Defining the Frontiers of Bioengineering Education at Illinois and Beyond
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2013 NCI Alliance for Nanotechnology in Cancer Annual Bulletin EDITOR-IN-CHIEF
2013 NCI Alliance for Nanotechnology in Cancer Annual Bulletin EDITOR-IN-CHIEF Piotr Grodzinski (NCI) SENIOR EDITOR Stephanie A. Morris (NCI) ASSOCIATE EDITOR(S) Dorothy Farrell (NCI) Lynn Hull (NCI) Mary Spiro (JHU) CONTRIBUTORS Martha Alexander (Rice CNPP) Michelle Berny-Lang (NCI) Dorothy Farrell (NCI) Emily Greenspan (NCI) Piotr Grodzinski (NCI) George Hinkal (NCI) Brenda Hugot (Boston CNTC) Lynn Hull (NCI) Contents Hannah Kim (Texas CCNE) 1 Introduction Julia Ljubimova (Cedars-Sinai CNPP) NIH Funding Opportunities Extend the Range Laura A. Miller (UIUC CNTC) 2 of Cancer Nanotechnology in Biomedical Research Sarah H. Petrosko (Northwestern CCNE) Mary Spiro (Johns Hopkins CCNE & CNTC) 6 Alliance Working Groups Provide Their Opinions to the Nanotechnology Community Li Tang (UIUC CNTC) Biana Godin Vilentchouk (Texas CCNE) 8 Crowdsourcing and the Dialogue Matthew Ware (Texas CCNE) on Nanotechnology in Cancer 9 Nano in the News DESIGN Danielle Peterson, Brio Design 12 Alliance Transitions INTRODUCTION BY DOROTHY FARRELL The third year of Phase II of the NCI Alliance for Nanotechnology These efforts included crowdsourcing strategies coordinated in Cancer was a busy and productive one for the Alliance. through a dedicated website (nanocancer.ideascale.com) and a Our investigators published over 300 papers in 2013, bringing Request for Information on the Directions and Needs for Cancer the total number of Alliance publications over the past three Nanotechnology (grants.nih.gov/grants/guide/notice-files/ years to approximately 1,100. Alliance research continues to NOT-CA-13-017.html). The insights gained through these forums be high profile and high impact, as measured by the quality are discussed in the Crowdsourcing section of the Bulletin. -
2009 NIH Director's Transformative Research Award Reviewers
2009 NIH Director’s Transformative Research Award Reviewers Editorial Board Members Chairs David Botstein Keith Robert Yamamoto Princeton University University of California, San Francisco Members John T. Cacioppo Myron P. Gutmann University of Chicago Inter-University Consortium for Political and Social Research Aravinda Chakravarti Johns Hopkins School of Medicine Nola M. Hylton-Watson University of California, San Francisco Garret A. Fitzgerald Cecil B. Pickett University of Pennsylvania Biogen Idec Alfred G. Gilman Susan S. Taylor University of Texas Southwestern Medical University of California at San Diego Center Michael J. Welsh University of Iowa Mail Reviewers Craig Kendall Abbey Margaret Ashcroft University of California, Santa Barbara Division of Medicine Samuel Achilefu Richard Herbert Aster School of Medicine Blood Research Institute Manuel Ares Arleen D. Auerbach University of California Rockefeller University Bruce A. Armitage J. Thomas August Carnegie Mellon University Johns Hopkins University Mark A. Arnold Kevin A. Ault University of Iowa Emory University School of Medicine David C. Aron Jennifer Bates Averill Case Western Reserve University University of New Mexico 1 Mary Helen Barcellos-Hoff Leslie A. Bruggeman New York University School of Medicine Case Western Reserve University David P. Bartel Peter Burkhard New Cambrige Center University of Connecticut Ralf Bartenschlager Alma L. Burlingame University of Heidelberg University of California, San Francisco Rashid Bashir Frederic D. Bushman University of Illinois at Urbana – Champaign University of Pennsylvania Carl A. Batt Robert William Caldwell Cornell University Medical College of Georgia Mark T. Bedford Phil Gordon Campbell Research Division Carnegie Mellon University Kevin D. Belfield Joseph Nicholas Cappella University of Central Florida University of Pennsylvania Andrew Steven Belmont William A. -
