"I Used to Be Fat": a Qualitative Analysis of Bariatric Surgery Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Liminal Losers: Breakdowns and Breakthroughs in Reality Television's Biggest Hit
Western Michigan University ScholarWorks at WMU Master's Theses Graduate College 4-2013 Liminal Losers: Breakdowns and Breakthroughs in Reality Television's Biggest Hit Caitlin Rickert Follow this and additional works at: https://scholarworks.wmich.edu/masters_theses Part of the Broadcast and Video Studies Commons, and the Health Communication Commons Recommended Citation Rickert, Caitlin, "Liminal Losers: Breakdowns and Breakthroughs in Reality Television's Biggest Hit" (2013). Master's Theses. 136. https://scholarworks.wmich.edu/masters_theses/136 This Masters Thesis-Open Access is brought to you for free and open access by the Graduate College at ScholarWorks at WMU. It has been accepted for inclusion in Master's Theses by an authorized administrator of ScholarWorks at WMU. For more information, please contact [email protected]. LIMINAL LOSERS: BREAKDOWNS AND BREAKTHROUGHS IN REALITY TELEVISION’S BIGGEST HIT by Caitlin Rickert A Thesis submitted to the Graduate College in partial fulfillment of the requirements for the degree of Master of Arts School of Communication Western Michigan University April 2013 Thesis Committee: Heather Addison, Ph. D., Chair Sandra Borden, Ph. D. Joseph Kayany, Ph. D. LIMINAL LOSERS: BREAKDOWNS AND BREAKTHROUGHS IN REALITY TELEVISION’S BIGGEST HIT Caitlin Rickert, M.A. Western Michigan University, 2013 This study explores how The Biggest Loser, a popular television reality program that features a weight-loss competition, reflects and magnifies established stereotypes about obese individuals. The show, which encourages contestants to lose weight at a rapid pace, constructs a broken/fixed dichotomy that oversimplifies the complex issues of obesity and health. My research is a semiotic analysis of the eleventh season of the program (2011), focusing on three pairs of contestants (or “couples” teams) that each represent a different level of commitment to the program’s values. -

Tv Pg 01-04-11.Indd
The Goodland Star-News / Tuesday, January 4, 2011 7 All Mountain Time, for Kansas Central TIme Stations subtract an hour TV Channel Guide Tuesday Evening January 4, 2011 7:00 7:30 8:00 8:30 9:00 9:30 10:00 10:30 11:00 11:30 28 ESPN 57 Cartoon Net 21 TV Land 41 Hallmark ABC No Ordinary Family V Detroit 1-8-7 Local Nightline Jimmy Kimmel Live S&T Eagle CBS Live to Dance NCIS Local Late Show Letterman Late 29 ESPN 2 58 ABC Fam 22 ESPN 45 NFL NBC The Biggest Loser Parenthood Local Tonight Show w/Leno Late 2 PBS KOOD 2 PBS KOOD 23 ESPN 2 47 Food FOX Glee Million Dollar Local 30 ESPN Clas 59 TV Land Cable Channels 3 KWGN WB 31 Golf 60 Hallmark 3 NBC-KUSA 24 ESPN Nws 49 E! A&E The First 48 The First 48 The First 48 The First 48 Local 5 KSCW WB 4 ABC-KLBY AMC Demolition Man Demolition Man Crocodile Local 32 Speed 61 TCM 25 TBS 51 Travel ANIM 6 Weather When Animals Strike When Animals Strike When Animals Strike When Animals Strike Animals Local 6 ABC-KLBY 33 Versus 62 AMC 26 Animal 54 MTV BET American Gangster The Mo'Nique Show Wendy Williams Show State 2 Local 7 CBS-KBSL BRAVO Matchmaker Matchmaker The Fashion Show Matchmaker Matchmaker 7 KSAS FOX 34 Sportsman 63 Lifetime 27 VH1 55 Discovery CMT Local Local The Dukes of Hazzard The Dukes of Hazzard Canadian Bacon 8 NBC-KSNK 8 NBC-KSNK 28 TNT 56 Fox Nws CNN 35 NFL 64 Oxygen Larry King Live Anderson Cooper 360 Larry King Live Anderson Local 9 Eagle COMEDY 29 CNBC 57 Disney Tosh.0 Tosh.0 Tosh.0 Tosh.0 Daily Colbert Tosh.0 Tosh.0 Futurama Local 9 NBC-KUSA 37 USA 65 We DISC Local Local Dirty Jobs -

