Diagnosis of Malaria in Pregnancy: a Comparison of Microscopy with Rapid Diagnostic Tests
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download .Pdf
University of Nigeria Virtual Library Serial No ISSN: NEXT ISSUE Author 1 SAMUEL, Efiong Sunday Author 2 Author 3 Widowhood Practices in Amaigbo Town of Title Nwangele Local Government Area Imo State Keywords Widowhood Practices in Amaigbo Town of Description Nwangele Local Government Area Imo State Category Health Education Nigeria Journal of Health Education Publisher Publication Date 2004 Signature • Page 99to.' /06 Widowhood Practices in Amaigbo Town of Nwangele Local Gove'rnment · Area, ImoBtate 1 . -, ' ' r •· • · ' . i " . i ~ · I " 1 I It) I( . ~ ,.,1, .1 " "' ' ' J l . , E.S. Samuel, Ph.D. Department of Health and Physical Education University of Nigeria, Nsukka Abstract menace of Umuada or Agada (93.3%). The . only widow-related 1l1e main purpose of the study was to inheritance right practiced was I determine the widowhood practices sharing the deceased properly among Jl in lfmaiglw town of Nwangele Local male cbildren. It miS recommended Government Area, lmo Stale. The that stale, public and private health survey research design was utilized agencies and religious organizations for the stucz)' and the main tool for should ca111paign against all . .Jj data co/lee/ion was the research's widowhood practices that are structured (//Aeslionnaire. 711e sample detrimental to health. I consisted of 300 widows selected by purposive sampling technique. The Widowhood refers to loss of a !: investigator and four assistants who spouse and according to Saba ( 1977) hailed ji-om the town collected the it is one of the events of life, which data. 7/w major findings of the study many women go through. It is a \\"ere as follows: mourning rituals tragedy, which befalls a married practiced the. -
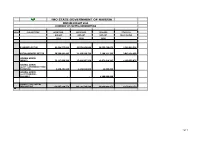
Imo State Government of Nigeria Revised Budget 2020 Summary of Capital Expenditure
IMO STATE GOVERNMENT OF NIGERIA REVISED BUDGET 2020 SUMMARY OF CAPITAL EXPENDITURE HEAD SUB-SECTORS APPROVED APPROVED REVISED COVID-19 BUDGET BUDGET BUDGET RESPONSIVE 2019 2020 2020 ECONOMIC SECTOR 82,439,555,839 63,576,043,808 20,555,468,871 2,186,094,528 SOCIAL SERVICES SECTOR 50,399,991,403 21,139,598,734 7,190,211,793 3,043,134,650 GENERAL ADMIN: (MDA'S) 72,117,999,396 17,421,907,270 12,971,619,207 1,150,599,075 GENERAL ADMIN: (GOVT COUNTERPART FUND PAYMENTS) 9,690,401,940 4,146,034,868 48,800,000 - GENERAL ADMIN: (GOVT TRANSFER - ISOPADEC) - - 4,200,000,000 - GRAND TOTAL CAPITAL EXPENDITURE 214,647,948,578 106,283,584,680 44,966,099,871 6,379,828,253 1of 1 IMO STATE GOVERNMENT OF NIGERIA IMO STATE GOVERNMENT OF NIGERIA REVISED BUDGET 2020 MINISTERIAL SUMMARY OF CAPITAL EXPENDITURE ECONOMIC SECTOR APPROVED 2019 APPROVED 2020 REVISED 2020 COVID-19 RESPONSIVE O414 MINISTRY OF AGRICULTURE AND FOOD SECURITY 1,499,486,000 2,939,000,000 1,150,450,000 - 0 AGRIC & FOOD SECURITY 1,499,486,000 0414-2 MINISTRY OF LIVESTOCK DEVELOPMENT 1,147,000,000 367,000,000 367,000,000 - 0 LIVESTOCK 1,147,000,000 697000000 1147000000 0414-1 MINISTRY OF ENVIRONMENT AND NATURAL RESOURCES 13,951,093,273 1,746,000,000 620,000,000 - 0 MINISTRY OF ENVIRONMENT 13951093273 450000000 O415 MINISTRY OF COMMERCE AND INDUSTRY 7,070,700,000 2,650,625,077 1,063,000,000 - -5,541,800,000 MINISTRY OF COMMERCE, INDUSTRY AND ENTREPRENEURSHIP1528900000 0419-2 MINISTRY OF WATER RESOURCES 2,880,754,957 2,657,000,000 636,869,000 - 1,261,745,492 MINISTRY OF PUBLIC UTILITIES 4,142,500,449 -