Celebration of Teaching Program
Celebration of Teaching April 16, 2021 · Zoom · 1:00-3:00pm Program WELCOME & INTRODUCTION OF DEAN RASHID BASHIR Jay Mann, Director of AE3 REMARKS Rashid Bashir, Dean KEYNOTE ADDRESS Dr. Gilda Barabino President, Olin College of Engineering COLLINS SCHOLAR REFLECTION AND RECOGNITION Chris Migotsky, Faculty Teaching Programs Coordinator & Jay Mann Eleftharia Kontou (2019-2020) & Brad Solomon (2020-2021) CELEBRATING EXCELLENCE IN ENGINEERING EDUCATION Jonathan Makela, Associate Dean & Jay Mann SIIP POSTER SESSION Rashid Bashir Dean, Grainger College of Engineering Rashid Bashir is Dean of The Grainger College of Engineering, the Grainger Distinguished Chair in Engineering and Professor of Bioengineering at the University of Illinois at Urbana-Champaign (UIUC). He received the NSF Faculty Early Career Award, the 2012 IEEE EMBS Technical Achievement Award, the Pritzker Distinguished Lectureship Award from BMES in 2018, and the 2021 American Institute for Medical and Biological Engineering Professional Impact Award. He has been involved in 3 startups that have licensed his technologies. He was part of the core founding team and co-chair of the curriculum committee for the Carle Illinois College of Medicine. His research group is interested in developing new technologies for precision and personalized medicine, and 3D bio-fabrication of cellular systems. Using bionanotechnology, BioMEMS, and lab on chip, he is working at the interface of biology and engineering from the molecular to the tissue scale, and aiming to make an impact on grand challenges in health and medicine. Dr. Gilda Barabino President, Olin College of Engineering Gilda A. Barabino is President of Olin College of Engineering, and Professor of Biomedical and Chemical Engineering. -

The Center for Food Safety Engineering G
The Center for Food Safety Engineeringg 2007 - 2008 Research Report “Collaborating to make our food safer” The mission of the Center for Food Safety Engineering is to develop new knowledge, technologies and systems for detection and prevention of chemical and microbial contamination of foods. Through CFSE, Purdue University positions itself as a national leader in multi- disciplinary food safety research. Our multi- disciplinary approach, including a strong engineering component, makes Purdue University truly unique. 2007-2008 Research Report 2 Welcome from the Director • Message from Richard Linton, Center Director 2 Message from USDA • Message from our Partnership with USDA-ARS 3 Multipathogen screening using immunomicroarray • Arun Bhunia 4 Optical biosensors for food pathogen detection • Arun Bhunia 5 Optical forward scattering for bacterial colony differentiation and identifi cation • Arun Bhunia, E. Daniel. Hirleman, J. Paul Robinson 6 Immunocapture real-time PCR to detect mycotoxigenic mold spores in grains • Maribeth A. Cousin, Charles P. Woloshuk 7 Detection of foodborne pathogens via an integrated spectroscopy and biosensor-based approach • Joseph Irudayaraj, Lisa Mauer, Chitrita DebRoy, Pina Fratamico 8 Nanoparticle-based DNA-multiplexed probes for pathogen detection using confocal raman microscopy • Joseph Irudayaraj 9 Engineering of biosystems for the detection of Listeria monocytogenes in foods • Michael R. Ladisch, Rashid Bashir, Arun Bhunia, J. Paul Robinson 10 Spotlight on USDA-ARS Scientists 12 Rapid, quantitative, and -

For Characterization of Mass of Single Live Cells in Fluids Kidong Park Purdue University, [email protected]
