Dive Briefing - Decompression Sickness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Similan Islands 9 – 19 May 2021
THAILAND LIVEABOARD SIMILAN ISLANDS 9 – 19 MAY 2021 BOAT INFORMATION: Manta Queen 8 is running a 5 days & 5 nights trip to Thailands premier dive site - Similan Islands, Koh Bon, Koh Tachai, Surin Islands, Richelieu Rock and Boon Sung Wreck. The boat accommodates 24 guests in comfortable air conditioned double ensuite, twin ensuite, twin non ensuite cabins. The vessel is a 28 meters long and 7 meters wide wooden hull built boat that is manned with 5 dive staff and 6 boat crew. There is plenty of space to enjoy the time in between dives in the saloon with HD-TV, the open dining area or on the large sundeck. All meals on board are served buffet style freshly cooked by the on board chef. Snacks and fruits are served in between dives. The dinghy gives you the opportunity to spend some time on the beautiful beaches. DIVE - EAT - SLEEP – REPEAT DIVES SITE INFORMATION: RICHELIEU ROCK (called in Thai Hin Plo Naam) is a famous dive site in the Andaman Sea near the Surin Islands. The site is marked by the top with a pinnacle which is 1m above the sea level during low tide, and disappears underwater during high tide. The horseshoe-shaped reef was discovered by Jacques-Yves Cousteau and is known for its purple corals (it reminded Jacques Cousteau of Cardinal Richelieu´s purple robe) as well as diverse marine life ranging from small fish and harlequin shrimp to large pelagics like whale shark, manta ray, barracuda and grouper. The pinnacle falls steeply to the surrounding sand bottom at a maximum depth of 35m. -

Undercurrent, July 2013
The Private, Exclusive Guide for Serious Divers July 2013 Vol. 28, No. 7 WAOW, Indonesia fiery volcanoes, dangerous dragons and colorful diving Dear Fellow Diver: IN THIS ISSUE: Sixty feet down on my first dive, I quietly admired WAOW, Indonesia . 1. a barrel sponge the size of a smart car. Tiny white sea How Diving Inspires this cucumbers thrived in every nook and cranny. Then a thun- dering explosion ripped through the water. I quickly Science-Fiction Writer . 3. looked at my dive buddy. “What in the world was that?” A Bahamas, Hawaii, Red Sea . 5. thousand thoughts raced through my mind, but I guessed it might just be local fishermen dynamiting. I shrugged it Lawsuit over Diver Death at San off. Upon returning to the surface some 60 minutes later, Diego’s Yukon Wreck . .6 . I had my answer. A towering mushroom cloud billowed from the lip of a nearby volcanic crater. The tiny island of DEMA’s “Reaching Out” Award Palau Palue had just erupted. “Awesome,” I thought. “It is Not Worth Winning . 8. doesn’t get more primal than this.” I climbed the ladder into the rigid tender, and the driver returned us divers The Disappearing Dive Shop 10 to the mother craft. Fine volcanic ash rained down on us, Navy Divers Got It Wrong . 11. covering chairs, tables, stairs, everything. I could not have asked for a more unusual way to begin my 12 days of Shark Baiting and Feeding . 12. diving on the luxury liveaboard WAOW. Fiji Airways Reverses Its Stance That’s an acronym for Water Adventure Ocean Wide. -

A Coral-Safe Diving Reminder Reduces Reef Contacts by Ashton
PROTECTING GUAM’S CORAL REEFS BY IMPROVING SCUBA DIVER BEHAVIOR: A CORAL-SAFE DIVING REMINDER REDUCES REEF CONTACTS BY ASHTON N. WILLIAMS A thesis submitted in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE IN BIOLOGY SUPERVISORY COMMITTEE Dr. Laurie Raymundo, Chair Dr. Alexander Kerr, Member Dr. Romina King, Member UNIVERSITY OF GUAM DECEMBER 2019 Abstract Coral reefs are a critical resource for the culture and economy of the American territory of Guam, but the island’s coral reef resources are increasingly imperiled by climate change, particularly bleaching caused by rising seawater temperatures. Severe bleaching events in 2013, 2014, 2016, and 2017 have caused mass mortality of corals and made evident the critical need to reduce local stressors to protect the future of Guam’s reefs. An estimated 300,000 people scuba dive on Guam’s reefs annually, but the impacts of these divers are unknown. This study examines the impacts of scuba diving activity on highly trafficked coral reefs and tests a low-effort approach to reducing diver impacts by using a coral-safe diving reminder. Comparisons of benthic cover, genus diversity, and health impacts did not reveal any significant differences between pairs of often dived and rarely dived sites, although it is likely that the damage and mortality caused by recent bleaching events may be masking the smaller impacts of scuba divers. A single-sentence coral-safe diving reminder delivered as part of the standard pre-dive briefing was highly effective in reducing both accidental and intentional contacts with reef. Divers who received a coral-safe diving reminder made 72% fewer contacts with the reef, and about 60% fewer contacts with live corals specifically, than divers who did not receive a reminder. -

