Tick-Borne Pathogens and Diseases in Greece
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Distribution of Tick-Borne Diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2*
Wu et al. Parasites & Vectors 2013, 6:119 http://www.parasitesandvectors.com/content/6/1/119 REVIEW Open Access Distribution of tick-borne diseases in China Xian-Bo Wu1, Ren-Hua Na2, Shan-Shan Wei2, Jin-Song Zhu3 and Hong-Juan Peng2* Abstract As an important contributor to vector-borne diseases in China, in recent years, tick-borne diseases have attracted much attention because of their increasing incidence and consequent significant harm to livestock and human health. The most commonly observed human tick-borne diseases in China include Lyme borreliosis (known as Lyme disease in China), tick-borne encephalitis (known as Forest encephalitis in China), Crimean-Congo hemorrhagic fever (known as Xinjiang hemorrhagic fever in China), Q-fever, tularemia and North-Asia tick-borne spotted fever. In recent years, some emerging tick-borne diseases, such as human monocytic ehrlichiosis, human granulocytic anaplasmosis, and a novel bunyavirus infection, have been reported frequently in China. Other tick-borne diseases that are not as frequently reported in China include Colorado fever, oriental spotted fever and piroplasmosis. Detailed information regarding the history, characteristics, and current epidemic status of these human tick-borne diseases in China will be reviewed in this paper. It is clear that greater efforts in government management and research are required for the prevention, control, diagnosis, and treatment of tick-borne diseases, as well as for the control of ticks, in order to decrease the tick-borne disease burden in China. Keywords: Ticks, Tick-borne diseases, Epidemic, China Review (Table 1) [2,4]. Continuous reports of emerging tick-borne Ticks can carry and transmit viruses, bacteria, rickettsia, disease cases in Shandong, Henan, Hebei, Anhui, and spirochetes, protozoans, Chlamydia, Mycoplasma,Bartonia other provinces demonstrate the rise of these diseases bodies, and nematodes [1,2]. -

Ixodes Ricinus Salivary Serpin Iripin-8 Inhibits the Intrinsic Pathway of Coagulation and Complement
International Journal of Molecular Sciences Article Ixodes ricinus Salivary Serpin Iripin-8 Inhibits the Intrinsic Pathway of Coagulation and Complement Jan Kotál 1,2 , Stéphanie G. I. Polderdijk 3 , Helena Langhansová 1, Monika Ederová 1, Larissa A. Martins 2 , Zuzana Beránková 1, Adéla Chlastáková 1 , OndˇrejHajdušek 4, Michail Kotsyfakis 1,2 , James A. Huntington 3 and JindˇrichChmelaˇr 1,* 1 Department of Medical Biology, Faculty of Science, University of South Bohemia in Ceskˇ é Budˇejovice, Branišovská 1760c, 37005 Ceskˇ é Budˇejovice,Czech Republic; [email protected] (J.K.); [email protected] (H.L.); [email protected] (M.E.); [email protected] (Z.B.); [email protected] (A.C.); [email protected] (M.K.) 2 Laboratory of Genomics and Proteomics of Disease Vectors, Institute of Parasitology, Biology Center CAS, Branišovská 1160/31, 37005 Ceskˇ é Budˇejovice,Czech Republic; [email protected] 3 Cambridge Institute for Medical Research, Department of Haematology, University of Cambridge, The Keith Peters Building, Hills Road, Cambridge CB2 0XY, UK; [email protected] (S.G.I.P.); [email protected] (J.A.H.) 4 Laboratory of Vector Immunology, Institute of Parasitology, Biology Center CAS, Branišovská 1160/31, 37005 Ceskˇ é Budˇejovice,Czech Republic; [email protected] * Correspondence: [email protected] Abstract: Tick saliva is a rich source of antihemostatic, anti-inflammatory, and immunomodulatory molecules that actively help the tick to finish its blood meal. Moreover, these molecules facilitate the Citation: Kotál, J.; Polderdijk, S.G.I.; transmission of tick-borne pathogens. Here we present the functional and structural characterization Langhansová, H.; Ederová, M.; of Iripin-8, a salivary serpin from the tick Ixodes ricinus, a European vector of tick-borne encephalitis Martins, L.A.; Beránková, Z.; and Lyme disease. -

