Nephritic Syndrome and Membranoproliferative Glomerulonephritis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Focal Segmental Glomerulosclerosis in Systemic Lupus Erythematosus
Relato de Caso Focal Segmental Glomerulosclerosis in Systemic Lupus Erythematosus: One or Two Glomerular Diseases? Glomerulosclerose Segmentar e Focal em Lúpus Eritematoso Sistêmico: Uma ou Duas Doenças? Rogério Barbosa de Deus1, Luis Antonio Moura1, Marcello Fabiano Franco2, Gianna Mastroianni Kirsztajn1 1 Nephrology Division and 2 Department of Pathology - Universidade Federal de São Paulo – EPM/UNIFESP- São Paulo. ABSTRACT Some patients with clinical and/or laboratory diagnosis of systemic lupus erythematosus (SLE) present with nephritis which from the morphological point of view does not fit in one of the 6 classes described in the WHO classification of lupus nephritis. On the other hand, nonlupus nephritis in patients with confirmed SLE is rarely reported. This condition may not be so uncommon as it seems. The associated glomerular lesions most frequently described are amyloidosis and focal segmental glomerulosclerosis (FSGS). We report on a 46 year-old, caucasian woman, who fulfilled the American College of Rheumatology criteria for SLE diagnosis: arthritis, positive anti-DNA, ANA, anti-Sm antibodies, and cutaneous maculae. During the follow-up, she presented arthralgias, alopecia, vasculitis, lower extremities edema and decreased serum levels of C3 and C4. Proteinuria was initially nephrotic, but reached negative levels. The serum creatinine varied from 0.7 to 3.0 mg/dl. The patient was submitted to the first renal biopsy at admission and to the second one, 3 years later, with diagnosis of minimal change disease and FSGS, respectively. No deposits were demonstrated by immunofluorescence. In the present case, we believe that the patient had SLE and developed an idiopathic disease of the minimal change disease-FSGS spectrum. -
What Is Lupus Nephritis
What is lupus nephritis (LN)? Lupus nephritis (LN) is inflammation of the kidney that occurs as a common symptom of systemic lupus erythematosus (SLE), also known as lupus. Proteins in the immune system called antibodies damage important structures in the kidney. ⅱ Why are the kidneys important? To understand how lupus nephritis damages the kidney, it is important to understand how the kidneys work. The kidneys’ main function is to filter out excess waste and water from the blood through the urine. Kidneys also balance the salts and minerals circulating in the blood, help control blood pressure and make red blood cells. So, when the kidneys are damaged or fail, they can’t do their job as well. As a result, the kidneys are not able to filter out waste and water into the urine causing it to stay in the blood. What are the signs and symptoms of LN? Signs to ask the doctor about include blood in the urine or foamy urine which can mean that there is excess protein. Other signs to notice are swelling of legs, ankles, hands or tissue around the eyes as well as weight gain that can be caused by fluid the body isn’t getting rid of. ⅲ Symptoms of lupus nephritis also include high blood pressure, joint/muscle pain, high levels of waste (creatinine) in the blood, or impaired/failing kidney. ⅳ How common is LN? Lupus nephritis is the most common complication of lupus. Five out of 10 adults with lupus will have lupus nephritis, while eight out of 10 children with lupus will have kidney damage, which usually stems from lupus nephritis. -

