Stigma and Disclosure: the Health Communication of Gay And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Philip Roth's Confessional Narrators: the Growth of Consciousness
Loyola University Chicago Loyola eCommons Dissertations Theses and Dissertations 1979 Philip Roth's Confessional Narrators: The Growth of Consciousness. Alexander George Loyola University Chicago Follow this and additional works at: https://ecommons.luc.edu/luc_diss Part of the English Language and Literature Commons Recommended Citation George, Alexander, "Philip Roth's Confessional Narrators: The Growth of Consciousness." (1979). Dissertations. 1823. https://ecommons.luc.edu/luc_diss/1823 This Dissertation is brought to you for free and open access by the Theses and Dissertations at Loyola eCommons. It has been accepted for inclusion in Dissertations by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. Copyright © 1979 Alexander George PHILIP ROTH'S CONFESSIONAL NARRATORS: THE GROWTH OF' CONSCIOUSNESS by Alexander George A Dissertation Submitted to the Faculty of the Graduate School of Loyola University of Chicago in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy May 1979 ACKNOWLEDGE~£NTS It is a singular pleasure to acknowledge the many debts of gratitude incurred in the writing of this dissertation. My warmest thanks go to my Director, Dr. Thomas Gorman, not only for his wise counsel and practical guidance, but espec~ally for his steadfast encouragement. I am also deeply indebted to Dr. Paul Messbarger for his careful reading and helpful criticism of each chapter as it was written. Thanks also must go to Father Gene Phillips, S.J., for the benefit of his time and consideration. I am also deeply grateful for the all-important moral support given me by my family and friends, especially Dr. -

Pirate and Hacking Speak Because Your Communicating with the World, Tell Them What You Think
Pirate and Hacking Speak Because your communicating with the world, tell them what you think.... ----------------------------------------------------------------------- Afrikaans Poes / Doos - Pussy Fok jou - Fuck you Jy pis my af - You're pissing me off Hoer - Whore Slet - Slut Kak - Shit Poephol - Asshole Dom Doos - Dump Pussy Gaan fok jouself - Go fuck yourself ------------------------------------------------------------------------ Arabic Koos - cunt. nikomak - fuck your mother sharmuta - whore zarba - shit kis - vagina zib - penis Elif air ab tizak! - a thousand "dicks" in your ass! kisich - pussy Elif air ab dinich - A thousand dicks in your religion Mos zibby! - Suck my dick! Waj ab zibik! - An infection to your dick! kelbeh - bitch (lit a female dog) Muti - jackass Kanith - Fucker Kwanii - Faggot Bouse Tizi - Kiss my ass Armenian Aboosh - Stupid Dmbo, Khmbo - Idiot Myruht kooneh - Fuck your mother Peranuht shoonuh kukneh - The dog should shit in your mouth Esh - Donkey Buhlo (BUL-lo) - Dick Kuk oudelic shoon - Shit eating dog Juge / jugik - penis Vorig / vor - ass Eem juges bacheek doer - Kiss my penis Eem voriga bacheek doer - Kiss my ass Toon vor es - You are an ass Toon esh es - You are a jackass Metz Dzi-zik - Big Breasts Metz Jugik - Big penis ------------------------------------------------------------------------ Bengali baing chood - sister fucker chood - fuck/fucker choodmarani - mother fucker haramjada - bastard dhon - dick gud - pussy khanki/maggi - whore laewra aga - dickhead tor bapre choodi - fuck your dad ------------------------------------------------------------------------ -