Science Education and Challenges of Globalization in Igbo Nation
US-China Education Review B, ISSN 2161-6248 February 2013, Vol. 3, No. 2, 116-127 D DAVID PUBLISHING Science Education and Challenges of Globalization in Igbo Nation Ezeudu F. O., Nkokelonye C. U., Adigwe J. C. University of Nigeria, Nsukka, Nigeria This paper reviewed the scientific contents in Igbo culture. Description of the Igbos who constitutes an ethnic group occupying southeastern Nigeria was made. It x-rayed the pre-colonial, colonial, and post-colonial culture of Igbo people and identified the scientific cultural activities, which can be harnessed to meet the challenges of modern day globalization. The advent of science and science education in Igbo culture and its applications in various cultural activities of the Igbos both in the pre-literate and post-literate era were discussed. The implications of these for the development of Igbo nation were examined and recommendations were made on how the scientific cultural activities can be improved to enhance the integration of the Igbo culture into the modern-day globalization. Keywords: Igbo, origin, culture, evolution, science education, colonial, globalization, challenges Introduction Igbo Origin and Cultural Evolution The Igbo nation is not to be introduced in the community of nations. The University of Nigeria, the first indigenous university in Africa, south of Sahara and north of the River Limpopo, is Igbo contribution to world civilization. From the 18th century, three Igbo patriots had acquired international fame and reputation (Afigbo, 1981, p. 145): (1) Olaudah Equiano -
The Example of Imo State; Nigeria
Waste Management as a Correlate of Environmental Sustainability in Sub- Saharan Africa: The example of Imo State, Nigeria Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades an der Julius- Maximilians-Universität Würzburg ABSTRACT If Sub-Saharan Africans understand the value of waste and handle it correctly and introduce “political hygiene” in governance, the issue of a filthy environment, unemployment, hunger, malnutrition and Vorgelegt von poverty will be greatly minimised. Nghengwa Ache Patience Juli 2019 Eingereicht am 10. Juli 2019 Von Nghengwa Ache Patience 1. Betreuerin Prof. Dr. Barbara Sponholz 2. Betreuer Prof. Dr. Roland Baumhauer 3. Betreuer Prof. Dr. Jürgen Rauh 1. Gutachterin Prof. Dr. Barbara Sponholz 2. Gutachter der Dissertation Prof. Dr. Jürgen Rauh 1. Prüfer Prof. Dr. Barbara Sponholz 2. Prüfer Prof. Dr. Jürgen Rauh 3.Tag der mündlichen Prüfung 14. Oktober 2019 (The quotation “political hygiene” was used by the Kenyan Professor - Patrick Loch Otieno Lumumba in Tanzania on June 29, 2017). (Cover picture: Oldest waste picker at the Old Road Landfill besides Nwaorie River Owerri, Imo State, Nigeria on February 9, 2017). “Africa must do her own growing, no matter how tall her neighbours are.” This work was completed with the assistance of the “DAAD STIBET Abschlussbeihilfe” I dedicate this work to waste pickers and waste users. Summary Introduction. Rapid and uncontrolled industrialisation and urbanisation in most developing countries are resulting in land, air and water pollution at rates that the natural environment cannot fully renew. These contemporary environmental issues have attracted local, national and international attention. The problem of urban garbage management is associated with rapid population growth in developing countries. -

List of Community Banks Converted to Microfinance Banks As at 31St
CENTRAL BANK OF NIGERIA IMPORTANT NOTICE LIST OF COMMUNITY BANKS THAT HAVE SUCESSFULLY CONVERTED TO MICROFINANCE BANKS AS AT DECEMBER 31, 2007 Following the expiration of December 31, 2007 deadline for all existing community banks to re-capitalize to a minimum of N20 million shareholders’ fund, unimpaired by losses, and consequently convert to microfinance banks (MFB), it is imperative to publish the outcome of the conversion exercise for the guidance of the general public. Accordingly, the attached list represents 607 erstwhile community banks that have successfully converted to microfinance banks with either final licence or provisional approval. This list does not, however, include new investors that have been granted Final Licences or Approvals-In- Principle to operate as microfinance banks since the launch of Microfinance Policy on December 15, 2005. The Central Bank of Nigeria (CBN) hereby states categorically that only the community banks on this list that have successfully converted to microfinance banks shall continue to be supervised by the CBN. Members of the public are hereby advised not to transact business with any community bank which is not on the list of these successfully converted microfinance banks. Any member of the public, who transacts business with any community bank that failed to convert to MFB does so at his/her own risk. Members of the public are also to note that the operating licences of community banks that failed to re-capitalize and consequently do not appear on this list, have automatically been revoked pursuant to Section 12 of BOFIA, 1991 (as amended). For the avoidance of the doubt, new applications either as a Unit or State Microfinance Banks from potential investors or promoters shall continue to be received and processed for licensing by the Central Bank of Nigeria. -