June 18-20, 2015 Annual Scientific Meeting
UNDERSEA & HYPERBARIC MEDICAL SOCIETY ANNUAL SCIENTIFIC MEETING HOTEL BONAVENTURE MONTREAL, CANADA JUNE 18-20, 2015 2015 UHMS Scientific Meeting June 18-20 Montreal, Canada TABLE OF CONTENTS Subject Page No. Disclosures ................................................................................................................................................................ 6-7 Schedule .................................................................................................................................................................. 8-13 Continuing Education ................................................................................................................................................ 13 Associates’ Breakout Schedule .................................................................................................................................. 14 Evaluation / MOC Credit Information ....................................................................................................................... 15 Committee Meetings .................................................................................................................................................. 16 Exhibitors .............................................................................................................................................................. 17-20 SESSIONS/ABSTRACTS THURSDAY GENERAL SESSION .............................................................................................................. 22-63 PRESIDENT’S -

Diving Procedures Manual
Diving Procedures Manual Emergency Contacts Flinders University Security (24hrs) (08) 8201 2880 University Diving Officer Matt Lloyd – 0414 190 051 or 8201 2534 Charlie Huveneers (S&E) – 0405 635 257 or 8201 2825 Faculty Diving Administrators John Naumann (EHL) – 0427 427 179 or 8201 5533 Associate Director, WHS 0414 190 024 WHS Unit (during office hours) 08 8201 3024 Diving Emergency Service 1800 088 200 Ambulance/Police 000 (112 on mobile) SES 132 500 UHF 1 Marine Radio VHF 16 2016 TABLE OF CONTENTS OVERVIEW ............................................................................................................................................................. 5 References .......................................................................................................................................5 Section 1 SCOPE AND Responsibilities ........................................................................................................... 6 1.1 Scope .....................................................................................................................................6 1.2 Responsibilities ......................................................................................................................6 1.2.1 Vice Chancellor ........................................................................................................6 1.2.2 Executive Deans .......................................................................................................6 1.2.3 Deans of School .......................................................................................................6 -

Safe Boating Guidelines
DIVE FLAGS HEALTH & DIVING REFERENCE SERIES When diving, fly the flag. Ensure the flags are stiff, 6 West Colony Place unfurled and in recognizable condition. Durham, NC 27705 USA SAFE BOATING PHONE: +1-919-684-2948 DIVER DOWN FLAG DAN EMERGENCY HOTLINE: +1-919-684-9111 GUIDELINES This flag explicitly signals that divers are in the water and should always be flown from a vessel or buoy when divers are in the water. When flown from a vessel, the diver down flag should be at least 20 inches by 24 inches and flown above the vessel’s highest point. When displayed from a buoy, the flag should be at least 12 inches by 12 inches. ALPHA FLAG Internationally recognized, this flag is flown when the mobility of a vessel is restricted, indicating that other vessels should yield the right of way. The alpha flag may be flown along with the diver down flag when divers are in the water. D SURFACE MARKER BUOYS I V When deployed during ascent, a E surface marker buoy (SMB) will make R a diver’s presence more visible. In B addition to a SMB, divers may also E L use a whistle or audible signal, a dive O light or a signaling mirror to notify W boaters of their location in the water. Part #: 013-1034 Rev. 3.27.15 REPORT DIVING INCIDENTS ONLINE AT DAN.ORG/INCIDENTREPORT. JOIN US AT DAN.ORG SAFE BOATING GUIDELINES To prevent injuries and death by propeller and vessel strikes, divers and boaters must be proactively aware of one another. -
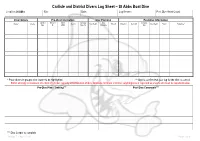
Carlisle and District Divers Log Sheet – St Abbs Boat Dive
Carlisle and District Divers Log Sheet – St Abbs Boat Dive Location: St Abbs Site: Date: Log Keeper: Post Dive Head Count: Diver Details Pre-Dive Information Dive Planning Post-Dive Information Cylinder Nitrox % Nitrox Aux Gas Max Aux Gas Name* Grade Gas In Max Depth Time In Duration Gas Out Max Depth Stops Signature** Size O2 MOD Size / In Duration Out * Place divers in groups; dive leader to be highlighted. ** Sign to confirm that your log for the dive is correct. BSAC strongly recommend one third of cylinder capacity at termination of dive. Absolute minimum is 40 bar; anything less is regarded as unsafe and must be reported below. Pre-Dive Plan / Training*** Post Dive Comments*** *** Dive Leader to complete Version 7 – April 2013 Page 1 of 4 Carlisle and District Divers Dive Specific Assessment – St Abbs Boat Dive Location: St Abbs Date: Dive Manager: Assistant Dive Manager: Location of Phones or Radios: UK Emergencies at Sea: First Aider / Oxygen Administrator: Deputy First Aider / Oxygen Administrator: Coastguard: VHF DSC / Channel 16 Lives in danger: Mayday, Mayday DCI: Pan, Pan Location of Nearest A&E Facility: UK Emergencies on Land: Location of First Aid and Oxygen Kits: Access to First Aid and Oxygen Kits: Berwick Infirmary, DCI: 07831 151523 Infirmary Square, Berwick-upon-Tweed, DCI Scotland: 0845 408 6008 Northumberland. TD15 1LT DCI: 999 / 112 (Coastguard) 0844 811 8111 Near Drowning: 999 / 112 (Ambulance) Approximately 13 miles Lost Diver: 999 / 112 (Police) Weather Forecast: Wind Direction / Speed: Air Temperature: Anticipated -