2020-05-25 Prohibited Words List
Clouthub Prohibited Word List Our prohibited words include derogatory racial terms and graphic sexual terms. Rev. 05/25/2020 Words Code 2g1c 1 4r5e 1 1 Not Allowed a2m 1 a54 1 a55 1 acrotomophilia 1 anal 1 analprobe 1 anilingus 1 ass-fucker 1 ass-hat 1 ass-jabber 1 ass-pirate 1 assbag 1 assbandit 1 assbang 1 assbanged 1 assbanger 1 assbangs 1 assbite 1 asscock 1 asscracker 1 assface 1 assfaces 1 assfuck 1 assfucker 1 assfukka 1 assgoblin 1 asshat 1 asshead 1 asshopper 1 assjacker 1 asslick 1 asslicker 1 assmaster 1 assmonkey 1 assmucus 1 assmunch 1 assmuncher 1 assnigger 1 asspirate 1 assshit 1 asssucker 1 asswad 1 asswipe 1 asswipes 1 autoerotic 1 axwound 1 b17ch 1 b1tch 1 babeland 1 1 Clouthub Prohibited Word List Our prohibited words include derogatory racial terms and graphic sexual terms. Rev. 05/25/2020 ballbag 1 ballsack 1 bampot 1 bangbros 1 bawdy 1 bbw 1 bdsm 1 beaner 1 beaners 1 beardedclam 1 bellend 1 beotch 1 bescumber 1 birdlock 1 blowjob 1 blowjobs 1 blumpkin 1 boiolas 1 bollock 1 bollocks 1 bollok 1 bollox 1 boner 1 boners 1 boong 1 booobs 1 boooobs 1 booooobs 1 booooooobs 1 brotherfucker 1 buceta 1 bugger 1 bukkake 1 bulldyke 1 bumblefuck 1 buncombe 1 butt-pirate 1 buttfuck 1 buttfucka 1 buttfucker 1 butthole 1 buttmuch 1 buttmunch 1 buttplug 1 c-0-c-k 1 c-o-c-k 1 c-u-n-t 1 c.0.c.k 1 c.o.c.k. -

Rhetorical Meaning-Making Within Intimate Encounters and Their Discourses at the Macro, Meso, and Micro Levels
University of Wisconsin Milwaukee UWM Digital Commons Theses and Dissertations August 2020 'Would You Say You Had Sex If...' Rhetorical Meaning-Making Within Intimate Encounters and Their Discourses at the Macro, Meso, and Micro Levels Megan Orcholski University of Wisconsin-Milwaukee Follow this and additional works at: https://dc.uwm.edu/etd Part of the Gender and Sexuality Commons, and the Rhetoric Commons Recommended Citation Orcholski, Megan, "'Would You Say You Had Sex If...' Rhetorical Meaning-Making Within Intimate Encounters and Their Discourses at the Macro, Meso, and Micro Levels" (2020). Theses and Dissertations. 2571. https://dc.uwm.edu/etd/2571 This Dissertation is brought to you for free and open access by UWM Digital Commons. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of UWM Digital Commons. For more information, please contact [email protected]. ‘WOULD YOU SAY YOU HAD SEX IF…’ RHETORICAL MEANING-MAKING WITHIN INTIMATE ENCOUNTERS AND THEIR DISCOURSES AT THE MACRO, MESO, AND MICRO LEVELS. by Megan Orcholski A Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Communication at The University of Wisconsin-Milwaukee December 2020 ABSTRACT ‘WOULD YOU SAY YOU HAD SEX IF…’ RETORICAL MEANING-MAKING WITHIN INTIMATE ENCOUNTERS AND THEIR DISCOURSES AT THE MACRO, MESO, AND MICRO LEVELS. by Megan Orcholski The University of Wisconsin-Milwaukee, 2020 Under the Supervision of Professor Dr. Leslie Harris, Ph.D. This dissertation advances a deeper understanding of the rhetoric of intimate encounters by analyzing meaning-making practices at the intersections of sex, sexuality, and sexualized violence at the macro, meso, and micro levels. -
Dissertation for the Degree of Master of Arts In
DISSERTATION FOR THE DEGREE OF MASTER OF ARTS IN LINGUISTICS (BY RESEARCH) STEPHEN TURTON (454123) TITLE Trufax about Discussion Group Netspeak: An Historical Analysis of Semantic Change in the English Slang of Newsgroups and Web Forums SUPERVISOR Dr Andrew Van der Spuy Stephen Turton (454123) LING7010 Page i DECLARATION I, Stephen Turton, state that to the best of my knowledge and belief this dissertation contains no material previously published by any other person except where due acknowledgement has been made. This thesis contains no material which has been accepted for the award of any other degree or diploma in any university. This is my own unaided work. Signed: Date: 27 October 2014 Stephen Turton (454123) LING7010 Page ii A NOTE OF THANKS I should like to thank the Department of Linguistics at the University of the Witwatersrand for the kindness and generosity they have shown to me over the last five years. In particular I wish to thank my supervisor, Dr Andrew Van der Spuy, for the enthusiasm, encouragement, and insight he offered in guiding my research from an inkling of an idea to the completed dissertation. Stephen Turton (454123) LING7010 Page 1 TABLE OF CONTENTS 1 Introduction p. 4 1.1 A Note on the Title p. 4 1.2 Preliminary Remarks p. 4 1.3 Overview p. 6 1.4 Regarding the Presentation of Data p. 7 2 Background p. 8 2.1 Semantic Change p. 8 2.2 Slang p. 8 2.3 Internet Discussion Groups p. 13 3 Literature Review p. 17 4 Methodology p. 21 5 Theoretical Framework p. -