Water Quality Assessment of Nwangele River in Imo State, Nigeria
Journal of Ecobiotechnology 2019, 11: 1-5 doi: 10.25081/jebt.2019.v11.3866 http://updatepublishing.com/journal/index.php/jebt Research Article Water quality assessment of Nwangele river in Imo State, Nigeria Anudike Joseph1*, Duru Majesty2, Uhegbu Friday1 ISSN: 2077-0464 1Department of Biochemistry, Abia State University, Uturu, Nigeria, 2Department of Chemical Sciences (Biochemistry Unit), Rhema University, Aba, Nigeria. ABSTRACT Water quality assessment of Nwangele river was undertaken using standard methods. Water samples were drawn from upstream, midstream and downstream of the river and assessed for quality. Results obtained for physicochemical characteristics showed pH (4.83±.0.01-5.00±0.31), total solid (200.00±2.40-613.19±1.10 mg/L), and total suspended solid (49.98±0.11-399.04±2.09 mg/L). Heavy metals found in the river water were iron (0.132±0.01- 0.144±0.02 mg/L), zinc (0.034±0.02- 0.044±0.02 mg/L), mercury (0.004±0.001- 0.011±0.00 mg/L), lead (0.008±0.00- 0.016±0.00 mg/L) Received: November 12, 2018 and cadmium (0.03±0.01- 0.011±0.00 mg/L). Microbiological studies on the river revealed the presence of Klebsieilla Accepted: February 21, 2019 sp., Vibro sp., Pseudomonas sp., Proteus sp., Escherichia sp., Staphylococcus sp., Shigella sp., Bacillus sp., Serratia sp., Published: February 28, 2019 Citrobacter sp., and Enterobacter sp as bacterial isolates with high total heterotrophic bacteria count (THBC), total coliform count (TCC), Salmonella-shigella count (SSC), and total viable count (TVC). -

Environmental-And-Social-Impact-Assessment-For-The-Rehabilitation-And-Construction-Of
Public Disclosure Authorized FEDERAL REPUPLIC OF NIGERIA IMO STATE RURAL ACCESS AND MOBILITY PROJECT (RAMP-2) ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT (ESIA) Public Disclosure Authorized FOR Public Disclosure Authorized THE REHABILITATION/ CONSTRUCTION OF 380.1KM OF RURAL ROADS IN IMO STATE August 2019 Public Disclosure Authorized Final ESIA for the Rehabilitation of 88 Rural Roads in Imo State under RAMP-2 TABLE OF CONTENTS TABLE OF CONTENTS ..................................................................................................................... ii LIST OF TABLES .............................................................................................................................. vii LIST OF FIGURES ........................................................................................................................... viii LIST OF PLATES ............................................................................................................................. viii LIST OF ACRONYMS AND ABBREVIATIONS ........................................................................... ix EXECUTIVE SUMMARY .................................................................................................................. x CHAPTER ONE: INTRODUCTION ................................................................................................. 1 1.1 Background................................................................................................................................ 1 1.2 Project Development Objective -