Body Curves and Story Arcs
Body Curves and Story Arcs: Weight Loss in Contemporary Television Narratives ! ! ! Thesis submitted to Jawaharlal Nehru University and Università degli Studi di Bergamo, as part of Erasmus Mundus Joint Doctorate Program “Cultural Studies in Literary Interzones,” in partial fulfilment of the requirements for the degree of ! Doctor of Philosophy ! ! by ! ! Margaret Hass ! ! ! Centre for English Studies School of Language, Literature and Culture Studies Jawaharlal Nehru University New Delhi - 110067, India 2016 ! Table of Contents !Acknowledgements !Foreword iii Introduction: Body Curves and Story Arcs Between Fat Shame and Fat Studies 1 Liquid Modernity, Consumer Culture, and Weight Loss 5 Temporality and Makeover Culture in Liquid Modernity 10 The Teleology of Weight Loss, or What Jones and Bauman Miss 13 Fat Studies and the Transformation of Discourse 17 Alternative Paradigms 23 Lessons from Feminism: Pleasure and Danger in Viewing Fat 26 Mediatization and Medicalization 29 Fictional Roles, Real Bodies 33 Weight and Television Narratology 36 Addressing Media Texts 39 Selection of Corpus 43 ! Description of Chapters 45 Part One: Reality! TV Change in “Real” Time: The Teleologies and Temporalities of the Weight Loss Makeover 48 I. Theorizing the Weight Loss Makeover: Means and Ends Paradoxes 52 Labor Revealed: Exercise and Affect 57 ! Health and the Tyranny of Numbers 65 II. The Temporality of Transformation 74 Before/After and During 81 Temporality and Mortality 89 Weight Loss and Becoming an Adult 96 I Used to Be Fat 97 ! Jung und Dick! Eine Generation im Kampf gegen Kilos 102 III. Competition and Bodily Meritocracy 111 The Biggest Loser: Competition, Social Difference, and Redemption 111 Redemption and Difference 117 Gender and Competition 120 Beyond the Telos: Rachel 129 Another Aesthetics of Competition: Dance Your Ass Off 133 ! IV. -

Healthism and Fat Politics in TLC's My Big Fat Fabulous Life
Repositorium für die Geschlechterforschung “I Wanna Be Fat” : Healthism and Fat Politics in TLC’s My Big Fat Fabulous Life Kindinger, Evangelia 2017 https://doi.org/10.25595/1555 Veröffentlichungsversion / published version Zeitschriftenartikel / journal article Empfohlene Zitierung / Suggested Citation: Kindinger, Evangelia: “I Wanna Be Fat” : Healthism and Fat Politics in TLC’s My Big Fat Fabulous Life, in: FKW : Zeitschrift für Geschlechterforschung und visuelle Kultur (2017) Nr. 62, 48-60. DOI: https://doi.org/10.25595/1555. Nutzungsbedingungen: Terms of use: Dieser Text wird unter einer CC BY NC ND 4.0 Lizenz This document is made available under a CC BY NC ND 4.0 (Namensnennung - Nicht kommerziell - Keine Bearbeitung) zur License (Attribution - NonCommercial - NoDerivates). For more Verfügung gestellt. Nähere Auskünfte zu dieser Lizenz finden Sie information see: hier: https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode.de www.genderopen.de // Evangelia Kindinger “I WANNA BE FAT”: HEALTHISM AND FAT POLITICS IN TLC’S MY BIG FAT FABULOUS LIFE “I wanna be fat.” – This sentence uttered by Whitney Thore, the 1) protagonist of TLC’s My Big Fat Fabulous Life (2015–), in the third Onwards cited as MBFFL. In Germany, the series is broadcasted as Whitney! season’s premiere episode is astonishing because, as the public is – Voll im Leben. lectured time and again by media, medical doctors and other so 2) called health professionals, nobody wants to be (or should be) fat. Cf.: http://www.nobodyshame.com Thore’s declaration becomes even more conspicuous considering (January 2017) its context, namely a reality TV program. -

Wednesday Morning, March 28
WEDNESDAY MORNING, MARCH 28 FRO 6:00 6:30 7:00 7:30 8:00 8:30 9:00 9:30 10:00 10:30 11:00 11:30 COM 4:30 KATU News This Morning (N) Good Morning America (N) (cc) AM Northwest (cc) The View 50 Cent; Vera Wang; Live! With Kelly Jessica Biel; Abi- 2/KATU 2 2 (cc) (Cont’d) Bone Hampton. (cc) (TV14) gail Breslin. (N) (cc) (TVPG) KOIN Local 6 at 6am (N) (cc) CBS This Morning (N) (cc) Let’s Make a Deal (N) (cc) (TVPG) The Price Is Right (N) (cc) (TVG) The Young and the Restless (N) (cc) 6/KOIN 6 6 (TV14) NewsChannel 8 at Sunrise at 6:00 Today The Hiring Our Heroes Today initiative. (N) (cc) Anderson (cc) (TVG) 8/KGW 8 8 AM (N) (cc) EXHALE: Core Wild Kratts (cc) Curious George Cat in the Hat Super Why! Dinosaur Train Sesame Street Gina teaches Sid the Science Clifford the Big Martha Speaks WordWorld (TVY) 10/KOPB 10 10 Fusion (TVG) (TVY) (TVY) Knows a Lot (TVY) (TVY) Marco about Spanish. (cc) (TVY) Kid (TVY) Red Dog (TVY) (TVY) Good Day Oregon-6 (N) Good Day Oregon (N) MORE Good Day Oregon The 700 Club (cc) (TVPG) Law & Order: Criminal Intent An ear 12/KPTV 12 12 surgeon’s murder. (TV14) International Fel- Paid Paid Paid Zula Patrol (cc) Pearlie (TVY7) Through the Bible International Fel- Paid Paid Paid Paid 22/KPXG 5 5 lowship (TVY) lowship Creflo Dollar (cc) John Hagee Breakthrough This Is Your Day Believer’s Voice Winning With 360 Degree Life Pro-Claim Behind the Joyce Meyer Life Today With Today: Marilyn & 24/KNMT 20 20 (TVG) Today (cc) (TVG) W/Rod Parsley (cc) (TVG) of Victory (cc) Wisdom (cc) Scenes (cc) James Robison Sarah Eye Opener (N) (cc) My Name Is Earl My Name Is Earl Swift Justice: Swift Justice: Maury (cc) (TV14) The Steve Wilkos Show (cc) (TVPG) 32/KRCW 3 3 (TV14) (TV14) Jackie Glass Jackie Glass Andrew Wom- Paid The Jeremy Kyle Show (N) (cc) America Now (cc) Divorce Court (N) Excused (cc) Excused (cc) Cheaters (cc) Cheaters (cc) America’s Court Judge Alex (N) 49/KPDX 13 13 mack (TVPG) (TVG) (TVPG) (TV14) (TV14) (TV14) (TV14) (cc) (TVPG) Paid Paid Dog the Bounty Hunter (cc) (TVPG) Dog the Bounty Hunter (cc) (TVPG) Criminal Minds Mayhem. -
Harrells Man Killed After Crash
Swinging into action Remember, act, educate, spread the word SCC Foundation gears up for annual golf tourney, National Breast Cancer Awareness Month Page A6 THE SAMPSON INDE www.clintonnc.comPENDENT 50 cents F Vol. LXXXVII; Issue 201 Tuesday, October 11, 2011 Clinton, North Carolina F 12 pages Harrells man killed after crash Speed a factor in tragic accident By DOUG CLARK Willie Floyd Crumpler, 45, of was driving along Cannady Road early the crash was 75 mph, a factor, the Tomahawk Highway, Harrells, was Sunday morning when