Medical Language in the Speeches of Demosthenes Allison Das a Dissertation Submitted in Partial Fulfillment of the Requirement
Medical Language in the Speeches of Demosthenes Allison Das A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2015 Reading Committee: Ruby Blondell, Chair Deborah Kamen Alexander Hollmann Program Authorized to Offer Degree: Classics Department Allison Das ii ©Copyright 2015 Allison E. Das Allison Das iii University of Washington Abstract Medical Language in the Speeches of Demosthenes Allison E. Das Chair of Supervisory Committee Dr. Ruby Blondell Classics Department Introduction This project is intended as an examination of medical language and imagery in the speeches of Demosthenes, with special attention given to his speeches against his political opponent Aeschines, Against the False Embassy (19) and On the Crown (18). In Chapter 1, I contextualize his use of such language and imagery by exploring the influence of Hippocratic medicine on fourth- and fifth-century non-medical literature. I argue that the shared anxieties of medicine and politics, namely that both arts demand quick action and foresight on the part of the good practitioner, and the rich new vocabulary of suffering and disease, made Hippocratic medicine an enticing model for the political writer, that is, the historian, philosopher, and orator. Demosthenes' medical language and imagery should thus be seen as part of a tradition of analogizing the two arts, which began during the circulation of the first Hippocratic treatises and continued well into and past his own day. Allison Das iv In Chapter 2, I look at medical language and imagery in Demosthenes' prosecution of Aeschines for political misconduct during the Second Embassy to Philip II of Macedon, On the False Embassy. -

29.Philosophy of Liberation.Pdf
CONTENTS Preface viii Chapter 1 HISTORY 1.1 Geopolitics and Philosophy 1 1.2 Philosophy of Liberation ofthe Periphery 9 Chapter 2 FROM PHENOMENOLOGY TO LIBERATION 2.1 Proximity 16 2.2 Tota1ity 21 2.3 Mediation 29 2.4 Exteriority 39 2.5 Alienation 49 2.6 Liberation 58 Chapter 3 FROM POLITICS TO ANTIFETISHISM 3.1 Politics 67 3.2 Erotics 78 3.3 Pedagogics 87 3.4 Antifetishism 95 Chapter 4 FROM NATURE TO ECONOMICS 4.1 Nature 106 4.2 Semiotics 117 4.3 Poietics 126 4.4 Economics 140 vi Chapter 5 FROM SCIENCE TO PHILOSOPHY OF LIBERATION 5.1 Science 153 5.2 Dialectic 156 5.3 The Analectical Moment 158 5.4 Practice 160 5.5 Poietics 163 5.6 Human Sciences 165 5.7 Ideological Methods 167 5.8 Critical Methods 169 5.9 Philosophy of Liberation 170 Appendix PHILOSOPHY AND PRAXIS A. Philosophy and Ideology 181 B. Dialectic between Philosophy and Praxis 183 C. Exigencies for a Philosophy of Liberation 188 D. Toward an International Division of Philosophical Labor 195 Notes 197 Glossary of Concepts 201 Glossary of Non-English Terms 213 vii PREFACE What follows is addressed to neophytes in philosophy of libera- tion. It does not claim to be an exhaustive exposition. It is a discourse that proceeds by elaborating one thesis after another, using its own categories and its own method. It is a provisional theoretical philosophical framework. Except in the Appendix, this work has few footnotes and no bibliography. Writing in the sorrow of exile (in Mexico), I did not have access to my personal library (in Argentina). -

