The Anticancer Effects of Cinobufagin on Hepatocellular Carcinoma Huh‑7 Cells Are Associated with Activation of the P73 Signaling Pathway
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bufadienolides from the Skin Secretions of the Neotropical Toad Rhinella Alata (Anura: Bufonidae): Antiprotozoal Activity Against Trypanosoma Cruzi
molecules Article Bufadienolides from the Skin Secretions of the Neotropical Toad Rhinella alata (Anura: Bufonidae): Antiprotozoal Activity against Trypanosoma cruzi Candelario Rodriguez 1,2,3 , Roberto Ibáñez 4 , Luis Mojica 5, Michelle Ng 6, Carmenza Spadafora 6 , Armando A. Durant-Archibold 1,3,* and Marcelino Gutiérrez 1,* 1 Centro de Biodiversidad y Descubrimiento de Drogas, Instituto de Investigaciones Científicas y Servicios de Alta Tecnología (INDICASAT AIP), Apartado 0843-01103, Panama; [email protected] 2 Department of Biotechnology, Acharya Nagarjuna University, Nagarjuna Nagar, Guntur 522510, India 3 Departamento de Bioquímica, Facultad de Ciencias Naturales, Exactas y Tecnología, Universidad de Panamá, Apartado 0824-03366, Panama 4 Smithsonian Tropical Research Institute (STRI), Balboa, Ancon P.O. Box 0843-03092, Panama; [email protected] 5 Centro Nacional de Metrología de Panamá (CENAMEP AIP), Apartado 0843-01353, Panama; [email protected] 6 Centro de Biología Celular y Molecular de Enfermedades, INDICASAT AIP, Apartado 0843-01103, Panama; [email protected] (M.N.); [email protected] (C.S.) * Correspondence: [email protected] (A.A.D.-A.); [email protected] (M.G.) Abstract: Toads in the family Bufonidae contain bufadienolides in their venom, which are charac- Citation: Rodriguez, C.; Ibáñez, R.; terized by their chemical diversity and high pharmacological potential. American trypanosomiasis Mojica, L.; Ng, M.; Spadafora, C.; is a neglected disease that affects an estimated 8 million people in tropical and subtropical coun- Durant-Archibold, A.A.; Gutiérrez, M. tries. In this research, we investigated the chemical composition and antitrypanosomal activity Bufadienolides from the Skin of toad venom from Rhinella alata collected in Panama. -

Pharmaceutical Sciences
JOURNAL OF Pharmaceutical Sciences December 1967 volume 56, number 12 ___ Review Article __ Pharmacology and Toxicology of Toad Venom By K. K. CHEN and ALENA KOVARiKOVA CONTENTS speare made the witch throw a toad into the hell-broth. It has been long believed that han- HISTORY.. 1535 dling of toads causes warts. In a small area of CHEMICALINGREDIEXTSOF TOADPOISOX. 1536 Pharmacology of Bufadienolides. 1536 the state of Illinois, folklore has 300 references Bufagins. .... 1536 to warts of toad origin, particularly their cures (2). Bufotoxins. ... .. .. 1538 These superstitions can of course be disproved Clinical Trials... .... 1539 by laboratory experience. Houssay (3) op- Catecholamines. .. .. 1539 Epinephrine.. .. .. .. 1539 erated on 15,000 toads for endocrine studies and Norephinephrine.. .. .. .. .. 1539 we handled more than 10,000 toads for the Indolealkylamines..... 1539 collection of their poisons-with no ill effects. Noncardiotonic Sterols. .. 1540 In form of a votive animal, the toad is associated Cholesterol. ... .. .. ... .. .. 1540 with the uterus and various gynecological dis- Provitamin D. .. .. 1540 -v-Sitosterol .......... ... .. .. 1540 eases (4) in Central Europe. Bronze toads of Miscellaneous Substances.. 1540 the Perm culture of Kortheastern Russia were USE OF THE VENOMTO THE TOAD. 1540 among the archaeological findings dating from Protection from Enemies. 1540 the middle of the 1st century A.D. Significance to Behavior. 1540 ="ATURALTOLERANCETO CARDIACGLYCO- Toad medicine has been advocated all over SIDESANDAGLYCONES. 1540 the world. For many years the Chinese have RESPONSEOFOTHERTISSUESTODRUGS. 1541 used a preparation of toad venom, ch'an su, REFERENCES. 1541 for the treatment of canker sores, toothache, HISTORY sinusitis, and local inflammations (5). During the 15th century a European physician wrote a FOR CENTURIES the toad has been known to book, "De Vcnenis," in which he mentioned that produce a poisonous secretion. -