Severe Babesiosis Caused by Babesia Divergens in a Host with Intact Spleen, Russia, 2018 T ⁎ Irina V
Ticks and Tick-borne Diseases 10 (2019) 101262 Contents lists available at ScienceDirect Ticks and Tick-borne Diseases journal homepage: www.elsevier.com/locate/ttbdis Severe babesiosis caused by Babesia divergens in a host with intact spleen, Russia, 2018 T ⁎ Irina V. Kukinaa, Olga P. Zelyaa, , Tatiana M. Guzeevaa, Ludmila S. Karanb, Irina A. Perkovskayac, Nina I. Tymoshenkod, Marina V. Guzeevad a Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russian Federation b Central Research Institute of Epidemiology, Moscow, Russian Federation c Infectious Clinical Hospital №2 of the Moscow Department of Health, Moscow, Russian Federation d Centre for Hygiene and Epidemiology in Moscow, Moscow, Russian Federation ARTICLE INFO ABSTRACT Keywords: We report a case of severe babesiosis caused by the bovine pathogen Babesia divergens with the development of Protozoan parasites multisystem failure in a splenic host. Immunosuppression other than splenectomy can also predispose people to Babesia divergens B. divergens. There was heavy multiple invasion of up to 14 parasites inside the erythrocyte, which had not been Ixodes ricinus previously observed even in asplenic hosts. The piroplasm 18S rRNA sequence from our patient was identical B. Tick-borne disease divergens EU lineage with identity 99.5–100%. Human babesiosis 1. Introduction Leucocyte left shift with immature neutrophils, signs of dysery- thropoiesis, anisocytosis, and poikilocytosis were seen on the peripheral Babesia divergens, a protozoan blood parasite (Apicomplexa: smear. Numerous intra-erythrocytic parasites were found, which were Babesiidae) is primarily specific to bovines. This parasite is widespread initially falsely identified as Plasmodium falciparum. The patient was throughout Europe within the vector Ixodes ricinus. -
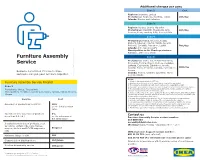
Assembly Leaflet AES ACS
Additional charges per zone Υπηρεσία Zone 2 Cost Regions: Ioannina, Larissa συναρμολόγησης επίπλων Prefectures: Magnesia, Karditsa, Trikala 20€/day Islands: Rhodes and Salamina Zone 3 Regions: Achaea, Chania, Heraklion Prefectures: Chalkidiki, Thesprotia, Arta, 40€/day Preveza, Pieria, Imathia, Pella, Serres, Kilkis Zone 4 Prefectures: Drama, Grevena, Kozani, Kastoria, Rhodope, Kavala, Xanthi, Boeotia, Phthiotis, Corinthia, Rethymno, Lasithi 70€/day © Islands: Argo-Saronic Gulf's Inter IKEA Systems B.V. 2018 B.V. Inter IKEA Systems Municipalities in the Chania prefecture: Kantanos, Selino and Sfakia Furniture Assembly Zone 5 Prefectures: Corfu, Ilia, Aetolia-Acarnania, Service Evrytania, Florina, Phocis, Euboea, Cyclades, Lefkada, Cephalonia, Zakynthos, Argolis, Arcadia, Evros, Messinia, Laconia, Dodecanese, 100€/day Because sometimes it’s nice to have Lesbos Islands: Thasos, Cythera, Sporades, North someone else put your furniture together. Aegean islands Notes: 1. All above listed prices include VAT 24%. Furniture Assembly Service Pricelist 2. Furniture must be located to the space where they will be assembled. 3. The charge for an additional visit, due to customer’s responsibility, is 25€. Zone 1 4. Consumer is not obliged to pay if the notice of payment is not received (receipt-invoice). Prefectures: Attica, Thessaloniki 5. The assembly charge for products purchased from the As-Is Department or with a discount is calculated based on their initial value. Municipalities: Heraklion, Ioannina, Komotini, Larissa, Patras, Rhodes, 6. Disassembly service in the store, applies for the stores IKEA Airport, IKEA Kifissos, IKEA Chania Thessaloniki and IKEA Ioannina. Maximum waiting time is 2 hours. Service is available until 2 hours before closing time of the store. -