Crypto Anarchy, Cyberstates, and Pirate Utopias Edited by Peter Ludlow
Ludlow cover 7/7/01 2:08 PM Page 1 Crypto Anarchy, Cyberstates, and Pirate Utopias Crypto Anarchy, Crypto Anarchy, Cyberstates, and Pirate Utopias edited by Peter Ludlow In Crypto Anarchy, Cyberstates, and Pirate Utopias, Peter Ludlow extends the approach he used so successfully in High Noon on the Electronic Frontier, offering a collection of writings that reflect the eclectic nature of the online world, as well as its tremendous energy and creativity. This time the subject is the emergence of governance structures within online communities and the visions of political sovereignty shaping some of those communities. Ludlow views virtual communities as laboratories for conducting experiments in the Peter Ludlow construction of new societies and governance structures. While many online experiments will fail, Ludlow argues that given the synergy of the online world, new and superior governance structures may emerge. Indeed, utopian visions are not out of place, provided that we understand the new utopias to edited by be fleeting localized “islands in the Net” and not permanent institutions. The book is organized in five sections. The first section considers the sovereignty of the Internet. The second section asks how widespread access to resources such as Pretty Good Privacy and anonymous remailers allows the possibility of “Crypto Anarchy”—essentially carving out space for activities that lie outside the purview of nation-states and other traditional powers. The Crypto Anarchy, Cyberstates, third section shows how the growth of e-commerce is raising questions of legal jurisdiction and taxation for which the geographic boundaries of nation- states are obsolete. The fourth section looks at specific experimental governance and Pirate Utopias structures evolved by online communities. -

Seafood Appetizers Appetizers Salads Sandwiches Pirate Burgers Entrees Side Dishes
Seafood Appetizers Appetizers Bucket O’ Fries Maryland Cream of Crab Soup xx xx Crispy Hand-Cut Seasoned Fries, Mutiny Sauce 6 Backfin Crabmeat, Old Bay, Sherry 6 Crispy Cannon Balls Raw Oysters on the Half Shell xx Fried Mac n’ Cheese, Smoked Chipotle Mayo 9 Ask Your Server for Today’s Selections Salads Market Price Jumbo Wings! Shiver Me Tender Salad Crock O’ Crab Dip Served with Celery & Choice of Chipotle Ranch or Blue Cheese xx Hand Breaded Chicken Breast, Housemade Old Bay Chips 11 ** Grilled with Jamaican Jerk Sauce Baby Mixed Greens, Hard Boiled ** Traditional Buffalo Hot Sauce Egg, Tomato, Beer Battered Beer Steamed Mussels ** Old Bay Rub Onion Rings, Chipotle Ranch Andouille Sausage, Spicy Tomato Beer Broth, House Beer ** Grilled with House Rib Rub xx Bread –or- Natty Boh, Chipotle Butter, Cilantro Sour Cream ** Barbecued – Guava, Spiced Rum or Kentucky Bourbon Sauce Dressing 15 xx xx 9 11 Grilled Salmon Salad Baby Spinach, Red Onion, Kraken Tentacles Moby Pickle xx xx Tomato, Hard Boiled Egg, Flash Fried Calamari, Spicy Tomato Sauce 10 Beer Battered Dill Pickle Spears, Chipotle Ranch Sauce 6 Applewood Smoked Bacon, xx Calypso Fries Pepperoni Flatbread Honey Orange Vinaigrette 16 xx Crab Dip, Hand-Cut Fries, Cheddar Jack Cheese Spicy Garlic Tomato Sauce, Grilled Red Onion, 11 Grilled Sesame Chicken Mozzarella Cheese 9xx Salad Romaine Lettuce, Green Bell Scurvy Nachos Pepper, Red Onion, Toasted House Fried Tortilla Chips, Grilled Marinated Chicken Breast, Sesame Seeds, Dried Cranberries, Black Beans, Pico de Gallo, Sour Cream, -

