Interstitial Pneumonia with Autoimmune Features: Why Rheumatologist-Pulmonologist Collaboration Is Essential
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Newsletter Editor: Yoichi Nakanishi Associate Editors: Yoshinosuke Fukuchi, David CL Lam, Suga Konno
Vol.30, No.1 (January 2021) Newsletter Editor: Yoichi Nakanishi Associate Editors: Yoshinosuke Fukuchi, David CL Lam, Suga Konno Message from the President A Happy New Year to all APSR members. Last year was a year of COVID-19. The APSR was also influenced by the disease, and the APSR 2020 Congress in Kyoto was postponed to 2021. I would express sincere appreciation to the Japanese Local Congress Committee team for their tremendous efforts to re-arrange the Congress, and also to the Korean Local Congress Committee team for their kind acceptance of postponement of the APSR Congress in Seoul to 2022. Under this difficult situation, we should not stagnate scientific progress and educational activities. We have held two COVID-19 webinars, three APSR virtual meetings, an ATS-APSR joint webinar, joint symposia with the Philippine College of Chest Physicians (PCCP), the Malaysian Thoracic Society (MTS) and the Taiwan Society of Pulmonary and Critical Care Medicine (TSPCCM). It is a great pleasure that many APSR members joined these web meetings and all of them were so successful. I am profoundly grateful to the Central Congress Committee members, Assembly members, presenters, facilitators, audiences, en bloc members, sponsors and the APSR secretariat office. The Asia-Pacific region has the biggest population in the world and is accomplishing rapid development, though it still has many health problems such as air pollution, tobacco smoking, respiratory infection including tuberculosis, and poor medical infrastructure. We are happy to have lots of projects to solve these problems. This year, we are going to further enhance our activities in order to achieve our objectives, i.e., “The advancement and promotion of knowledge of the respiratory system in health and disease, which strives to encourage research, improve clinical practice through teaching, increase awareness of health problems in the area and promote the exchange of knowledge among respirologists in the Asia-Pacific region”. -

Scientific Publications in Respiratory Journals from Chinese
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2013-004201 on 28 February 2014. Downloaded from Scientific publications in respiratory journals from Chinese authors in various parts of North Asia: a 10-year survey of literature Bo Ye,1 Ting-Ting Du,1 Ting Xie,2 Jun-Tao Ji,1 Zhao-Hong Zheng,1 Zhuan Liao,1 Liang-Hao Hu,1 Zhao-Shen Li1 To cite: Ye B, Du T-T, Xie T, ABSTRACT et al Strengths and limitations of this study . Scientific publications in Objectives: Respiratory disease remains one of the respiratory journals from leading causes of morbidity and mortality in China. Chinese authors in various A few journals covered resources beyond respiratory However, little is known about the research status of parts of North Asia: a 10-year even selected from the respiratory system of Science — survey of literature. BMJ Open respirology in three major regions of China Mainland Citation Index Expanded (SCIE). Besides, some 2014;4:e004201. doi:10.1136/ (ML), Hong Kong (HK) and Taiwan (TW). A 10-year related journals not shown in SCIE were not col- bmjopen-2013-004201 survey