Leatherback Report Ana Bikik Odyssey Marine Technical Diving Illumination
Funky Gifts for Folks with Fins ... GirlDiver: Yoga & Diving Papua Leatherback Report Portfolio GLOBAL EDITION May 2009 Number 29 Ana Bikik Profile Odyssey Marine Tech Talk Technical Diving BIKINI ATOLL & KWAJALEIN ATOLL Photography Illumination Pacific1 X-RAY MAG : 29 : 2009 Wrecks COVER PHOTO BY JOOST-JAN WAANDERS DIRECTORY Join Kurt Amsler’s efforts to save Indonesia’s X-RAY MAG is published by AquaScope Media ApS endangered sea turtles. Sign the petition and Frederiksberg, Denmark donate to the cause at: www.sos-seaturtles.ch www.xray-mag.com PUBLISHER SENIOR EDITOR Team divers share a deco stop above the Saratoga, Bikini Atoll - Photo by Joost-Jan Waanders & EDITOR-IN-CHIEF Michael Symes Peter Symes [email protected] [email protected] SECTION EDITORS contents PUBLISHER / EDITOR Andrey Bizyukin, PhD - Features & CREATIVE DIRECTOR Arnold Weisz - News, Features Gunild Symes Catherine Lim - News, Books [email protected] Simon Kong - News, Books Mathias Carvalho - Wrecks ASSOCIATE EDITORS Cindy Ross - GirlDiver & REPRESENTATIVES: Cedric Verdier - Tech Talk Americas: Scott Bennett - Photography Arnold Weisz Scott Bennett - Travel [email protected] Fiona Ayerst - Sharks Michael Arvedlund, PhD Russia Editors & Reps: - Ecology Andrey Bizyukin PhD, Moscow [email protected] CORRESPONDENTS Robert Aston - CA, USA Svetlana Murashkina PhD, Moscow Enrico Cappeletti - Italy [email protected] John Collins - Ireland Marcelo Mammana - Argentina South East Asia Editor & Rep: Nonoy Tan - The Philippines Catherine GS Lim, Singapore [email protected] -