Download File
A Monster for Our Times: Reading Sade across the Centuries Matthew Bridge Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2011 © 2011 Matthew Bridge All Rights Reserved ABSTRACT A Monster for Our Times: Reading Sade across the Centuries Matthew Bridge This doctoral dissertation looks at several readings and interpretations of the works of the Marquis de Sade, from the eighteenth century to the present. Ever since he was imprisoned under the Old Regime following highly publicized instances of physical and sexual abuse, Sade has remained a controversial figure who has been both condemned as a dangerous criminal and celebrated as an icon for artistic freedom. The most enduring aspect of his legacy has been a vast collection of obscene publications, characterized by detailed descriptions of sexual torture and murder, along with philosophical diatribes that offer theoretical justifications for the atrocities. Not surprisingly, Sade’s works have been subject to censorship almost from the beginning, leading to the author’s imprisonment under Napoleon and to the eventual trials of his mid-twentieth-century publishers in France and Japan. The following pages examine the reception of Sade’s works in relation to the legal concept of obscenity, which provides a consistent framework for textual interpretation from the 1790s to the present. I begin with a prelude discussing the 1956 trial of Jean-Jacques Pauvert, in order to situate the remainder of the dissertation within the context of how readers approached a body of work as quintessentially obscene as that of Sade. -
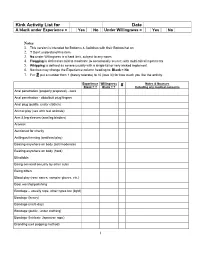
Kink Activity List for Date
Kink Activity List for Date A blank under Experience = Yes No Under Willingness = Yes No Notes 1. This version is intended for Bottoms & Switches with their Bottom hat on 2. ? Don't understand this item. 3. No under Willingness is a hard limit, subject to any notes 4. Flogging is defined as mild to moderate (& occasionally severe) with multi-tailed implements 5. Whipping is defined as severe usually with a single-tail or very wicked implement 6. Novices may change the Experience column heading to: Blank = No 7. For # put a number from 1 (barely tolerate) to 10 (love it!) for how much you like the activity. Experience Willingness # Notes & Nuances Blank = ? Blank = ? Including any medical concerns Anal penetration (properly prepared) - cock Anal penetration - dildo/butt plug/fingers Anal plug (public, under clothes) Animal play (sex with real animals) Arm & leg sleeves (arm/leg binders) Aromas Auctioned for charity Anilingus/rimming (oral/anal play) Beating anywhere on body (soft/moderate) Beating anywhere on body (hard) Blindfolds Being serviced sexually by other subs Being bitten Blood play (rose canes, vampire gloves, etc.) Boot worship/polishing Bondage – usually rope, other types too (light) Bondage (heavy) Bondage (multi-day) Bondage (public, under clothing) Bondage (Intricate Japanese rope) Branding (cell popping method) 1 Kink Activity List for Date A blank under Experience = Yes No Under Willingness = Yes No Experience Willingness # Notes & Nuances Blank = ? Blank = ? Including any medical concerns Branding (violet wand) Branding -

Sing Solo Pirate: Songs in the Key of Arrr! a Literature Guide for the Singer and Vocal Pedagogue
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Student Research, Creative Activity, and Performance - School of Music Music, School of 5-2013 Sing Solo Pirate: Songs in the Key of Arrr! A Literature Guide for the Singer and Vocal Pedagogue Michael S. Tully University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/musicstudent Part of the Music Pedagogy Commons, Music Performance Commons, and the Music Practice Commons Tully, Michael S., "Sing Solo Pirate: Songs in the Key of Arrr! A Literature Guide for the Singer and Vocal Pedagogue" (2013). Student Research, Creative Activity, and Performance - School of Music. 62. https://digitalcommons.unl.edu/musicstudent/62 This Article is brought to you for free and open access by the Music, School of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Student Research, Creative Activity, and Performance - School of Music by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. SING SOLO PIRATE: SONGS IN THE KEY OF ARRR! A LITERATURE GUIDE FOR THE SINGER AND VOCAL PEDAGOGUE by Michael S. Tully A DOCTORAL DOCUMENT Presented to the Faculty of The Graduate College at the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Doctor of Musical Arts Major: Music Under the Supervision of Professor William Shomos Lincoln, Nebraska May, 2013 SING SOLO PIRATE: SONGS IN THE KEY OF ARRR! A LITERATURE GUIDE FOR THE SINGER AND VOCAL PEDAGOGUE Michael S. Tully, D.M.A. University of Nebraska, 2013 Advisor: William Shomos Pirates have always been mysterious figures.