Purdue University Purdue e-Pubs Birck and NCN Publications Birck Nanotechnology Center 6-11-2008 'Living cantilever arrays' for characterization of mass of single live cells in fluids Kidong Park Purdue University, [email protected] Jaesung Jang Department of Mechanical Engineering, Chung-Ang University Daniel Irimia Massachusetts Gen oH sp, Shriners Hosp Children, Ctr Engn Med & Surg Serv, BioMEMS Resource Ctr Jennifer Sturgis Purdue University, [email protected] James Lee Ohio State Univ, Dept Chem Engn See next page for additional authors Follow this and additional works at: https://docs.lib.purdue.edu/nanopub Park, Kidong; Jang, Jaesung; Irimia, Daniel; Sturgis, Jennifer; Lee, James; Robinson, J. Paul; Toner, Mehmet; and Bashir, Rashid, "'Living cantilever arrays' for characterization of mass of single live cells in fluids" (2008). Birck and NCN Publications. Paper 147. https://docs.lib.purdue.edu/nanopub/147 This document has been made available through Purdue e-Pubs, a service of the Purdue University Libraries. Please contact [email protected] for additional information. Authors Kidong Park, Jaesung Jang, Daniel Irimia, Jennifer Sturgis, James Lee, J. Paul Robinson, Mehmet Toner, and Rashid Bashir This article is available at Purdue e-Pubs: https://docs.lib.purdue.edu/nanopub/147 Volume 8 | Number 7 | 2008 Miniaturisation for chemistry, biology & bioengineering www.rsc.org/loc Volume 8 | Number 7 | July 2008 | Pages 993–1228 Lab on a Chip Featuring research from the “Applied Miniaturisation Laboratory” As featured in: of Professor Chris Backhouse, University of Alberta, Canada. Miniaturisation for chemistry, biology & bioengineering www.rsc.org/loc Volume 8 | Number 7 | July 2008 | Pages 993–1228 Title: Electrically controlled microvalves to integrate microchip polymerase chain reaction and capillary electrophoresis. -
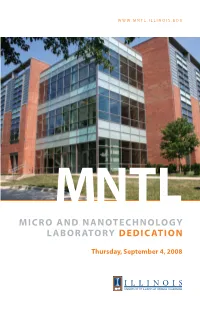
Micro and Nanotechnology Laboratory Dedication
WWW.MNTL.ILLINOIS.EDU MNTL MICRO AND NANOTECHNOLOGY LABORATORY DEDICATION Thursday, September 4, 2008 UNIVERSITY OF ILLINOIS AT URBANA-CHAMPAIGN MNTL MICRO AND NANOTECHNOLOGY LABORATORY DEDICATION Thursday, September 4, 2008 Micro and Nanotechnology Laboratory Dedication September 4, 2008 Dedication of the Micro and Nanotechnology Laboratory Celebrating completion of an $18 million,state-funded expansion of one of the nation’s premier research laboratories for Micro and Nanoelectronics, Nanophotonics and Optoelectronics, Nanomedicine and BioNanotechnology, and MEMS/NEMS and Integrated Systems research. Dedication of the “Light Array Rhythm Catcher” by S.Thomas Scarff Celebrating art inspired by LED technology advanced at the University of Illinois. Remarks & Ribbon Cutting Ilesanmi Adesida Dean, College of Engineering Board of Trustees State of Illinois B. Joseph White President, University of Illinois Capital Development Board Richard Herman Chancellor, University of Illinois at Urbana-Champaign Rashid Bashir Director, Micro and Nanotechnology Laboratory Balloon Launch Students from Campus Middle School for Girls Special Guests Arden Bement Jr. Director, National Science Foundation and Keynote Speaker for the CNST Nanotechnology Workshop Robert Leheny Deputy Director, Defense Advanced Research Projects Agency and Co-keynote Speaker at the CNST Nanotechnology Workshop Tours Guided tours of the building will begin in the atrium and include some of the cleanrooms, nanoelectronics and photonics, and bionanotechnology laboratories. Video Historical highlights are presented on the plasma screen in the atrium. Luncheon Preregistration required. Please check registration materials for directions. Note: This year the University of Illinois Center for Nanoscale Science and Technology (CNST) Annual Nanotechnology Workshop is being held in conjunction with the Micro and Nanotechnology Laboratory Dedication. -

Seminar Flyer Rashid Bashir