he came around report noted, in the accident. Assistant Editor killed after being ejected from his a curve too fast and struck a concrete Crumpler, it was noted, died at the A 45-year-old Harrells man became 1995 Lexus just 6.7 miles west of driveway culvert. The Lexus flipped scene. the 14th person killed on Sampson Harrells, on Cannady Road, around several times, eventually ejecting No other injuries were reported. County roadways this year when he 1:40 a.m., according to reports by N.C. Crumpler, who was not wearing a seat To reach Doug Clark call 910-592- lost control of his vehicle in a one-car Highway Patrol trooper R.S. Smith. belt. 8137 ext. 123 or email to sisports@ accident Sunday. Those reports note that Crumpler His estimated speed at the time of heartlandpublications.com. Sex case Hobbton cookbook Fugitive heads to featured in state magazine caught court in R’boro By DOUG CLARK this week Assistant Editor By DOUG CLARK A routine traffic stop in Roseboro Assistant Editor has led to the apprehension of a fugi- tive wanted on outstanding fraud and The case of a drug charges by the state of Maryland. -
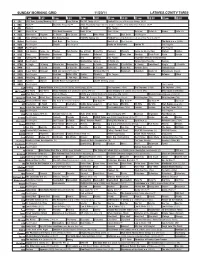
Sunday Morning Grid 11/20/11 Latimes.Com/Tv Times
SUNDAY MORNING GRID 11/20/11 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Morning (N) Å Face/Nation The NFL Today (N) Å Football Raiders at Minnesota Vikings. (N) Å 4 NBC News Å Meet the Press (N) Å 2011 Presidents Cup Final Day. Singles matches. From Melbourne, Australia. (N) Å 5 CW News Å In Touch Paid Program 7 ABC News (N) Å This Week-Amanpour News (N) Å News (N) Å News Å Vista L.A. Heroes Vista L.A. 9 KCAL Tomorrow’s Kingdom K. Shook Joel Osteen Prince Mike Webb Paid Best Deals Paid Program 11 FOX Hour of Power (N) (TVG) Fox News Sunday FOX NFL Sunday (N) Football Tampa Bay Buccaneers at Green Bay Packers. (N) Å 13 MyNet Paid Program Best Buys Paid Program Best of L.A. Paid Program The Hoax ››› (2006) 18 KSCI Paid Program Church Paid Program Hecho en Guatemala Iranian TV Paid Program 22 KWHY Paid Program Paid Program 24 KVCR Sid Science Curios -ity Thomas Bob Builder Joy of Paint Paint This Dewberry Wyland’s Home for Christy Rost Kitchen Kitchen 28 KCET Cons. Wubbulous Busytown Peep Pancakes Pufnstuf Lidsville Place, Own Roadtrip Chefs Field Pépin Venetia 30 ION Turning Pnt. Discovery In Touch Paid Beyond Paid Program Inspiration Ministry Campmeeting 34 KMEX Paid Program Muchachitas Como Tu Al Punto (N) Aurora Valle Presenta... Vecinos 40 KTBN K. Hagin Ed Young Miracle-You Redemption Love In Touch PowerPoint It Is Written B. -
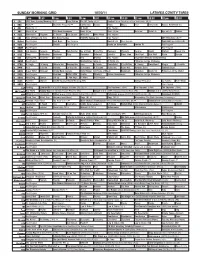
Sunday Morning Grid 10/30/11 Latimes.Com/Tv Times
SUNDAY MORNING GRID 10/30/11 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Morning (N) Å Face/Nation The NFL Today (N) Å Football Miami Dolphins at New York Giants. (N) Å 4 NBC News Å Meet the Press (N) Å Conference George House House Paid Travel Cafe Access Hollywood (N) 5 CW News (N) Å In Touch Paid Program 7 ABC News (N) Å This Week-Amanpour News (N) Å News (N) Å News Å Vista L.A. Eye on L.A. Motion 9 KCAL Tomorrow’s Kingdom K. Shook Joel Osteen Ministries Mike Webb Paid Program 11 FOX Hour of Power (N) (TVG) Fox News Sunday FOX NFL Sunday (N) Paid Program UFC Primetime (N) Å 13 MyNet Paid Program Best Buys Paid Program Best of L.A. Paid Program