Give These Divers a Break!
GIVE THESE DIVERS A BREAK! As many people are well aware, two divers, Allyson Dalton and Richard Neely were rescued after being adrift for 19 hours off the Whitsunday Islands in Queensland. It is a credit to the Queensland emergency services that they were found reasonably swiftly once daylight was available. It is also a great relief that they were relatively unharmed. I have followed this story closely and with great interest, both as a long time diver and as Executive Director of the Divers Alert Network (DAN) Asia‐Pacific. DAN is a group of worldwide not‐for‐profit membership‐based organisations whose core mission involves striving to enhance the safety of diving for the recreational diving community. Divers Alert Network is not an insurance company. The organisation, on behalf of its members, sources appropriate insurance coverage from a variety of insurance providers around the world. All DAN members are automatically covered with up to US$100,000 Emergency Evacuation Coverage, no matter where in the world they are, for diving and non‐diving accidents or illnesses. In addition, members can choose to add dive injury insurance to their membership if required. This insurance is designed to pay for the medical costs associated with covered diving accidents. Allyson is a long time member of DAN America and Richard of DAN Europe. They are both experienced divers who have dived in various parts of the world. On this occasion they went for a day’s diving on a charter vessel. They had three uneventful dives followed by one that evolved into this drama. -
Diving Safe Practices Manual
Diving Safe Practices Manual Underwater Inspection Program U.S. Department of the Interior February 2021 Mission Statements The Department of the Interior conserves and manages the Nation’s natural resources and cultural heritage for the benefit and enjoyment of the American people, provides scientific and other information about natural resources and natural hazards to address societal challenges and create opportunities for the American people, and honors the Nation’s trust responsibilities or special commitments to American Indians, Alaska Natives, and affiliated island communities to help them prosper. The mission of the Bureau of Reclamation is to manage, develop, and protect water and related resources in an environmentally and economically sound manner in the interest of the American public. Diving Safe Practices Manual Underwater Inspection Program Prepared by R. L. Harris (September 2006) Regional Dive Team Leader and Chair Reclamation Diving Safety Advisory Board Revised by Reclamation Diving Safety Advisory Board (February 2021) Diving Safe Practices Manual Contents Page Contents .................................................................................................................................. iii 1 Introduction .............................................................................................................. 1 1.1 Use of this Manual ............................................................................................. 1 1.2 Diving Safety ..................................................................................................... -
Standards (Belize Standard: Code of Practice for Recreational Scuba Diving Services) (Declaration of Compulsory Standard) Order, 2016
BELIZE: STANDARDS (BELIZE STANDARD: CODE OF PRACTICE FOR RECREATIONAL SCUBA DIVING SERVICES) (DECLARATION OF COMPULSORY STANDARD) ORDER, 2016 ARRANGEMENT OF ORDER 1. Citation. 2. Declaration of Compulsory Standard. 3. Purpose of Compulsory Standard. Schedule. No. 57] Standards 1 BELIZE: STATUTORY INSTRUMENT No. 57 of 2016 ____________ AN ORDER made by the Minister responsible for the Belize Bureau of Standards, on the recommendation of the Belize Bureau of Standards, in exercise of the powers conferred upon him by section 9(2) of the Standards Act, Chapter 295 of the Substantive Laws of Belize Revised Edition 2011, and all other powers thereunto him enabling. (Gazetted 18th June, 2016) ____________ 1. This Order may be cited as the Citation. STANDARDS (BELIZE STANDARD: CODE OF PRACTICE FOR RECREATIONAL SCUBA DIVING SERVICES) (DECLARATION OF COMPULSORY STANDARD) ORDER, 2016. 2. The Belize Standard (BZ CP 5: 2016) – Code of Declaration of Compulsory Practice for Recreational Scuba Diving Services, which is Standard. set out in the Schedule is hereby declared to be a compulsory Schedule standard with effect from June 1, 2016. 3. The compulsory standard declared in paragraph 2 is Purpose of intended primarily to, Compulsory Standard. (a) protect the consumer or user against danger to health or safety; (b) to require adequate information to be given to the consumer or user; and (c) to ensure quality in any case where there is restriction in choice of source of supply. 2 Standards [No. 57 (Paragraph 2) SCHEDULE belize standard (bz CP 5: 2016) - CODE OF PRACTICE FOR RECREATIONAL SCUBA DIVING SERVICES FOREWORD 0.1 This standard specifies minimum requirements for the effective and operational safety of the scuba diving experience in Belize. -

2018 September;48(3):132−140
Diving and Hyperbaric Medicine The Journal of the South Pacific Underwater Medicine Society and the European Underwater and Baromedical Society Volume 48 No. 3 September 2018 Subclavian Doppler bubble monitoring Australian snorkelling and diving fatalities 2012 Inner ear barotrauma – a tool for diagnosis Which tooth restoration for divers? HBOT for large bowel anastomosis problems ISSN 2209-1491 (online); ISSN 1833-3516 (print) ABN 29 299 823 713 CONTENTS Diving and Hyperbaric Medicine Volume 48 No.3 September 2018 Editorials 198 Baltic Symposium on Diving and Hyperbaric Medicine 2018 129 The Editor’s offering Fiona Sharp 130 Decompression sickness, fatness and active hydrophobic spots Pieter Jan AM van Ooij Book review 199 Gas bubble dynamics in the human body Original articles John Fitz-Clarke 132 Reliability of venous gas embolism detection in the subclavian area for decompression stress assessment following scuba diving Julien Hugon, Asya Metelkina, Axel Barbaud, Ron Nishi, Fethi Bouak, SPUMS notices and news Jean-Eric Blatteau, Emmanuel Gempp 141 Provisional report on diving-related fatalities in Australian 201 ANZ Hyperbaric Medicine Group waters in 2011 Introductory Course in Diving John Lippmann, Chris Lawrence, Andrew Fock, Scott Jamieson and Hyperbaric Medicine 2019 168 Impact of various pressures on fracture resistance and 201 Australian and New Zealand microleakage of amalgam and composite restorations College of Anaesthetists Diving Elnaz Shafigh, Reza Fekrazad, Amir Reza Beglou and Hyperbaric Medicine Special 173 Meta-analysis