Risk of Renal Function Decline in Patients with Ketamine-Associated Uropathy
International Journal of Environmental Research and Public Health Article Risk of Renal Function Decline in Patients with Ketamine-Associated Uropathy Shih-Hsiang Ou 1,2,3, Ling-Ying Wu 4, Hsin-Yu Chen 1,2, Chien-Wei Huang 1,2, Chih-Yang Hsu 1,2, Chien-Liang Chen 1,2 , Kang-Ju Chou 1,2, Hua-Chang Fang 1,2 and Po-Tsang Lee 1,2,* 1 Division of Nephrology, Department of Internal Medicine, Kaohsiung Veterans General Hospital, Kaohsiung 813, Taiwan; [email protected] (S.-H.O.); [email protected] (H.-Y.C.); [email protected] (C.-W.H.); [email protected] (C.-Y.H.); [email protected] (C.-L.C.); [email protected] (K.-J.C.); [email protected] (H.-C.F.) 2 Faculty of Medicine, School of Medicine, National Yang-Ming University, Taipei 112, Taiwan 3 Graduate Institute of Clinical Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung 807, Taiwan 4 Department of Obstetrics and Gynecology, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung 833, Taiwan; [email protected] * Correspondence: [email protected]; Tel.: +886-7342-2121 (ext. 8090) Received: 8 August 2020; Accepted: 29 September 2020; Published: 4 October 2020 Abstract: Ketamine-associated diseases have been increasing with the rise in ketamine abuse. Ketamine-associated uropathy is one of the most common complications. We investigated the effects of ketamine-associated uropathy on renal health and determined predictors of renal function decline in chronic ketamine abusers. This retrospective cohort study analyzed 51 patients (22 with ketamine- associated hydronephrosis and 29 with ketamine cystitis) from Kaohsiung Veterans General Hospital in Taiwan. -

Acute Nephritis. (Diffuse)
Postgrad Med J: first published as 10.1136/pgmj.13.136.39 on 1 February 1937. Downloaded from February, 1937 CLASSIFICATION OF NEPHRITIS 39 CLASSIFICATION OF NEPHRITIS. By JOHN GRAY, M.D. (Reader in Pathology, British Post-Graduate Medical School.) In some ways, classification of nephritis is a rather discouraging, as well as a difficult, task, for it is likely that with fuller knowledge of causation we will eventually be enabled to improve on and to simplify any classification possible at present. In the meantime, it is very difficult to decide on the respective merits of the numerous classifications suggested. On the other hand, however, it is true that the multiplicity of the terms which have been used to define various groups of nephritic cases rather tends to exaggerate the number of really important differences of opinion. Many opposing terms in use imply little fundamental difference of opinion, and simply indicate a preference for some particular label for a given type of case. On many points there is, except for this question of nomenclature, fairly general agreement, and it is perhaps as well to begin by indicating some of these, before entering on any discussion of those of a more controversial nature. Few, for instance, would object to the statement that the terms acute, sub- acute, and chronic nephritis provide a useful primary grouping for the majority Protected by copyright. of cases of true nephritis; nor, one thinks, would many take exception to the statement that, of the allied diseases which must be considered with nephritis, easily the most important is non-nephritic hypertension-whatever term is used to describe that condition. -

The Nephrotic Syndrome in Early Infancy: a Report of Three Cases* by H
Arch Dis Child: first published as 10.1136/adc.32.163.167 on 1 June 1957. Downloaded from THE NEPHROTIC SYNDROME IN EARLY INFANCY: A REPORT OF THREE CASES* BY H. McC. GILES, R. C. B. PUGH, E. M. DARMADY, FAY STRANACK and L. I. WOOLF From the Department of Paediatrics, St. Mary's Hospital, The Hospital for Sick Children, Great Ormond Street, London, and the Central Laboratory, Portsmouth (RECEIVED FOR PUBLICATION, DECEMBER 12, 1956) The nephrotic syndrome is characterized by evidence of genetic aetiology inasmuch as two of generalized oedema, hypoproteinaemia with diminu- the infants were brother and sister and both sets of tion or reversal of the albumin/globulin ratio, hyper- parents were cousins. Further points of interest lipaemia and gross albuminuria. Haematuria is not were the demonstration of anisotropic crystalline prominent; hypertension and azotaemia, except in material in alcohol-fixed tissues from all three the terminal stages, are slight and transient and infants, and the discovery on renal microdissection often do not occur at all. Recognition of this of lesions of the proximal tubule recalling those syndrome presents no difficulty but in many cases, found in Fanconi-Lignac disease (cystinosis). particularly in childhood, its cause remains obscure. Occasionally certain drugs such as troxidone or mercury, or certain diseases such as amyloidosis, Case Reports pyelonephritis, diabetes, disseminated lupus erythe- The parents of the first two patients (and the paternal copyright. matosus or renal vein thrombosis, can be in- grandparents) are first cousins. They, and a sister born criminated. In cases which develop renal failure three years before the first of her affected siblings, have and come to necropsy the lesions of glomerulo- been investigated in detail and show no sign of renal II disease. -