From Hell ›› (2001) (R) 18 KSCI Paid Program Church Paid Program Hecho en Guatemala Iranian TV Paid Program 22 KWHY Paid Program Paid Program 24 KVCR Sid Science Curiosity Thomas Bob Builder Joy of Paint Paint This Dewberry Wyland’s Cuisine Cook’s Kitchen Sweet Life 28 KCET Cons. Wubbulous Busytown Peep Pancakes Pufnstuf Lidsville Place, Own Chef Paul Burt Wolf Pépin Venetia 30 ION Turning Pnt. Discovery In Touch Paid Beyond Paid Program Inspiration Ministry Campmeeting 34 KMEX Paid Program Muchachitas Como Tu Al Punto (N) Fútbol de la Liga Mexicana 40 KTBN K. Hagin Ed Young Miracle-You Redemption Love In Touch PowerPoint It Is Written B. -

PACIFIC LINGUISTICS Research School of Pacific and Asian Studies
PACIFIC LINGUISTICS Research School of Pacific and Asian Studies THE AUSTRALIAN NATIONAL UNIVERSITY Out of print book This .pdf (portable document file) document is an image file produced from a scan of an original copy of the book. It may not be reproduced without the permission of Pacific Linguistics. Pacific Linguistics Home Page: http://www.pacling.com Colloquial Jakartan Indonesian James Neil Sneddon PL 581 This book aims to describe aspects of the Indonesian language as spoken by educated Jakartans in everyday interactions. This style of language is in many ways significantly different from the formal language of government and education, to the extent that it deserves separate consideration. While formal Indonesian has been the subject of a considerable amount of description very little attention has been paid to informal styles of the language. The variety described here, Colloquial Jakartan Indonesian, is the prestige variety of colloquial Indonesian and is becoming the standard informal style. The description and texts in following chapters are drawn from recordings of natural speech of educated people living in Jakarta. While the book aims to inform those with a background in linguistics the needs of teachers and learners with little or no knowledge of linguistics is always borne in mind. The work thus does not consider theoretical linguistic issues nor use technical terms which would not be readily understood by most readers. 2006 ISBN 085883 571 1 298 pp Prices: Australia AUD $30.25 (incl. GST) Overseas AUD $27.50 Colloquial Jakartan Indonesian Pacific Linguistics 581 Pacific Linguistics is a publisher specialising in grammars and linguistic descriptions, dictionaries and other materials on languages of the Pacific, Taiwan, the Philippines, Indonesia, East Timor, southeast and south Asia, and Australia. -

Sunday Morning Grid 10/9/11
SUNDAY MORNING GRID 10/9/11 LATIMES.COM/TV TIMES 7 am 7:30 8 am 8:30 9 am 9:30 10 am 10:30 11 am 11:30 12 pm 12:30 2 CBS CBS News Sunday Morning (N) Å Face/Nation The NFL Today (N) Å Football Raiders at Houston Texans. From Reliant Stadium in Houston. (N) 4 NBC News Å Meet the Press (N) News George House House Paid Program Access Hollywood (N) 5 CW News Å In Touch Paid Program 7 ABC News (N) Å This Week-Amanpour News (N) Å News (N) Å Jack Hanna Ocean Mys. Explore Culture 9 KCAL Tomorrow’s Kingdom K. Shook Joel Osteen Ministries Mike Webb Paid Program 11 FOX Hour of Power (N) (TVG) Fox News Sunday FOX NFL Sunday (N) Football Philadelphia Eagles at Buffalo Bills. (N) Å 13 MyNet Paid Program Best Buys Paid Program Best of L.A. Paid