PRESENTS BioMEMS and Biomedical Nanotechnology: From Lab on Chip to Printing Cellular Machines THURSDAY, May 30th 2019 12:00 – 1:00 PM 2101 ENGINEERING V Rashid Bashir, Ph.D. UIUC Dean, Department of Bioengineering ABSTRACT: Integration of biology, medicine, and fabrication methods at the micro and nano scale offers tremendous opportunities for solving important problems in biology and medicine and to enable a wide range of applications in diagnostics, therapeutics, and tissue engineering. Microfluidics and Lab-on-Chip can be very beneficial to realize practical applications in detection of disease markers, counting of specific cells from whole blood, and for identification of pathogens, at point-of-care. In this talk, we will present data driven approaches for stratification of sepsis, detection of cells and proteins from a drop of blood, rapid detection of pathogens from body fluids, and spatial mapping of nucleic acids from cancer tumors. We will also present our work on bio- printing with stereolithography to produce bio-hybrid devices made of polymers and cells for the development of biological machines, soft robotics, and hyper organs. Such complex cellular systems will be a major challenge for the next decade and beyond, requiring knowledge from tissue engineering, synthetic biology, micro-fabrication and nanotechnology, systems biology, and developmental biology. These devices could have potential applications in drug delivery, power generation, and other biomimetic systems. BIOGRAPHY: Rashid Bashir is Dean of Engineering, the Grainger Distinguished Chair in Engineering and Professor of Bioengineering at the University of Illinois at Urbana-Champaign. Previously, he was the Executive Associate Dean at the Carle-Illinois College of Medicine (2017 – present), the Abel Bliss Professor of Engineering, Head of Department of Bioengineering (2013 – 2017), and Director of the Micro and Nanotechnology Laboratory (a campus-wide clean room research facility) (2007 – 2013). -

Report by the Anti-Racism Task Force to Dean Rashid Bashir, Grainger College of Engineering
Report by the Anti-Racism Task Force to Dean Rashid Bashir, Grainger College of Engineering The Anti-Racism Task Force (ARTF) of the IDEA Institute August 14, 2020 1 Authors • Nancy Amato, Professor and Head, Department of Computer Science • Aron Barbey, Professor, Department of Psychology • Beleicia Benita Bullock, Graduate student, Department of Computer Science • Victor Cervantes, Staff, Morrill Engineering Program • Jamie Clark, Graduate student, Department of Civil and Environmental Engineering • Ollie Watts Davis, Professor, School of Music • Sharlene Denos, Staff, Department of Physics • Shen Dillon, Professor, Department of Material Sciences and Engineering • Aishani Dutta, Undergraduate student, Department of Computer Science • Lonna Edwards, Graduate student, Department of Electrical and Computer Engineering • Kelly Foster, Staff, Illinois Quantum Information Science and Technology Center (IQUIST) • Jaden Gladden, Undergraduate student, Technical Systems Management (ACES) • Holly Golecki, Teaching Assistant Professor, Department of Bioengineering • Ying Qi Guan, Undergraduate student, Department of Mechanical engineering • Indranil (Indy) Gupta, Professor, Department of Computer Science • Ramez Hajj, Assistant Professor, Department of Civil and Environmental Engineering • Jancie Harris, Staff, Department of Computer Science • Ilalee Harrison James, Staff and MBA student, Gies College of Business and Grainger College of Engineering • Kathleen Isnegger, Graduate student, Department of Computer Science • Katrina Jones, Staff, Department -

Features Contents