Christianity, Colonialism and the Challenge of Nkwerre Blacksmithing Technological Culture, 1913 – 1960
CHRISTIANITY, COLONIALISM AND THE CHALLENGE OF NKWERRE BLACKSMITHING TECHNOLOGICAL CULTURE, 1913 – 1960 Uzoma Samuel Osuala* and Yakubu Soja Jibrin** Abstract The advent of Christianity paved way for colonialism in most parts of African communities. These two external variables – Christianity and colonialism – have in no small measures, transformed the communities they traversed. The advent of missionaries and the spread of the Christian faith were accompanied by colonial manipulations. Thus, Nkwerre, a small Igbo community with tradition of blacksmithing technological culture was caught up in Christian and colonial webs. The promising doctrines of Christianity, colonial legislations and the integration of Igboland into a capitalist economy stunted Nkwerre blacksmithing technology. Therefore, the paper appraises the role of the Siamese twin of Christianity and colonialism in the gradual disintegration of Nkwerre blacksmithing technological culture. It argues that African communities should be cautious to embrace Western culture. The data for this paper are derived from primary and secondary sources which include archival materials, journal articles, books and oral traditions. The methodology is narrative, thematic and adopted multidisciplinary approach. Keywords: Christianity, Colonialism, Nkwerre, Blacksmithing, Technology, Culture *Uzoma Samuel Osuala Department of History & Int’l Studies, Federal University Lokoja,Kogi State, Nigeria [email protected]/ [email protected] **Yakubu Soja Jibrin Department of History & Int’l Studies, Federal University Lokoja,Kogi State, Nigeria. KDJAS: Kenneth Dike Journal of African Studies, Vol. 1 (1), 2020. Introduction Nkwerre blacksmithing technology was acknowledged to have evolved from the manufacture of simple farm implements such as cutlasses, hoes, staples, among others farm and household equipment to gun production. As a result, Nkwerre town was usually addressed with the sobriquet, Nkwerre – Opia Egbe (Nkwerre, the gun manufacturer). -

Hydrogeophysical Evaluation of Aquifer of the Lower Orashi River
International Journal of Advanced Academic Research | Sciences, Technology and Engineering | ISSN: 2488-9849 Vol. 5, Issue 8 (August 2019) HYDROGEOPHYSICAL EVALUATION OF AQUIFER UNITS AROUND THE LOWER ORASHI RIVER AREA, SOUTHEASTERN NIGERIA 1MBAGWU E.C., 1IBENEME S.I., 1OKEREKE C.N AND 1EZEBUNANWA A.C. 1Department of Geology, Federal University of Technology Owerri, Imo State, Nigeria. Corresponding Authors: [email protected], [email protected] ABSTRACT Hydrogeophysical characteristics of the aquifers of the Lower Orashi River Area, Southeastern Nigeria was done using VES to delineate the aquifers and evaluate their geometric characteristics. The study area is underlain by the Ameki, Ogwashi and Benin Formations. The unconsolidated nature of the Formations and their high susceptibility to contamination have made this study imperative, as it would assist water resource planners and developers in the area to understand the best way to plan and site boreholes in the area. Eighty eight (88) Schlumberger Vertical Electrical Soundings (VES) were carried out in various parts of the study area with a maximum electrode separation (AB/2) of 350 m. The VES data were processed using a combination of curve matching techniques and computer iterative modeling. The study revealed seven to ten geo-electric layers with varying lithologies majorly sand units and a multiple aquifer system ranging from confined to unconfined aquifers. The results indicate that aquifer thickness ranges from 20m to about 227m. A quantitative interpretation of the curves -

Agulu Road, Adazi Ani, Anambra State. ANAMBRA 2 AB Microfinance Bank Limited National No
LICENSED MICROFINANCE BANKS (MFBs) IN NIGERIA AS AT SEPTEMBER 22, 2017 # Name Category Address State Description 1 AACB Microfinance Bank Limited State Nnewi/ Agulu Road, Adazi Ani, Anambra State. ANAMBRA 2 AB Microfinance Bank Limited National No. 9 Oba Akran Avenue, Ikeja Lagos State. LAGOS 3 Abatete Microfinance Bank Limited Unit Abatete Town, Idemili Local Govt Area, Anambra State ANAMBRA 4 ABC Microfinance Bank Limited Unit Mission Road, Okada, Edo State EDO 5 Abestone Microfinance Bank Ltd Unit Commerce House, Beside Government House, Oke Igbein, Abeokuta, Ogun State OGUN 6 Abia State University Microfinance Bank Limited Unit Uturu, Isuikwuato LGA, Abia State ABIA 7 Abigi Microfinance Bank Limited Unit 28, Moborode Odofin Street, Ijebu Waterside, Ogun State OGUN 8 Abokie Microfinance Bank Limited Unit Plot 2, Murtala Mohammed Square, By Independence Way, Kaduna State. KADUNA 9 Abubakar Tafawa Balewa University Microfinance Bank Limited Unit Abubakar Tafawa Balewa University (ATBU), Yelwa Road, Bauchi Bauchi 10 Abucoop Microfinance Bank Limited State Plot 251, Millenium Builder's Plaza, Hebert Macaulay Way, Central Business District, Garki, Abuja ABUJA 11 Accion Microfinance Bank Limited National 4th Floor, Elizade Plaza, 322A, Ikorodu Road, Beside LASU Mini Campus, Anthony, Lagos LAGOS 12 ACE Microfinance Bank Limited Unit 3, Daniel Aliyu Street, Kwali, Abuja ABUJA 13 Acheajebwa Microfinance Bank Limited Unit Sarkin Pawa Town, Muya L.G.A Niger State NIGER 14 Achina Microfinance Bank Limited Unit Achina Aguata LGA, Anambra State ANAMBRA 15 Active Point Microfinance Bank Limited State 18A Nkemba Street, Uyo, Akwa Ibom State AKWA IBOM 16 Acuity Microfinance Bank Limited Unit 167, Adeniji Adele Road, Lagos LAGOS 17 Ada Microfinance Bank Limited Unit Agwada Town, Kokona Local Govt. -