of literature was conducted to compare the lected. Some respiratory medicine research articles three regions’ outputs in the research of respirology. were published in general journals, rather than in the ▸ Prepublication history for Design: A bibliometric study. specialized ones. Searching by the author’s address this paper is available online. Setting: China. (China, HK or TW) led to another problem that the To view these files please Participants and outcome measures: A literature articles which addressed other cities or provinces visit the journal online search in PubMed database, updated as of September were not included. -
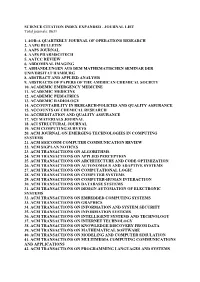
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total Journals: 8631
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total journals: 8631 1. 4OR-A QUARTERLY JOURNAL OF OPERATIONS RESEARCH 2. AAPG BULLETIN 3. AAPS JOURNAL 4. AAPS PHARMSCITECH 5. AATCC REVIEW 6. ABDOMINAL IMAGING 7. ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG 8. ABSTRACT AND APPLIED ANALYSIS 9. ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY 10. ACADEMIC EMERGENCY MEDICINE 11. ACADEMIC MEDICINE 12. ACADEMIC PEDIATRICS 13. ACADEMIC RADIOLOGY 14. ACCOUNTABILITY IN RESEARCH-POLICIES AND QUALITY ASSURANCE 15. ACCOUNTS OF CHEMICAL RESEARCH 16. ACCREDITATION AND QUALITY ASSURANCE 17. ACI MATERIALS JOURNAL 18. ACI STRUCTURAL JOURNAL 19. ACM COMPUTING SURVEYS 20. ACM JOURNAL ON EMERGING TECHNOLOGIES IN COMPUTING SYSTEMS 21. ACM SIGCOMM COMPUTER COMMUNICATION REVIEW 22. ACM SIGPLAN NOTICES 23. ACM TRANSACTIONS ON ALGORITHMS 24. ACM TRANSACTIONS ON APPLIED PERCEPTION 25. ACM TRANSACTIONS ON ARCHITECTURE AND CODE OPTIMIZATION 26. ACM TRANSACTIONS ON AUTONOMOUS AND ADAPTIVE SYSTEMS 27. ACM TRANSACTIONS ON COMPUTATIONAL LOGIC 28. ACM TRANSACTIONS ON COMPUTER SYSTEMS 29. ACM TRANSACTIONS ON COMPUTER-HUMAN INTERACTION 30. ACM TRANSACTIONS ON DATABASE SYSTEMS 31. ACM TRANSACTIONS ON DESIGN AUTOMATION OF ELECTRONIC SYSTEMS 32. ACM TRANSACTIONS ON EMBEDDED COMPUTING SYSTEMS 33. ACM TRANSACTIONS ON GRAPHICS 34. ACM TRANSACTIONS ON INFORMATION AND SYSTEM SECURITY 35. ACM TRANSACTIONS ON INFORMATION SYSTEMS 36. ACM TRANSACTIONS ON INTELLIGENT SYSTEMS AND TECHNOLOGY 37. ACM TRANSACTIONS ON INTERNET TECHNOLOGY 38. ACM TRANSACTIONS ON KNOWLEDGE DISCOVERY FROM DATA 39. ACM TRANSACTIONS ON MATHEMATICAL SOFTWARE 40. ACM TRANSACTIONS ON MODELING AND COMPUTER SIMULATION 41. ACM TRANSACTIONS ON MULTIMEDIA COMPUTING COMMUNICATIONS AND APPLICATIONS 42. ACM TRANSACTIONS ON PROGRAMMING LANGUAGES AND SYSTEMS 43. ACM TRANSACTIONS ON RECONFIGURABLE TECHNOLOGY AND SYSTEMS 44. -

Volume 24.1 (Jan 2015)
Vol.24, No.1 (January, 2015) Editor : Michiaki Mishima Associate Editors : Yoshinosuke Fukuchi, J Patrick Barron, Kwun M Fong, Yasutomi Yamanaka Message from the President Dear APSR members; I am honoured to take this opportunity to deliver this first message to all my colleagues — the APSR members. First of all, I would like to say thank you very much for your continuing great support to the Asian Pacific Society of Respirology. Attended by over 2,700 delegates from around the world, the 19th Congress of the APSR in Bali, Indonesia, was successfully staged in November 2014, with the great cooperation of the Indonesian Society of Respirology led by Dr Faisal Yunus. Another milestone to celebrate is the Impact Factor of our official