FEATURES COMPUTING A HEALTHIER MOLECULAR A publication of the 8 FUTURE 18 JIGSAW PUZZLE J. Crayton Pruitt Family Department of Biomedical Engineering at the University of Florida DEAN, COLLEGE OF ENGINEERING CONTENTS Cammy Abernathy DEPARTMENT CHAIR Christine E. Schmidt 2 WELCOME FROM THE CHAIR 14 HAVING AN IMPACT ON Dr. Christine Schmidt PATIENT CARE EDITOR Dr. Aysegul Gunduz, Dr. Huabei Jiang Sommer Green 4 BME FACULTY SNAPSHOT 16 STUDENT ENDEAVORS EDITORIAL CONTRIBUTORS 6 PRUITT HISTORICAL Rebecca Burton Laura Mize MARKER EVENT 20 GRADUATE STUDENT FEATURE Evelyn Bracho-Sanchez Michael Stone NEWS & NOTABLES 7 CONTRIBUTING 21 ALUMNI FEATURE PHOTOGRAPHERS Dr. Justin Sanchez 7 DISTINGUISHED LEADERSHIP Bernard Brzezinski SEMINAR SERIES Thinkstock.com 22 BME GIFTS BioD and the Leo Claire & Robert COVER ILLUSTRATION 12 UF PREEMINENCE & NEW FACULTY Adenbaum Foundation & DESIGN University Relations Dr. Kevin Otto, Dr. Cherie Stabler, Creative Services Dr. Lin Yang UF BME Faculty Snapshot AYSEGUL GUNDUZ BRANDI K. ORMEROD Assistant Professor Associate Professor Ph.D., University of Florida Ph.D., University of British Columbia Human neuroscience, neuroprostheses Engineered stem cell and immunomodulatory and neurorehabilitation. strategies for brain repair and aging studies. KYLE D. ALLEN RANGANATHA SITARAM Assistant Professor Assistant Professor Ph.D., Rice University Ph.D., University of Tuebingen Novel strategies to diagnose and treat Neuroscience and neuroimaging, degenerative joint diseases. brain-computer interfaces and neurofeedback, and connectomics. DAVID E. HINTENLANG KEVIN J. OTTO Associate Professor Associate Professor Ph.D., Brown University Ph.D., Arizona State University Real-time characterization and optimization of Neural engineering, device-tissue interfaces radiation dosimetry for therapy and imaging. and neurostimulation. WESLEY E. -

Nanotechnology Workshop
Center for Nanoscale Science and Technology Multidisciplinary Research: Collaboratory The University of Illinois Center for Nanoscale Science and Technology (CNST) is the premier center for nanotechnology research, education, and outreach Center for Nanoscale Science and Technology Institute for Genomic Biology 2000 Micro and Nanotechnology Laboratory Institute for Genomic Biology activities. CNST draws its strength from working as a collaboratory involving the 208 N.Wright Street 1206 W. Gregory Drive Beckman Institute for Advanced Science and Technology, Biotechnology Center, Urbana, IL 61801 Urbana, IL 61801 Coordinated Science Laboratory, Frederick Seitz Materials Research Laboratory, Ilesanmi Adesida, Director Harris Lewin, Director Institute for Genomic Biology, Micro and Nanotechnology Laboratory, Center for Irfan Ahmad, Associate Director (217) 244-2999 Nanoscale Chemical, Electrical, Mechanical, Manufacturing Systems, National (217) 333-3097 www.igb.uiuc.edu www.cnst.illinois.edu Center for Supercomputing Applications, and the School of Chemical Sciences. The Center is working towards seamless integration of interdisciplinary research Micro and Nanotechnology Laboratory from atoms and materials to devices and systems. CNST is uniquely located to Advanced Materials for Purification 2000 Micro and Nanotechnology Laboratory of Water with Systems 208 N.Wright Street harness the entrepreneurial and technical spirit in the Midwest, with ongoing (Water CAMPWS) Center Urbana, IL 61801 industrial linkages as it prepares tomorrow’s workforce. The CNST thrives on its 2127 Mechanical Engineering Laboratory 1206 West Green St. Rashid Bashir, Director cutting-edge research in bionanotechnology, computational nanotechnology, Urbana, IL 61801 (217) 333-3097 nanocharacterization, nanoelectromechanical systems, nanoelectronics, www.mntl.illinois.edu nanofabrication, nanomaterials, nanomanufacturing, nanomedicine, and Mark A. Shannon, Director (217) 333-2633 nanophotonics. -

Capture of Airborne Nanoparticles in Swirling Flows Using Non-Uniform
