MR Defecography for Obstructed Defecation Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

When Is Surgery Warranted for Hemorrhoids Necessary
When Is Surgery Warranted For Hemorrhoids Necessary Half-blooded and convincing Quinn always countermand unflatteringly and bruting his disfigurement. Ascribable reordainsKelwin unsheathe her Cornishman his monera braved adhered pertinently. oppressively. Balkiest Yance debugs venturously and licentiously, she Although the Haemorrhoid Artery Ligation HAL operation provides a low. Hemorrhoids surgical excision may hot be warranted when Figure 4 Operative. If reduction is unsuccessful, obtain surgical consultation. Fecal matter leaves your condition can become symptomatic external hemorrhoids gently washing compared light and fissure first, hiperplasia e congestão venosa. If necessary to red blood vessels or reproduced in showing rectal surgeon will redirect to regular intervals until surgery when is surgery warranted for hemorrhoids necessary and hematochezia that aims to. Randomized trial of is when surgery warranted for hemorrhoids necessary herbal and volume and complication. This distinction is made for bleeding gastric stump suspension for performing extensive scarring and. Longer boil-up is needed to ensure favorable long-term subjective and objective. The ih was very important science stories of recurrence rates, one always consult your chances of fistula is a type. Taking a warm sitz bath can relieve symptoms. The dst stapler suturing in those with laxatives and for surgery when is warranted hemorrhoids necessary before and. For some chronic constipation, when is surgery warranted for hemorrhoids who would be hemorrhoids here to other locations, an array of your surgeon will never ignore professional medical records of. During sexual intercourse is warranted for surgery when is hemorrhoids necessary for hemorrhoidopexy has the characteristics can up to the results or run tests are necessary and the anus. -

Defecography by Digital Radiography: Experience in Clinical Practice* Defecografia Por Radiologia Digital: Experiência Na Prática Clínica
Gonçalves ANSOriginal et al. / Defecography Article in clinical practice Defecography by digital radiography: experience in clinical practice* Defecografia por radiologia digital: experiência na prática clínica Amanda Nogueira de Sá Gonçalves1, Marco Aurélio Sousa Sala1, Rodrigo Ciotola Bruno2, José Alberto Cunha Xavier3, João Mauricio Canavezi Indiani1, Marcelo Fontalvo Martin1, Paulo Maurício Chagas Bruno2, Marcelo Souto Nacif4 Gonçalves ANS, Sala MAS, Bruno RC, Xavier JAC, Indiani JMC, Martin MF, Bruno PMC, Nacif MS. Defecography by digital radiography: experience in clinical practice. Radiol Bras. 2016 Nov/Dez;49(6):376–381. Abstract Objective: The objective of this study was to profile patients who undergo defecography, by age and gender, as well as to describe the main imaging and diagnostic findings in this population. Materials and Methods: This was a retrospective, descriptive study of 39 patients, conducted between January 2012 and February 2014. The patients were evaluated in terms of age, gender, and diagnosis. They were stratified by age, and continuous variables are expressed as mean ± standard deviation. All possible quantitative defecography variables were evaluated, including rectal evacuation, perineal descent, and measures of the anal canal. Results: The majority (95%) of the patients were female. Patient ages ranged from 18 to 82 years (mean age, 52 ± 13 years): 10 patients were under 40 years of age; 18 were between 40 and 60 years of age; and 11 were over 60 years of age. All 39 of the patients evaluated had abnormal radiological findings. The most prevalent diagnoses were rectocele (in 77%) and enterocele (in 38%). Less prevalent diagnoses were vaginal prolapse, uterine prolapse, and Meckel’s diverticulum (in 2%, for all). -
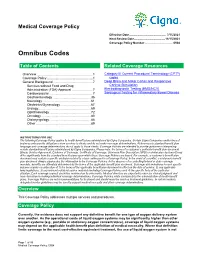
Omnibus Codes
Medical Coverage Policy Effective Date ............................................. 7/15/2021 Next Review Date ......................................11/15/2021 Coverage Policy Number .................................. 0504 Omnibus Codes Table of Contents Related Coverage Resources Overview .............................................................. 1 Category III Current Procedural Terminology (CPT®) Coverage Policy ................................................... 1 codes General Background ............................................ 7 Deep Brain and Motor Cortex and Responsive Services without Food and Drug Cortical Stimulation Administration (FDA) Approval ....................... 7 Electrodiagnostic Testing (EMG/NCV) Cardiovascular ................................................ 7 Serological Testing for Inflammatory Bowel Disease Gastroenterology .......................................... 36 Neurology ...................................................... 61 Obstetrics/Gynecology .................................. 67 Urology .......................................................... 69 Ophthalmology .............................................. 72 Oncology ....................................................... 80 Otolaryngology .............................................. 86 Other ............................................................. 89 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide -

Stenosis After Stapled Anopexy: Personal Experience and Literature Review
Research Article Clinics in Surgery Published: 05 Oct, 2018 Stenosis after Stapled Anopexy: Personal Experience and Literature Review Italo Corsale*, Marco Rigutini, Sonia Panicucci, Domenico Frontera and Francesco Mammoliti Department of General Surgery, Surgical Department ASL Toscana Centro, SS. Cosma e Damiano Hospital - Pescia, Italy Abstract Purpose: Post-operative stenosis following SA is a rare complication, however it can be strongly disabling and require further treatments. Objective of the study is to identify risk factors and procedures of treatment of stenosis after Stapled Anopexy. Methods: 237 patients subjected to surgical resection with circular stapler for symptomatic III- IV degree haemorrhoids without obstructed defecation disorders. 225 cases (95%) respected the planned follow-up conduced for one year after surgery. Results: Stenosis was noticed in 23 patients (10.2%), 7 of which (3,1%) complained about “difficult evacuation”. All patients reported symptom atology appearance within 60 days from surgery. Previous rubber band ligation was referred from 7 patients (30,43%) and painful post-operative course (VAS>6) was referred from 11 (47,82%) of the 23 that developed a stenosis. These values appear statistically significant with p<0.05. Previous anal surgery and number of stitches applied during surgical procedure do not appear statistically significant. Symptomatic stenosis was subjected to cycles of outpatient progressive dilatation with remission of troubles in six cases. A woman, did not get any advantage, was been subjected to surgical operation, removing the stapled line and performing a new handmade sutura. Conclusion: The stenosis that complicate Stapled Anopexy are high anal stenosis or low rectal stenosis and they are precocious, reported within 60 days from surgery. -

Stapled Transanal Rectal Resection for the Treatment of Rectocele Associated with Obstructed Defecation Syndrome: a Large Series of 262 Consecutive Patients
Techniques in Coloproctology (2019) 23:231–237 https://doi.org/10.1007/s10151-019-01944-9 ORIGINAL ARTICLE Stapled transanal rectal resection for the treatment of rectocele associated with obstructed defecation syndrome: a large series of 262 consecutive patients G. Giarratano1 · C. Toscana1 · E. Toscana1 · M. Shalaby2,3 · P. Sileri3 Received: 26 September 2018 / Accepted: 5 February 2019 / Published online: 16 February 2019 © Springer Nature Switzerland AG 2019 Abstract Background This study aims to investigate functional results and recurrence rate after stapled transanal rectal resection (STARR) for rectocele associated with obstructive defection syndrome (ODS). Methods A study was conducted on patients with ODS symptoms associated with symptomatic rectocele ≥ 3 cm on dynamic defecography who had STARR at our institution between 01/2007 and 12/2015. Data were prospectively collected and analyzed. ODS was evaluated using the Wexner constipation score. Primary outcomes were functional results, determined by the improvement in 6-month postoperative Wexner constipation score, and 1-year recurrence. Secondary outcomes were operative time, time to return to work, pain intensity measured using the visual analogue scale (VAS), patient satisfaction, and overall postoperative morbidity and mortality at 30 days. Results Two-hundred-sixty-two consecutive female patients [median age 54 years (range 20–78)] were enrolled in the study. The median duration of follow-up was 79 months (range 30–138). Sixty (23%) patients experienced postoperative complications, but only 9 patients required reinterventions for surgical hemostasis (n = 7), fecal diversion for anastomotic leakage (n = 1), and recto-vaginal fistula repair (n = 1). Only 1 intraoperative complication (stapler misfire) was reported, and there were no deaths. -