journal; Respirology, which jumped from 2.781 in 2012 to 3.495 in 2013. Respirology is now ranked the 15th out of 53 journals in the Respiratory System category, compared with being the 18th the previous year. Respirology Case Reports has been steadily building a sound reputation in the short period since its inauguration. I would like to thank particularly Dr Peter Eastwood, Dr Norbert Berend and their colleagues at the Editorial Office for their excellent achievement. In addition, an education component called 'ESAP' (Educational Seminar of the APSR) has been used to implement seminars in the Asia-Pacific region, coordinated by Dr David Lam. Three ESAPs were held in 2014: 'State of the Art Pulmonology' in Quezon City, Philippines, in August; 'Lung cancer' in Bali, Indonesia, in November prior to the APSR2014 Congress; and finally 'Paediatric Asthma' in Ho Chi Minh City, Vietnam in December. -

2018 Journal Citation Reports Journals in the 2018 Release of JCR 2 Journals in the 2018 Release of JCR
2018 Journal Citation Reports Journals in the 2018 release of JCR 2 Journals in the 2018 release of JCR Abbreviated Title Full Title Country/Region SCIE SSCI 2D MATER 2D MATERIALS England ✓ 3 BIOTECH 3 BIOTECH Germany ✓ 3D PRINT ADDIT MANUF 3D PRINTING AND ADDITIVE MANUFACTURING United States ✓ 4OR-A QUARTERLY JOURNAL OF 4OR-Q J OPER RES OPERATIONS RESEARCH Germany ✓ AAPG BULL AAPG BULLETIN United States ✓ AAPS J AAPS JOURNAL United States ✓ AAPS PHARMSCITECH AAPS PHARMSCITECH United States ✓ AATCC J RES AATCC JOURNAL OF RESEARCH United States ✓ AATCC REV AATCC REVIEW United States ✓ ABACUS-A JOURNAL OF ACCOUNTING ABACUS FINANCE AND BUSINESS STUDIES Australia ✓ ABDOM IMAGING ABDOMINAL IMAGING United States ✓ ABDOM RADIOL ABDOMINAL RADIOLOGY United States ✓ ABHANDLUNGEN AUS DEM MATHEMATISCHEN ABH MATH SEM HAMBURG SEMINAR DER UNIVERSITAT HAMBURG Germany ✓ ACADEMIA-REVISTA LATINOAMERICANA ACAD-REV LATINOAM AD DE ADMINISTRACION Colombia ✓ ACAD EMERG MED ACADEMIC EMERGENCY MEDICINE United States ✓ ACAD MED ACADEMIC MEDICINE United States ✓ ACAD PEDIATR ACADEMIC PEDIATRICS United States ✓ ACAD PSYCHIATR ACADEMIC PSYCHIATRY United States ✓ ACAD RADIOL ACADEMIC RADIOLOGY United States ✓ ACAD MANAG ANN ACADEMY OF MANAGEMENT ANNALS United States ✓ ACAD MANAGE J ACADEMY OF MANAGEMENT JOURNAL United States ✓ ACAD MANAG LEARN EDU ACADEMY OF MANAGEMENT LEARNING & EDUCATION United States ✓ ACAD MANAGE PERSPECT ACADEMY OF MANAGEMENT PERSPECTIVES United States ✓ ACAD MANAGE REV ACADEMY OF MANAGEMENT REVIEW United States ✓ ACAROLOGIA ACAROLOGIA France ✓ -
2017 Latest Impact Factors (2016 Journal Citation Reports, Thomson Reuters)
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/317639994 2017 Latest Impact Factors (2016 Journal Citation Reports, Thomson Reuters) Research · June 2017 CITATIONS READS 0 23,550 1 author: Anket Sharma Guru Nanak Dev University 42 PUBLICATIONS 34 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Brassinosteroids and Abiotic Stress management in Plants View project 24-epibrassinolide regulated detoxification of imidacloprid in Brassica juncea L. View project All content following this page was uploaded by Anket Sharma on 17 June 2017. The user has requested enhancement of the downloaded file. Journal Data Filtered By: Selected JCR Year: 2016 Selected Editions: SCIE,SSCI Selected Category Scheme: WoS Journal Impact Rank Full Journal Title Total Cites Eigenfactor