/duplication analysis (MLPA) Both panels are recommended to differentiate Common β-variants 1 HBB (β-globin) gene sequencing homozygous (e.g. Hb CC) and compound heterozygous Hb C, D, O, others 2 HBB (β-globin) locus deletion/duplication analysis (MLPA) states (e.g. Hb Cβ-thalassemia, Hb C-HPFH). For Hb E, use the guidance for thalassemia. Both panels are recommended because sequence variants Common α-variants 1 HBA (α-globin) gene sequencing can occur on a chromosome with 1 or 2 α-globin genes, and α-globin gene copy number affects the proportion of 2 Hb G-Philadelphia, Hb I, others HBA (α-globin) locus deletion/duplication analysis (MLPA) the variant Hb.