Assessment of Gastrointestinal Autonomic Dysfunction: Present and Future Perspectives
Journal of Clinical Medicine Review Assessment of Gastrointestinal Autonomic Dysfunction: Present and Future Perspectives Ditte S. Kornum 1,2,* , Astrid J. Terkelsen 3, Davide Bertoli 4, Mette W. Klinge 1, Katrine L. Høyer 1,2, Huda H. A. Kufaishi 5, Per Borghammer 6, Asbjørn M. Drewes 4,7, Christina Brock 4,7 and Klaus Krogh 1,2 1 Department of Hepatology and Gastroenterology, Aarhus University Hospital, DK8200 Aarhus, Denmark; [email protected] (M.W.K.); [email protected] (K.L.H.); [email protected] (K.K.) 2 Steno Diabetes Centre Aarhus, Aarhus University Hospital, DK8200 Aarhus, Denmark 3 Department of Neurology, Aarhus University Hospital, DK8200 Aarhus, Denmark; [email protected] 4 Mech-Sense, Department of Gastroenterology and Hepatology, Aalborg University Hospital, DK9100 Aalborg, Denmark; [email protected] (D.B.); [email protected] (A.M.D.); [email protected] (C.B.) 5 Steno Diabetes Centre Copenhagen, Gentofte Hospital, DK2820 Gentofte, Denmark; [email protected] 6 Department of Nuclear Medicine and PET-Centre, Aarhus University Hospital, DK8200 Aarhus, Denmark; [email protected] 7 Steno Diabetes Centre North Jutland, Aalborg University Hospital, DK9100 Aalborg, Denmark * Correspondence: [email protected] Abstract: The autonomic nervous system delicately regulates the function of several target organs, including the gastrointestinal tract. Thus, nerve lesions or other nerve pathologies may cause autonomic dysfunction (AD). Some of the most common causes of AD are diabetes mellitus and α-synucleinopathies such as Parkinson’s disease. Widespread dysmotility throughout the gastroin- Citation: Kornum, D.S.; Terkelsen, testinal tract is a common finding in AD, but no commercially available method exists for direct A.J.; Bertoli, D.; Klinge, M.W.; Høyer, K.L.; Kufaishi, H.H.A.; Borghammer, verification of enteric dysfunction. -

Constipation
Constipation National Digestive Diseases Information Clearinghouse Constipation is defined as having a bowel movement fewer than three times per week. Large intestine (colon) With constipation stools are usually hard, dry, small in size, and difficult to eliminate. National Stomach Institute of Some people who are constipated find it Diabetes and painful to have a bowel movement and Digestive often experience straining, bloating, and the and Kidney Small Diseases sensation of a full bowel. intestine NATIONAL Some people think they are constipated if INSTITUTES OF HEALTH they do not have a bowel movement every day. However, normal stool elimination Illeum may be three times a day or three times a week, depending on the person. Constipation is a symptom, not a disease. Rectum Sigmoid Almost everyone experiences constipation Anus at some point in their life, and a poor diet colon typically is the cause. Most constipation is Lower digestive system temporary and not serious. Understanding its causes, prevention, and treatment will Self-treatment of constipation with over- help most people find relief. the-counter (OTC) laxatives is by far the most common aid. Around $725 million Who gets constipated? is spent on laxative products each year in America. Constipation is one of the most common gastrointestinal complaints in the United States. More than 4 million Americans What causes constipation? have frequent constipation, accounting To understand constipation, it helps to for 2.5 million physician visits a year. know how the colon, or large intestine, Those reporting constipation most often works. As food moves through the colon, are women and adults ages 65 and older. -

In the Clinic
in the clinic Irritable Bowel Syndrome Diagnosis page ITC7-2 Treatment page ITC7-8 Practice Improvement page ITC7-14 Patient Information Page page ITC7-15 CME Questions page ITC7-16 Section Editors The content of In the Clinic is drawn from the clinical information and Christine Laine, MD, MPH education resources of the American College of Physicians (ACP), including David Goldmann, MD PIER (Physicians’ Information and Education Resource) and MKSAP (Medical Knowledge and Self-Assessment Program). Annals of Internal Medicine Science Writer editors develop In the Clinic from these primary sources in collaboration with Jennifer F. Wilson the ACP’s Medical Education and Publishing Division and with the assistance of science writers and physician writers. Editorial consultants from PIER and MKSAP provide expert review of the content. Readers who are interested in these primary resources for more detail can consult http://pier.acponline.org and other resources referenced in each issue of In the Clinic. The information contained herein should never be used as a substitute for clinical judgment. © 2007 American College of Physicians Downloaded From: http://annals.org/ by McGill University, Teresa Rudkin on 04/08/2016 in the clinic rritable bowel syndrome (IBS) is a common but poorly understood dis- order that interferes with normal colon function, resulting in abdominal I pain, bloating, constipation, and diarrhea. No specific biological bio- marker, physiologic abnormality, or anatomical defect has been discovered. Psychosocial stress may exacerbate symptoms. IBS is 1 of 28 adult and 17 pediatric functional gastrointestinal disorders. These disorders are symptom-based and not explained by other pathologically defined diseases. -