Score Factor 1 CA-A CANCER JOURNAL FOR CLINICIANS 24,539 187.040 0.064590 2 NEW ENGLAND JOURNAL OF MEDICINE 315,143 72.406 0.700770 3 NATURE REVIEWS DRUG DISCOVERY 28,750 57.000 0.060820 4 CHEMICAL REVIEWS 159,155 47.928 0.246600 5 LANCET 214,732 47.831 0.404930 6 NATURE REVIEWS MOLECULAR CELL BIOLOGY40,565 46.602 0.095760 7 JAMA-JOURNAL OF THE AMERICAN MEDICAL141,015 ASSOCIATION44.405 0.280910 8 NATURE BIOTECHNOLOGY 53,992 41.667 0.169930 9 NATURE REVIEWS GENETICS 32,654 40.282 0.102540 10 NATURE 671,254 40.137 1.433990 11 NATURE REVIEWS IMMUNOLOGY 34,948 39.932 0.093010 12 NATURE MATERIALS 81,831 39.737 0.204020 13 Nature Nanotechnology 48,814 38.986 0.172520 14 -
Apsr Respiratory Updates
APSR RESPIRATORY UPDATES Volume 11 Issue 8 Newsletter Date: August 2019 APSR EDUCATION PUBLICATION Inside this issue: Bronchoscopy How Many Passes Are Needed for Endobronchial Ultrasound-Guided Transbronchial Needle Aspira- 2 tion for Sarcoidosis? A Prospective Multicenter Study. Endoscopic Ultrasound with Bronchoscope-Guided Fine Needle Aspiration for the Diagnosis of 3 Paraesophageally Located Lung Lesions. Impact of Rapid On-Site Cytological Evaluation (ROSE) on the Diagnostic Yield of Transbronchial Nee- 4 dle Aspiration During Mediastinal Lymph Node Sampling: Systematic Review and Meta-Analysis. The Evolutional History of Electromagnetic Navigation Bronchoscopy: State of the Art. 4 Poor Concordance between Sequential Transbronchial Lung Cryobiopsy and Surgical Lung Biopsy in 5 the Diagnosis of Diffuse Interstitial Lung Diseases. Long-Term Quality-Adjusted Survival following Therapeutic Bronchoscopy for Malignant Central Air- 6 way Obstruction. Effectiveness of Bronchial Thermoplasty in Patients with Severe Refractory Asthma: Clinical and His- 7 topathologic Correlations. A Multicenter Randomized Controlled Trial of Zephyr Endobronchial Valve Treatment in Heterogene- 8 ous Emphysema (LIBERATE). Predictors of Response to Endobronchial Coil Therapy in Patients With Advanced Emphysema. 8 A Novel Laser Fiberscope for Simultaneous Imaging and Phototherapy of Peripheral Lung Cancer. 9 Articles selected and commented on by: Takeo Inoue and Masamichi Mineshita, Internal Medicine, Division of Respiratory Medicine, St. Marianna University School of Medicine, Japan Keep informed about the latest news and published articles in Respirology and Respirology Case Reports with direct links to the articles! Sign up to follow us on Twitter today! To advertise, subscribe a colleague or to unsubscribe please contact : Secretariat, Asian Pacific Society of Respirology, 2F, UK's Bldg. -

Top 20 Journals Relevant to Overall Health Care Services Ranked by Impact Factor
The following lists of journals have been provided as a resource to assist the Quality Improvement community in identifying high impact journals, and journals influential in specific topic areas relevant to QI efforts within health care. Identified journals publish papers by both traditional and open access publication processes. Top 20 journals relevant to overall health care services ranked by impact factor: Journal Name Impact Factor CA-A CANCER JOURNAL FOR CLINICIANS (supports open access) 137.578 NEW ENGLAND JOURNAL OF MEDICINE 59.558 LANCET (supports open access) 44.002 JAMA-JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION 37.684 NATURE MEDICINE 30.357 NATURE REVIEWS NEUROSCIENCE 29.298 LANCET ONCOLOGY (supports