Chapter 10: Radiation Nephropathy
Chapter 10: Radiation Nephropathy † Amaka Edeani, MBBS,* and Eric P. Cohen, MD *Kidney Diseases Branch, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland; and †Nephrology Division, Department of Medicine, University of Maryland School of Medicine, and Baltimore Veterans Affairs Medical Center, Baltimore, Maryland INTRODUCTION Classical radiation nephropathy occurred after external beam radiation for treatment of solid The occurrence of renal dysfunction as a consequence cancers such as seminomas (6); the incidence has of ionizing radiation has been known for more than declined with the advent of more effective chemo- 100 years (1,2). Initial reports termed this condition therapy. In recent years, radiation nephropathy has “radiation nephritis,” but that is a misnomer, because occurred due to TBI used as part of chemo-irradiation it is not an inflammatory condition. Renal radiation conditioning just before hematopoietic stem cell injury may be avoided by the exclusion of an ade- transplantation (HSCT) and also from targeted ra- quate volume of kidney exposure during radiation dionuclide therapy used for instance in the treatment therapy, but the kidneys’ central location can make of neuroendocrine malignancies. TBI may be myelo- this difficult to impossible when tumors of the abdo- ablative or nonmyeloablative, with myeloablative men or retroperitoneum are treated, or during total regimens using radiation doses of 10–12 Gy to de- body irradiation (TBI) (3). stroy or suppress the recipient’s bone marrow. These doses are given in a single fraction or in nine fractions over 3 days (4). In addition, TBI for bone marrow BACKGROUND/CLINICAL SIGNIFICANCE transplantation (BMT) is preceded or accompanied by cytotoxic chemotherapy, which potentiates the Radiation nephropathy is renal injury and loss of effects of ionizing radiation (7). -

People with Lupus Are Much More Likely to Have Kidney Disease Than People Who Don't Have Lupus
Lupus and kidney disease What does kidney disease have to do with lupus? People with lupus are much more likely to have kidney disease than people who don't have lupus. The kidneys are the organs that make urine. Kidneys filter the blood by putting the waste products into the urine where they can leave the body. Kidney disease can cause blood and protein in the urine, swelling of the body, high blood pressure, and other symptoms. "Lupus nephritis" is the medical name for a type of kidney disease in people with lupus. People who have lupus can also get kidney disease caused by other problems. For example, if someone with lupus also has diabetes, the diabetes might be the cause of kidney problems. The way we find out is by doing a kidney biopsy. Types of Lupus Nephritis: There are several types or “classes” of lupus nephritis. They range from Class I to Class 6: Class 1 disease is mild, Classes 2 and 5 are moderate Classes 3 and 4 are aggressive, Class 6 indicates severe non-reversible disease. What are the symptoms of lupus nephritis? Foamy Urine- This is often one of the first signs of lupus nephritis Blood in the Urine- This is also often one of the first signs of lupus nephritis Swelling- Usually in the legs, feet, or ankles and less often in the hands or face. This tends to worsen as the day progresses or after sitting (this is called edema) High Blood Pressure Changes in Frequency of Urination– Either much more or much less Vomiting- Toxins that build up because the kidney is unable to remove them from the body can result in abnormal function of the liver and the process of digestion. -
Nephritis Fact Sheet
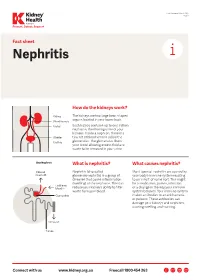
Last Reviewed March 2017 Page 1 Prevent, Detect, Support. Fact sheet Nephritis How do the kidneys work? The kidneys are two large bean-shaped organs located in your lower back. Each kidney contains up to one million nephrons, the filtering units of your kidneys. Inside a nephron, there is a tiny set of blood vessels called the glomerulus. The glomerulus filters your blood allowing excess fluid and waste to be removed in your urine. What is nephritis? What causes nephritis? Nephritis (also called Most types of nephritis are caused by glomerulonephritis) is a group of your body’s immune system reacting diseases that cause inflammation to an ‘insult’ of some sort. This might (swelling) of the nephrons. This can be a medication, poison, infection reduce your kidney’s ability to filter or a change in the way your immune waste from your blood. system behaves. Your immune system makes antibodies to attack bacteria or poisons. These antibodies can damage your kidneys and nephrons, causing swelling and scarring. Connect with us www.kidney.org.au Freecall 1800 454 363 Kidney Health Australia Nephritis Last Reviewed March 2017 Prevent, Detect, Support. Page 2 What are the different types of nephritis? There are many different types of Different types of nephritis include: Nephrotic syndrome: Damage to the nephritis. It can vary from a mild, nephrons causes them to leak large Focal nephritis: Less than a half of non-damaging condition to a serious amounts of protein into your urine your nephrons have scarring, and problem causing kidney failure. Some but little blood. Losing this protein blood and a small amount of protein types of nephritis appear mild at means your body does not have are found in your urine. -