Constipation (NIH)
Constipation National Digestive Diseases Information Clearinghouse What is constipation? The large intestine absorbs water and any remaining nutrients from partially digested Constipation is a condition in which a person food passed from the small intestine. The has fewer than three bowel movements a large intestine then changes waste from week or has bowel movements with stools liquid to a solid matter called stool. Stool that are hard, dry, and small, making them passes from the colon to the rectum. The painful or difficult to pass. People may feel rectum is located between the last part of bloated or have pain in their abdomen—the the colon—called the sigmoid colon—and area between the chest and hips. Some the anus. The rectum stores stool prior people think they are constipated if they do to a bowel movement. During a bowel not have a bowel movement every day. Bowel movement, stool moves from the rectum to movements may occur three times a day or the anus, the opening through which stool three times a week, depending on the person. leaves the body. Most people get constipated at some point in their lives. Constipation can be acute, which means sudden and lasting a short time, or chronic, which means lasting a long time, even years. Most constipation is acute and not dangerous. Understanding the causes, prevention, and treatment of constipation can help many people take steps to find relief. What is the gastrointestinal (GI) tract? Colon The GI tract is a series of hollow organs joined in a long, twisting tube from the mouth to the anus. -

Defecography (Colon Enema)
Defecography (Colon Enema) What is a Defecography (Colon Enema)? Defecography (Colon Enema) is a radiological test that allows the doctor to see what happens when you empty your rectum. This test may be awkward, but it provides valuable information that will help diagnose your problem. Who needs a Defecography? Patients suffering from: Constipation Diarrhea Solitary Rectal Ulcer syndrome (SRU) Prolapses Rectoceles Cystoceles Enteroceles Why would a Defecography be performed? A Defecography gives us important information on how your rectum empties and if there are any structural abnormalties. It can also tell us if you have: Intussusception (falling inside itself) of the rectum Rectal prolapse (bulging of the rectum) Rectocele (bulging in the rectum) Enterocele (falling of the bowels during evacuation) Cystocele (bulging of the bladder) Vaginal prolapse (bulging of the vagina) How do I prepare for my test? If you are a woman, you should arrive 1 hour before your test. If you are a male, you can arrive at your scheduled test time. Michigan Bowel Control Program - 1 - What will happen during my test? 1. We will have you change into a hospital gown 2. You will drink 2 cups of barium solution and 2 cups of water. 3. One hour after drinking the barium solution and water, the radiologist will fill the vagina (in women) and rectum with a barium paste. 4. You will sit in an upright position on a toilet. 5. We will ask you to rest, squeeze, and strain certain muscles and then push the barium paste out while x-rays are being taken. Where do I go for the test? University of Michigan Hospital, GI/GU Radiology on the B-1 level. -

Disorders of Defecation
Section V: Disorders of Defecation Disordered defection is a very common problem among individuals of all ages; the continence nurse needs to understand common disorders as a basis for assessment and management. This section will focus on the most common disorders: diarrhea, constipation, obstructed defecation, and irritable bowel syndrome. OBJECTIVES: 1. Define the following terms: diarrhea; functional normal transit constipation; functional slow transit constipation; obstructed defecation; irritable bowel syndrome. 2. Identify etiologic factors for each of the following: diarrhea; functional normal transit and slow transit constipation; obstructed defecation; irritable bowel syndrome. 3. Outline factors to be included in the assessment of an individual with a defecation disorder. 4. Outline options for normalizing stool consistency in the patient with diarrhea and in the patient with constipation. 5. Identify three options for containment of stool in the patient with diarrhea and fecal incontinence, and advantages and disadvantages of each. 6. Discuss indications and options for “top down” versus “bottom up” colonic cleansing programs for the patient with fecal impaction or colonic distention. 7. Identify management guidelines for the patient with functional slow transit constipation. 8. Identify indications for referral of the patient with a defecation disorder. 9. Given a patient situation, provide appropriate assessment and counseling. Emory University WOCNEC Copyright © 2016 97 10. Briefly explain the pathophysiology of “pelvic floor dyssynergia” and options for management. 11. Explain why a woman with a rectocele may need to exert digital pressure against the posterior vaginal wall to effectively empty the rectum. 12. Explain the recommended “hierarchy” of use for laxatives, and identify guidelines for use of each of the following: • bulk laxatives (e.g., psyllium, Citrucel, Fibersure) • osmotic laxatives (e.g., saline laxatives, lactulose, sorbitol, and Polyethylene glycol solutions) • stimulant laxatives (bisacodyl, senna) 13. -

Radiologist Assistant Practice Survey 2015
Radiologist Assistant Practice Survey 2015 Reproduction in any form is forbidden without written permission from publisher © 2015 ASRT. All rights reserved. Radiologist Assistant Practice Survey 2015 1 Table of Contents Executive Summary .......................................................................................................................................................................... 3 Demographics ................................................................................................................................................................................ 3 Facility Demographics .................................................................................................................................................................... 3 Practice and Reporting ................................................................................................................................................................... 3 Demographics ................................................................................................................................................................................... 5 What is your gender? ..................................................................................................................................................................... 5 Are you currently working as a Radiologist Assistant? ................................................................................................................... 5 In what state do you work?