open access) 26.509 LANCET INFECTIOUS DISEASES (supports open access) 21.372 JOURNAL OF CLINICAL ONCOLOGY (supports open access) 20.982 BMJ-BRITISH MEDICAL JOURNAL (supports open access) 19.697 JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY (supports open access) 17.759 CIRCULATION (supports open access) 17.202 ANNALS OF INTERNAL MEDICINE 16.593 LANCENT DIABETES & ENDOCRINOLOGY (supports open access) 16.32 JAMA PSYCHIATRY 14.417 JAMA INTERNAL MEDICINE 14.00 PLOS MEDICINE (open access) 13.585 AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE 13.118 INTENSIVE CARE MEDICINE (supports open access) 10.125 Top 20 journals relevant to quality improvement in health care ranked by impact factor: Journal Name Impact Factor NEW ENGLAND JOURNAL OF MEDICINE 59.558 LANCET (supports open access) 44.002 JAMA-JOURNAL OF THE AMERICAN MEDICAL -

Erratum To: How to Choose the Best Journal for Your Case Report Richard A
Rison et al. Journal of Medical Case Reports (2017) 11:287 DOI 10.1186/s13256-017-1452-7 ERRATUM Open Access Erratum to: How to choose the best journal for your case report Richard A. Rison1,2*, Jennifer Kelly Shepphird3 and Michael R. Kidd4,5 Erratum In the publication of this article [1], there are two errors in Table 1 Case report journals. 1. The error: ‘The journal title BMJ Case Reports has no value in the PubMed Indexed column‘ Should instead read: ‘BMJ Case Reports in the PubMed Indexed column should have indicated “Yes”because it is PubMed indexed‘ 2. The error: ‘The journal title BMJ Case Reports has value “No” in the Open access column‘ Should instead read: ‘BMJ Case Reports in the Open access column should have indicated “Optional” because it does have an option for open access for an extra fee‘ This has now been included in this erratum. * Correspondence: [email protected] 1University of Southern California Keck School of Medicine, Los Angeles County Medical Center, 12401 Washington Blvd, Whittier, CA 90602, USA 2PIH Health Hospital-Whittier Stroke Center, PIH Health Hospital Non-Invasive Vascular Laboratory, 12401 Washington Blvd, Whittier, CA 90602, USA © The Author(s). 2017 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. -

Official Journal of the Asian Pacific Society of Respirology
Official Journal of the Asian Pacifi c Society of Respirology R e s p i r o l o g y Volume 24 û Supplement 1 û March 2019 Volume 24 Supplement 1 March 2019 TSANZSRS 2019 The Australia & New Zealand Society of Respiratory Science and The Thoracic Society of Australia and New Zealand (ANZSRS/TSANZ) Annual Scientifi c Meeting 29 March–2 April 2019 Gold Coast Convention and Exhibition Centre, QLD, Australia Disclaimer This abstract book has been produced using author-supplied copy. Editing has been restricted to some corrections of spelling and style where appropriate. The publisher assumes no responsibility for any claims, instructions, methods or drug dosages contained in the abstracts. It is recommended that these are verified independently. The contents contained herein are correct at the time of printing and may be subject to change. Contents ANZSRS Oral Abstracts New Investigators Awards (AO 001–AO 009) ANZSRS Oral Abstracts (AO 010–AO 018) ANZSRS Poster Abstracts ANZSRS Poster Abstracts (AP 001–AP 017) TSANZ Oral Abstracts TSANZ Ann Woolcock New Investigator Award (TO 001–TO 006) TSANZ Respiratory Nurses SIG Symposium 1 (TO 007–TO 008) TSANZ Respiratory Nurses SIG Symposium 3 (TO 009–TO 011) Cystic Fibrosis 1 (TO 012–TO 017) Evidence-Based Medicine and Practice (TO 018–TO 021) OLIV 1 (TO 022–TO 027) Primary Care / Palliative Care / Tobacco (TO 028–TO 033) Respiratory Infectious Diseases 1 (TO 034–TO 039) Asthma and Allergy 1 (TO 040–TO 045) Cell, Immunology and Molecular Biology of the Lung 1 (TO 046–TO 051) Chronic Obstructive Pulmonary -