The Impact of Chronic Kidney Disease in West Virginia
THE IMPACT OF CHRONIC KIDNEY DISEASE IN WEST VIRGINIA Joe Manchin III Governor Martha Yeager Walker Secretary Department of Health and Human Resources April 2006 West Virginia Bureau for Public Health Chris Curtis, MPH Acting Commissioner Catherine Slemp, MD, MPH Acting Medical Officer Joe Barker, MPA Director, Office of Epidemiology and Health Promotion Daniel M. Christy, MPA Director, Health Statistics Center Report Written By Eugenia Thoenen West Virginia Kidney Advisory Group Peggy J. Adams, MSN, RN, CDE Daniel M. Christy, MPA James C. Doria Mary Emmett, PhD Marie Gravely, MA, RD, LD, CDE Derrick Latos, MD, MACP Tammie Mitchell, RN, BSN, CNN Cecil Pollard, MA Rebecca Schmidt, DO, FACP, FASN Henry Taylor, MD, MPH Jessica Wright, RN, MPH Health Statistics Center James C. Doria, Program Manager, Statistical Services Unit Fred King, BRFSS Coordinator Thomas A. Leonard, MS, Programmer/Analyst Tom Light, Programmer Additional Acknowledgments Jay Eckhart, Health Data Analyst West Virginia Health Care Authority ii Executive Summary General Facts ● The kidneys are the chemists of our bodies. They have three main functions: (1) remove waste products, (2) balance our bodies’ chemicals, and (3) produce essential hormones. ● The kidneys filter approximately 50 gallons of blood every day; in general, a healthy adult will eliminate approximately one to two quarts of urine daily. If the kidneys do not function properly, wastes accumulate in the body. The progressive loss of kidney function eventually leads to end-stage renal disease (ESRD), or kidney failure, resulting in the need for either dialysis or kidney transplantation. ● The National Kidney Foundation (NKF) estimates that 1 in every 9 adults in the United States, more than 20 million people, has chronic kidney disease (CKD) and that more than 20 million others are at increased risk for the disease. -

Pyelonephritis.Pdf
Article renal Pyelonephritis William V. Raszka, Jr, Objectives After completing this article, readers should be able to: MD,* Omar Khan, MD† 1. Describe the epidemiology of urinary tract infections and pyelonephritis in children. 2. Discuss the risk factors for the development of pyelonephritis. Author Disclosure 3. Compare and contrast methods to diagnose urinary tract infection and pyelonephritis Drs Raszka and Khan in children. did not disclose any 4. Describe the management of pyelonephritis. financial relationships 5. Explain the long-term complications of pyelonephritis. relevant to this article. Introduction The frequency of urinary tract infections (UTIs) is second only to that of respiratory tract infections in the pediatric population. UTIs often are separated into infections of the lower urinary tract that involve the bladder and urethra and those of the upper tract that involve the kidneys, renal pelvis, and ureters. Infections of the upper tract are designated pyelo- nephritis. A complicated UTI, whether of the upper or lower tract, usually is associated with an underlying condition that increases the likelihood of a therapeutic failure. Underlying conditions include abnormal anatomy, urologic dysfunction, the presence of an indwelling catheter, or isolation of a multiresistant organism. Epidemiology Although the prevalence of UTI has been studied in a variety of patient populations, there are fewer data regarding the prevalence of pyelonephritis due, in part, to the difficulty in distinguishing upper from lower tract disease. The prevalence of UTI is influenced by factors such as age, sex, population sample, urine collection method, testing methodolo- gies, diagnostic criteria, and culture. Age and sex are the most important factors. -