Government Spending on Regional Public Services in Greece: Spatial Distribution of Their Evolution Before and During the Financial Crisis
Government spending on regional public services in Greece: Spatial distribution of their evolution before and during the financial crisis. Anastasiou Eugenia1,*, Theodossiou George2, Thanou Eleni3 1 PhD Candidate, Department of Planning and Regional Development, University of Thessaly, Greece 2Associate Professor, Department of Business Administration, TEI of Thessaly 3Lecturer, Graduate Program on Banking, Hellenic Open University *Corresponding author: [email protected], Tel +30 24210 74433 Abstract Greece is still caught in a prolonged recession, which started in 2008. As a result, the economy continues to shrink, which has direct repercussions on the level of private and public consumption as well as on the level government's functions. The present paper attempts to record and depict spatially the evolution of the per capita public spending of the central government on regional services. The specific category of public spending represents a measure of relative welfare as well as a measure of regional development. For the purposes of the research we applied analytical methods such as descriptive statistics and we used specialized mapping analysis programs and geographical information systems (GIS). The evolution over time is observed on the basis of the annual percentage changes of per capita spending. The period of analysis is 2008-2013 and it includes years before the manifestation of the economic crisis as well as the years of the crisis' peak. The thematic maps that were constructed on the basis of the data clearly demonstrate that government spending on the regions was dramatically reduced during the crisis while the period during which the tightening of fiscal policy had a direct impact on the regions stands out. -

Tick Saliva and Its Role in Pathogen Transmission
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by NERC Open Research Archive lyme borreliosis Wien Klin Wochenschr https://doi.org/10.1007/s00508-019-1500-y Tick saliva and its role in pathogen transmission Patricia A. Nuttall Received: 22 February 2019 / Accepted: 9 April 2019 © The Author(s) 2019 Summary Tick saliva is a complex mixture of peptidic cle of egg, larva, nymph, and adult (female or male). and non-peptidic molecules that aid engorgement. Each postembryonic stage generally requires a blood The composition of tick saliva changes as feeding meal before moulting to the next stage [2]. During progresses and the tick counters the dynamic host blood-feeding, ticks acquire infections they may sub- response. Ixodid ticks such as Ixodes ricinus,the sequently transmit when feeding again. When this most important tick species in Europe, transmit nu- occurs, ticks act as vectors of potential pathogens of merous pathogens that cause debilitating diseases, humans and other animals [3]. In fact, ticks are be- e.g. Lyme borreliosis and tick-borne encephalitis. lieved to transmit the greatest variety of infectious Tick-borne pathogens are transmitted in tick saliva agents of any blood-feeding vector. Notable diseases during blood feeding; however, saliva is not simply of humans caused by tick-borne pathogens include a medium enabling pathogen transfer. Instead, tick- Lyme borreliosis, tick-borne encephalitis (TBE), tu- borne pathogens exploit saliva-induced modulation laremia, babesiosis, rickettsiosis, and human granu- of host responses to promote their transmission and locytic anaplasmosis; however, tick-borne infectious infection, so-called saliva-assisted transmission (SAT). -

ANASTASIOS GEORGOTAS “Archaeological Tourism in Greece
UNIVERSITY OF THE PELOPONNESE ANASTASIOS GEORGOTAS (R.N. 1012201502004) DIPLOMA THESIS: “Archaeological tourism in Greece: an analysis of quantitative data, determining factors and prospects” SUPERVISING COMMITTEE: - Assoc. Prof. Nikos Zacharias - Dr. Aphrodite Kamara EXAMINATION COMMITTEE: - Assoc. Prof. Nikolaos Zacharias - Dr. Aphrodite Kamara - Dr. Nikolaos Platis ΚΑΛΑΜΑΤΑ, MARCH 2017 Abstract . For many decades now, Greece has invested a lot in tourism which can undoubtedly be considered the country’s most valuable asset and “heavy industry”. The country is gifted with a rich and diverse history, represented by a variety of cultural heritage sites which create an ideal setting for this particular type of tourism. Moreover, the variations in Greece’s landscape, cultural tradition and agricultural activity favor the development and promotion of most types of alternative types of tourism, such as agro-tourism, religious, sports and medicinal tourism. However, according to quantitative data from the Hellenic Statistical Authority, despite the large number of visitors recorded in state-run cultural heritage sites every year, the distribution pattern of visitors presents large variations per prefecture. A careful examination of this data shows that tourist flows tend to concentrate in certain prefectures, while others enjoy little to no visitor preference. The main factors behind this phenomenon include the number and importance of cultural heritage sites and the state of local and national infrastructure, which determines the accessibility of sites. An effective analysis of these deficiencies is vital in order to determine solutions in order to encourage the flow of visitors to the more “neglected” areas. The present thesis attempts an in-depth analysis of cultural tourism in Greece and the factors affecting it. -