Since January 2020 Elsevier Has Created a COVID-19 Resource Centre with Free Information in English and Mandarin on the Novel Coronavirus COVID- 19
Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information website. Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19 resource centre - including this research content - immediately available in PubMed Central and other publicly funded repositories, such as the WHO COVID database with rights for unrestricted research re-use and analyses in any form or by any means with acknowledgement of the original source. These permissions are granted for free by Elsevier for as long as the COVID-19 resource centre remains active. Journal Pre-proof Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations Wenlong Yao, Tingting Wang, Bailing Jiang, Feng Gao, Li Wang, Hongbo Zheng, Weimin Xiao, Li Xu, Shanglong Yao, Wei Mei, Xiangdong Chen, Ailin Luo, Liang Sun, Tim Cook, Elizabeth Behringer, Johannes M. Huitink, David T. Wong, Meghan Lane-Fall, Alistair McNarry, Barry McGuire, Andrew Higgs, Amit Shah, Anil Patel, Mingzhang Zuo, Wuhua Ma, Zhanggang Xue, Li-Ming Zhang, Wenxian Li, Yong Wang, Carin Hagberg, Ellen O’Sullivan, Lee A. Fleisher, Huafeng Wei, collaborators PII: S0007-0912(20)30203-8 DOI: https://doi.org/10.1016/j.bja.2020.03.026 Reference: BJA 1057 To appear in: British Journal of Anaesthesia Received Date: 27 March 2020 -

Source Subjects AA 27364 New Zealand Dental Journal Scopus
A B C Title Source Subjects ' ' : .. .. ... 1 A A 27364 New Zealand Dental Journal Scopus Dentistry ............... f 27365 New Zealand Economic Papers Scopus Economics, Econometrics and Finance 27366 New Zealand Engineering Scopus Business, Management and Accounting ............................... ‘ 27367 NEW ZEALAND ENTOMOLOGIST WoS & Scopus PLANT & ANIMAL SCIENCE ■■ .................... - 27368 New Zealand forestry Scopus Engineering 5* • “ n ---- — . —----- 27369 New Zealand Geographer WoS & Scopus SOCIAL SCIENCES, GENERAL 27370 New Zealand health & hospital Scopus Medicine 27371 New Zealand Hospital ■ y Scopus Medicine ___ NEW ZEALAND JOURNAL OF AGRICULTURAL 27372 RESEARCH WoS & Scopus AGRICULTURAL SCIENCES 27373 NEW ZEALAND JOURNAL OF BOTANY WoS & Scopus PLANT & ANIMAL SCIENCE NEW ZEALAND JOURNAL OF CROP AND 27374 HORTICULTURAL SCIENCE WoS & Scopus AGRICULTURAL SCIENCES 27375 NEW ZEALAND JOURNAL OF ECOLOGY WoS & Scopus ENVIRONMENT/ECOLOGY New Zealand Journal of Educational 27376 Studies Scopus Social Sciences New Zealand Journal of Experimental 27377 Agriculture Scopus Earth and Planetary Sciences Agricultural and Biological Sciences; Business, 27378 New Zealand Journal of Forestry Scopus Management and Accounting NEW ZEALAND JOURNAL OF FORESTRY 27379 SCIENCE WoS & Scopus PLANT & ANIMAL SCIENCE 27380 New Zealand Journal of Geography Scopus Earth and Planetary Sciences; Social Sciences NEW ZEALAND JOURNAL OF GEOLOGY AND 27381 GEOPHYSICS WoS GEOSCIENCES New Zealand Journal of Geology, and 27382 Geophysics Scopus Earth and Planetary