Redalyc.Nephritic Syndrome Associated to Skin Infection
Colombia Médica ISSN: 0120-8322 [email protected] Universidad del Valle Colombia Barrios, Emil Julio; Guerrero, Gustavo Adolfo Nephritic syndrome associated to skin infection, hepatitis A, and pneumonia: a case report Colombia Médica, vol. 41, núm. 2, abril-junio, 2010, pp. 171-175 Universidad del Valle Cali, Colombia Available in: http://www.redalyc.org/articulo.oa?id=28316817009 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Colombia Médica Vol. 41 Nº 2, 2010 (Abril-Junio) Nephritic syndrome associated to skin infection, hepatitis A, and pneumonia: a case report EMIL JULIO B ARRIOS, MD1, G USTAVO ADOLFO G UERRERO, MD2 SUMMARY Introduction: Glomerulonephritis is the most common cause of acute and chronic renal disease. The prototype of acute glomerulonephritis is acute post-infectious glomerulonephritis. Recently, increased cases of glomerulopathy have been associated with bacterial, viral, and other infections. Acute nephritic syndrome is part of glomerulonephritis with an acute beginning, characterized by hematuria, hypertension, edema, and oliguria due to the reduction of glomerular filtration reflected in an increase of nitrogen compounds. Development: This paper shows a male infant at 2 years and 7 months of age with nephritic syndrome associated to a skin infection, pneumonia, and hepatitis A virus infection. Conclusion: Acute glomerulonephritis may be associated to streptococcus or another coincidental infection. Children with skin infection, hepatitis A, or pneumonia who reveal abnormal urinalysis, hypertension, azotemia, or oliguria should be evaluated for concomitant glomerulonephritis. -

Megalocytic Interstitial Nephritis Following Acute Pyelonephritis with Escherichia Colibacteremia: a Case Report
CASE REPORT Nephrology http://dx.doi.org/10.3346/jkms.2015.30.1.110 • J Korean Med Sci 2015; 30: 110-114 Megalocytic Interstitial Nephritis Following Acute Pyelonephritis with Escherichia coli Bacteremia: A Case Report Hee Jin Kwon,1 Kwai Han Yoo,1 Megalocytic interstitial nephritis is a rare form of kidney disease caused by chronic In Young Kim,1 Seulkee Lee,1 inflammation. We report a case of megalocytic interstitial nephritis occurring in a 45-yr- Hye Ryoun Jang,2 and Ghee Young Kwon3 old woman who presented with oliguric acute kidney injury and acute pyelonephritis accompanied by Escherichia coli bacteremia. Her renal function was not recovered despite 1Department of Medicine, 2Division of Nephrology, Department of Medicine, and 3Department of adequate duration of susceptible antibiotic treatment, accompanied by negative Pathology, Samsung Medical Center, Sungkyunkwan conversion of bacteremia and bacteriuria. Kidney biopsy revealed an infiltration of University School of Medicine, Seoul, Korea numerous histiocytes without Michaelis-Gutmann bodies. The patient’s renal function was markedly improved after short-term treatment with high-dose steroid. Received: 24 April 2014 Accepted: 27 August 2014 Keywords: Acute Kidney Injury; Megalocytic Interstitial Nephritis; Interstitial Nephritis Address for Correspondence: Hye Ryoun Jang, MD Division of Nephrology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 135-710, Korea Tel: +82.2-3410-0782, Fax: +82.2-3410-3849 E-mail: [email protected] INTRODUCTION serum creatinine level of 6.80 mg/dL, high C-reactive protein level of 24.61 mg/dL, and high procalcitonin level of 39.05 ng/ Megalocytic interstitial nephritis is a rare form of chronic renal mL.