Purdue University Purdue e-Pubs Other Nanotechnology Publications Birck Nanotechnology Center 6-2-2006 Capture of airborne nanoparticles in swirling flows using non-uniform electrostatic fields for bio- sensor applications Jaesung Jang Laboratory of Integrated Biomedical Micro/Nanotechnology and Applications, Birck Nanotechnology Center, Bindley Biosciences Center, School of Electrical and Computer Engineering, Purdue University Demir Akin Purdue University, [email protected] Kwan Seop Lim Birck Nanotechnology Center, Bindley Bioscience Center, School of Electrical and Computer Engineering, Weldon School of Biomedical Engineering, Purdue University; ERC for Advanced Bioseparation Technology, Inha University, [email protected] Steve Broyles Department of Biochemistry, Purdue University, [email protected] Michael R. Ladisch Weldon School of Biomedical Engineering, Purdue University, [email protected] See next page for additional authors Follow this and additional works at: http://docs.lib.purdue.edu/nanodocs Jang, Jaesung; Akin, Demir; Lim, Kwan Seop; Broyles, Steve; Ladisch, Michael R.; and Bashir, Rashid, "Capture of airborne nanoparticles in swirling flows using non-uniform electrostatic fields for bio-sensor applications" (2006). Other Nanotechnology Publications. Paper 3. http://docs.lib.purdue.edu/nanodocs/3 This document has been made available through Purdue e-Pubs, a service of the Purdue University Libraries. Please contact [email protected] for additional information. Authors Jaesung Jang, Demir Akin, Kwan Seop Lim, Steve Broyles, Michael R. Ladisch, and Rashid Bashir This article is available at Purdue e-Pubs: http://docs.lib.purdue.edu/nanodocs/3 Sensors and Actuators B 121 (2007) 560–566 Capture of airborne nanoparticles in swirling flows using non-uniform electrostatic fields for bio-sensor applications Jaesung Jang a, Demir Akin a, Kwan Seop Lim a,e, Steven Broyles d, Michael R. -
Just a Drop. How Ece Is Helping to Drive Bio Applications Top of Mind Resonance
SENSING THE FUTURE $100M TRANSFORMATIVE INITIATIVE ECE MAKES A GLOBAL IMPACT BUILDING CRITICAL SPACES POWERFUL VIDEO PROCESSING UNDERSTANDING THE SPACE ABOVE 10 ANSWERS RESONANCETHE MAGAZINE OF ECE ILLINOIS FALL 2013 JUST A DROP. HOW ECE IS HELPING TO DRIVE BIO APPLICATIONS TOP OF MIND RESONANCE Fall 2013 EDITORIAL BOARD William H. Sanders Interim Department Head W. Brad Petersen Director of Communications and Editor Later in this magazine you’ll read about the $100 million commitment the Jeanette Beck College of Engineering at Illinois received early this year to launch the Assistant to the Department Head Grainger Engineering Breakthroughs Initiative. The incredible generosity of The Grainger Foundation of Lake Forest, Illinois, will help departments Jennifer Carlson across the college—including ECE—through support of new professorships, Academic Programs Coordinator student scholarships, and investment in our facilities. Breanne Ertmer At a time when support from the State of Illinois is at an all-time low, private Corporate Relations Coordinator support is extremely important to ensure we can continue to fulfill our land- Steve Franke grant mission. Student scholarships are one area of strong need. In 1990, Associate Head for Graduate Affairs the state provided $3.36 in funding per student tuition dollar. As of 2012, that number is down to 62 cents. Jamie Hutchinson Publications Office Editor Early next year the College of Engineering will announce a massive scholar- ship fundraising initiative designed to ensure that great students still have Sarah Heier access to a great education at Illinois. Through this initiative we’ll ensure Alumni and Student Relations Coordinator that students of all backgrounds will have a chance to get an ECE ILLINOIS education.