Program Day Parents Ran Away 18 KSCI Paid Program Grace Paid Program Hecho en Guatemala Iranian TV (In Farsi) Paid Program 22 KWHY Paid Program Paid Program 24 KVCR Sid Science Curios -ity Thomas Bob Builder Joy of Paint Paint This Dewberry Wyland’s Cuisine Cook’s Kitchen Sweet Life 28 KCET Cons. Wubbulous Busytown Peep Pancakes Pufnstuf Lidsville Place, Own Chef Paul Burt Wolf Pepin Venetia 30 ION Turning Pnt. Discovery In Touch Paid Beyond Paid Program Inspiration Ministry Campmeeting 34 KMEX Paid Program Muchachitas Como Tu Al Punto (N) República Deportiva 40 KTBN K. Hagin Ed Young Miracle-You Redemption Love In Touch PowerPoint It Is Written B. -

DGA Reality Directors Contact Guide
DGA’s REALITY DIRECTORS Contact Guide EF OP CH PRO T JE CT R FACT RU SE FEAR OR N W LO D BI A T E G Y S K K B E A K TAN A R N R ME O G HA R T G G S I H I N C I A E B ’ R T S A F E N D H E C X E R T C E F T T A F O S R O A P G E M M C N O I A Z F D A E R L M O I A R R E R T S S A I E A B W S D R T M A P A O T J K N A E K I E E N Y E V I B N N A C L A I R M E E A S T K M A U M L I E L T E L R C U H C A I L L A C E E N G A R N G G A R R I D T S ’ L U R A U P 7/2018 WHAT PRODUCERS AND AGENTS ARE SAYING ABOUT DGA REALITY AGREEMENTS: “The DGA has done an amazing job of building strong relationships with unscripted Producers. They understand that each show is different and work with us to structure deals that make sense for both the Producers and their Members on projects of all sizes and budgets. -

Adolescents' Explicit and Implicit Weight Bias Following Exposure To
Media Psychology ISSN: 1521-3269 (Print) 1532-785X (Online) Journal homepage: http://www.tandfonline.com/loi/hmep20 “Weak, Sad, and Lazy Fatties”: Adolescents’ Explicit and Implicit Weight Bias Following Exposure to Weight Loss Reality TV Shows Kathrin Karsay & Desirée Schmuck To cite this article: Kathrin Karsay & Desirée Schmuck (2017): “Weak, Sad, and Lazy Fatties”: Adolescents’ Explicit and Implicit Weight Bias Following Exposure to Weight Loss Reality TV Shows, Media Psychology, DOI: 10.1080/15213269.2017.1396903 To link to this article: https://doi.org/10.1080/15213269.2017.1396903 © 2017 Kathrin Karsay and Desirée Schmuck. Published with license by Taylor & Francis Group. Published online: 13 Nov 2017. Submit your article to this journal Article views: 448 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=hmep20 MEDIA PSYCHOLOGY https://doi.org/10.1080/15213269.2017.1396903 “Weak, Sad, and Lazy Fatties”: Adolescents’ Explicit and Implicit Weight Bias Following Exposure to Weight Loss Reality TV Shows Kathrin Karsay and Desirée Schmuck Department of Communication, University of Vienna, Vienna Austria ABSTRACT Weight loss reality TV shows, which portray obese individuals and their struggle to lose weight, are highly popular. However, the shows often contain negative and stereotypical portrayals of obese individuals that can contribute to the formation of weight bias among viewers. In particular, adolescents might be highly susceptible to such portrayals, since physical appearance and body image play an important role during adolescence. In our experimental study, we investigated the priming effects of expo- sure to weight loss reality TV shows on implicit and explicit atti- tudes toward obese individuals among 353 adolescents.