Sofia Bournazi Dynamic Marketing Pro for Northern Greece by Maralyn D
Sofia Bournazi Dynamic Marketing Pro For Northern Greece By Maralyn D. Hill 32 Travel arly October of 2012, I had the pleasure of meeting Sofia Bournazi via e-mail. She was Marketing Director for the Halkidiki Tourism EOrganization and was interested in sponsoring a press trip. As the committee I co-chaired worked putting together this trip, Sofia became a friend and our first trip was organized in May of 2013. Due to the success of the first trip, we worked on a second one for June 2014. This time, my husband Norm and I were fortunate to be part of the group attending. Sofia and I clicked and developed a great appreciation for her marketing ability, work ethic, love of country, and sense of life. Sofia thinks outside the box and has the ability Thessaloniki Photo to pull people together to provide by Maralyn D. Hill successful business and personal relationships and associations. country ends and the other begins; Maralyn: Can you tell us about vice versa. Most people who visit Maralyn: Sofia, what prompted you all we care about is how easy it is how you’ve seen Halkidiki tourism Greece fly from Athens to Santorini to focus on tourism as your career? to travel from one place to another demographics grow since you or Mykonos islands. This means that Sofia: The idea of visiting and if we have something interesting have started that collaboration they already have at least one cosmopolitan places and being part to see or do in a close distance. for tourism? internal flight. -

Ancient History Sourcebook: 11Th Brittanica: Sparta SPARTA an Ancient City in Greece, the Capital of Laconia and the Most Powerful State of the Peloponnese
Ancient History Sourcebook: 11th Brittanica: Sparta SPARTA AN ancient city in Greece, the capital of Laconia and the most powerful state of the Peloponnese. The city lay at the northern end of the central Laconian plain, on the right bank of the river Eurotas, a little south of the point where it is joined by its largest tributary, the Oenus (mount Kelefina). The site is admirably fitted by nature to guard the only routes by which an army can penetrate Laconia from the land side, the Oenus and Eurotas valleys leading from Arcadia, its northern neighbour, and the Langada Pass over Mt Taygetus connecting Laconia and Messenia. At the same time its distance from the sea-Sparta is 27 m. from its seaport, Gythium, made it invulnerable to a maritime attack. I.-HISTORY Prehistoric Period.-Tradition relates that Sparta was founded by Lacedaemon, son of Zeus and Taygete, who called the city after the name of his wife, the daughter of Eurotas. But Amyclae and Therapne (Therapnae) seem to have been in early times of greater importance than Sparta, the former a Minyan foundation a few miles to the south of Sparta, the latter probably the Achaean capital of Laconia and the seat of Menelaus, Agamemnon's younger brother. Eighty years after the Trojan War, according to the traditional chronology, the Dorian migration took place. A band of Dorians united with a body of Aetolians to cross the Corinthian Gulf and invade the Peloponnese from the northwest. The Aetolians settled in Elis, the Dorians pushed up to the headwaters of the Alpheus, where they divided into two forces, one of which under Cresphontes invaded and later subdued Messenia, while the other, led by Aristodemus or, according to another version, by his twin sons Eurysthenes and Procles, made its way down the Eurotas were new settlements were formed and gained Sparta, which became the Dorian capital of Laconia. -

Ehrlichiosis and Anaplasmosis Are Tick-Borne Diseases Caused by Obligate Anaplasmosis: Intracellular Bacteria in the Genera Ehrlichia and Anaplasma
Ehrlichiosis and Importance Ehrlichiosis and anaplasmosis are tick-borne diseases caused by obligate Anaplasmosis: intracellular bacteria in the genera Ehrlichia and Anaplasma. These organisms are widespread in nature; the reservoir hosts include numerous wild animals, as well as Zoonotic Species some domesticated species. For many years, Ehrlichia and Anaplasma species have been known to cause illness in pets and livestock. The consequences of exposure vary Canine Monocytic Ehrlichiosis, from asymptomatic infections to severe, potentially fatal illness. Some organisms Canine Hemorrhagic Fever, have also been recognized as human pathogens since the 1980s and 1990s. Tropical Canine Pancytopenia, Etiology Tracker Dog Disease, Ehrlichiosis and anaplasmosis are caused by members of the genera Ehrlichia Canine Tick Typhus, and Anaplasma, respectively. Both genera contain small, pleomorphic, Gram negative, Nairobi Bleeding Disorder, obligate intracellular organisms, and belong to the family Anaplasmataceae, order Canine Granulocytic Ehrlichiosis, Rickettsiales. They are classified as α-proteobacteria. A number of Ehrlichia and Canine Granulocytic Anaplasmosis, Anaplasma species affect animals. A limited number of these organisms have also Equine Granulocytic Ehrlichiosis, been identified in people. Equine Granulocytic Anaplasmosis, Recent changes in taxonomy can make the nomenclature of the Anaplasmataceae Tick-borne Fever, and their diseases somewhat confusing. At one time, ehrlichiosis was a group of Pasture Fever, diseases caused by organisms that mostly replicated in membrane-bound cytoplasmic Human Monocytic Ehrlichiosis, vacuoles of leukocytes, and belonged to the genus Ehrlichia, tribe Ehrlichieae and Human Granulocytic Anaplasmosis, family Rickettsiaceae. The names of the diseases were often based on the host Human Granulocytic Ehrlichiosis, species, together with type of leukocyte most often infected. -