Assessing the Impact of Military Rule on Imo State, 1976-1999
International Journal of Research in Humanities and Social Studies Volume 2, Issue 9, September 2015, PP 40-53 ISSN 2394-6288 (Print) & ISSN 2394-6296 (Online) The Military in Politics: Assessing the Impact of Military Rule on Imo State, 1976-1999 Kelechi C. Ubaku1*, Emmanuel U. Ezeifedi1, Solomon S. Duru1 1Department of History and International Studies, Imo State University, Owerri, Nigeria ABSTRACT Nigeria is one of the nations of the world with a history of military domination in her political activities. The earliest incursion of the military in the political affairs of the African polity was encouraged by the upheavals which encrusted the political atmosphere of the country in the first republic. Traditionally, the acquisition of power by the military at the centre (federal level) automatically means the presence of the military at the helm of political affairs in the federating units, as military personnel were usually appointed as governors or administrators at the state level. Periodically, this trend was felt in Imo state from creation in 1976 through 1999 when the military officially relinquished power and recognized a democratically elected government in Nigeria. Numerous impacts were created on Imo state, during this period, by the various serving military governments in the administration of the state, and the examination of these impacts therefore forms the central discourse of this study. Adopting historical methodology of data gathering which encouraged ample utilization of primary and secondary sourced materials in the study, findings, however, revealed that in as much as the developmental woes of the state, within the stipulated period, was attributed to the political activities of the military governors – a maxim held and promoted presently in some quarters, there were still elements of benefits that accrued from the activities of military governments in Imo state. -

The Communicativeness of Incantations in the Traditional Igbo Society
Vol. 8(7),pp. 63-70, October 2016 DOI: 10.5897/JMCS2016.0512 Article Number: 3ABBDF561047 ISSN: 2141-2545 Journal of Media and Communication Studies Copyright ©2016 Author(s) retain the copyright of this article http://www.academicjournlas.org/JMCS Full Length Research Paper The communicativeness of incantations in the traditional Igbo society Walter Duru Department of Communication Arts, University of Uyo, Uyo, Nigeria. Received 06 June, 2016; Accepted 19 September, 2016 This paper examines the communicativeness of incantations in the traditional Igbo society. Incantations are given force by oral tradition, a practice whereby the social, political, economic and cultural heritage of the people is communicated by word of mouth from one generation to another. It was the most predominant part of communication in many parts of Africa. Prior to colonialism, the African society, including the Igbo used oral tradition as a veritable tool in information gathering, sharing/dissemination and indeed worship. They lived normal and satisfactory lives, cultivated, built, ate, sang, danced, healed their sick, created and communicated. Incantation is one of the modes of communication in the traditional Igbo society. In an incantation, all words stand for something and are meaningful. Most of the cultural displays of the Igbo society employ incantations in communicating with spirits. While some aspects of the practice may appear fetish and obsolete, several others are purely traditional and, destroying it out-rightly amounts to throwing away a baby with the dirty water. This article traces the effectiveness of incantation as a mode of communication, examines its uses and purposes, while highlighting the implications of allowing it go into extinction.