ESPON ESCAPE Final Report Annex 11
ESCAPE European Shrinking Rural Areas: Challenges, Actions and Perspectives for Territorial Governance Applied Research Final Report – Annex 11 Case Study Kastoria, Western Macedonia, Greece Annex 11 This report is one of the deliverables of the ESCAPE project. This Applied ResearchProject is conducted within the framework of the ESPON 2020 Cooperation Programme, partly financed by the European Regional Development Fund. The ESPON EGTC is the Single Beneficiary of the ESPON 2020 Cooperation Programme. The Single Operation within the programme is implemented by the ESPON EGTC and co-financed by the European Regional Development Fund, the EU Member States and the Partner States, Iceland, Liechtenstein, Norway and Switzerland. This delivery does not necessarily reflect the opinion of the members of the ESPON 2020 Monitoring Committee. Authors Eleni Papadopoulou, Prof. Aristotle University of Thessaloniki, Faculty of Engineering, School of Spatial Planning and Development (Greece) Christos Papalexiou, Dr, Agricultural Engineer - Rural Economist Elena Kalantzi, Spatial Planing and Development Engineer Afroditi Basiouka, MSc, Spatial Planing and Development Engineer, Municipality of Tzumerka, Epirus (Greece) Advisory Group Project Support Team: Benoit Esmanne, DG Agriculture and Rural Development (EU), Izabela Ziatek, Ministry of Economic Development (Poland), Jana Ilcikova, Ministry of Transport and Construction (Slovakia), Amalia Virdol, Ministry of Regional Development and Public Administration (Romania) ESPON EGTC: Gavin Daly, Nicolas Rossignol, -

Ixodes Scapularis) Affected Species: Humans PATHOBIOLOGY and VETERINARY SCIENCE • CONNECTICUT VETERINARY MEDICAL DIAGNOSTIC LABORATORY
Tick Borne Diseases In New England Bullseye rash- common symptom of Lyme disease and STARI Skin lesions- common symptom of Tularemia Tularemia Rocky Mountain Spotted Fever Agent: Rickettsia rickettsii Agent: Francisella tularensis Brown Dog Tick Symptoms: fever, “spotted” rash, headache, nausea, Symptoms: fever, skin lesions in people, vomiting, abdominal pain, muscle pain, lack of appetite, face and eyes redden and become (Rhipicephalus sanguineus) red eyes inflamed, chills, headache, exhaustion Affected Species: humans, dogs Affected Species: humans, rabbits, rodents, cats, dogs, sheep, many Dog Tick mammalian species (Dermacentor variabilis) Ehrlichiosis Agent: Ehrlichia chaffeensis and Ehrlichia ewingii Symptoms: fever, headache, chills, muscle pain, nausea, vomiting, diarrhea, confusion, red eyes Affected Species: humans, dogs, cats Babesiosis Anaplasmosis Agent: Babesia microti Agent: Anaplasma phagocytophilum Symptoms: (many show none), fever, chills, sweats, Lone star tick Symptoms: fever, severe headache, muscle aches, headache, body aches, loss of appetite, nausea chills and shaking, nausea, vomiting, abdominal pain Affected Species: humans (Amblyomma americanum) Affected Species: humans, dogs, horses, cows Borrelia miyamotoi Disease Agent: Borrelia miyamotoi Southern Tick-Associated Lyme Disease Symptoms: fever, chills, headache, body and joint Agent: Borrelia burgdorferi pain, fatigue Rash Illness (STARI) Symptoms: “bullseye” rash Affected Species: humans Agent: Borrelia lonestari (humans only), fever, aching joints, Symptoms: “bullseye” rash, fatigue, muscle pains, headache, fatigue, neurological headache involvement Affected Species: humans Affected Species: humans, Powassan Virus horses, dogs, many others Agent: Powassan Virus Symptoms: (many show none), fever, headache, vomiting, weakness, confusion, loss of coordination, Deer Tick speech difficulties, seizures (Ixodes scapularis) Affected Species: humans PATHOBIOLOGY AND VETERINARY SCIENCE • CONNECTICUT VETERINARY MEDICAL DIAGNOSTIC LABORATORY.