World Journal of Pharmaceutical Research Pradhan Et Al
World Journal of Pharmaceutical Research Pradhan et al. World Journal of Pharmaceutical SJIF ImpactResearch Factor 6.805 Volume 5, Issue 8, 426-443. Review Article ISSN 2277– 7105 ` BUFO SKIN-SECRETIONS ARE SOURCES OF PHARMACOLOGICALLY AND THERAPEUTICALLY SIGNIFICANT COMPOUNDS Dr. Bishnu Charan Pradhan*1 and Shakti Prasad Pradhan2 1Dept. of Zoology Angul Mahila Mahavidyalaya, Angul, Odisha, India. 759122. 2Dept. of Pharmacy. Utkal University, Vanivihar, Bhubaneswar, Odisha, India. ABSTRACT Article Received on 07 June 2016, Amphibians have been occupying a wide range of habitats since they Revised on 28 June 2016, evolved around 363 million-years-ago. Along with legs and lungs, skin Accepted on 18 July 2016 DOI: 10.20959/wjpr20168-6752 played an important role in survival of amphibians and made it possible for them to exploit diverse ecological conditions. Amphibian skin not only helps in avoiding desiccation but also helps in imposing *Corresponding Author Dr. Bishnu Charan defense against predators as well as pathogens. Amphibian skin Pradhan possesses wide variety of chemical compounds, which have potential Dept. of Zoology Angul significance in pharmacology and therapeutics. Toads especially those Mahila Mahavidyalaya, belonging to genus Bufo, are outstanding source of useful granular- Angul, Odisha, India. 759122. gland secretions. Compounds derived from toad skin-secretions can be used as analgesics, painkillers and as medicine against cardiac- problems, multi-drug resistant bacteria, HIV and Cancer. KEYWORDS: Bufadienolides, pharmacology, Bufo skin-secretions, toxins. INTRODUCTION Amphibians started trolling the landmasses of earth about 363 million-years-ago, with Acanthostega and Ichthyostega probably being the earliest of known amphibians (Evans[20] et al 1998). Fossil records elucidate that ancestors of modern amphibians like Frogs, Toads, Caecilians and Salamanders probably evolved about 200 million years ago during the Triassic period. -

British Chemical Abstracts
BRITISH CHEMICAL ABSTRACTS A.-PURE CHEMISTRY MARCH, 1934. General, Physical, and Inorganic Chemistry. Theory of hyperfine structures. E. Fermi and Infra-red grating spectra and spectral series E. SEGRi: (Mem. R. Accad. d’ltalia Sci. fis., 1933, 4, (A1II, A11, He I and n, Zn I and II). F. Paschen 131—158).—A theoretical discussion of the hyperfine and R. Ritsciil (Ann. Physik, 1933, [v], 18 , 867— structure of the spectral lines of Li, Na, Cu, Ga, lib, 892).—A comprehensive analysis of the grating spec Cd, In, Cs, Ba, Au, Hg, Tl, Pb, and Bi. The theory trum of A in is made. With a specially luminous of the nuclear magnetic moment is discussed. hollow cathode arrangement new infra-red lines 0. J. W. beyond 1 ¡j. are tabulated and an extended analysis is Spectrum of atomic nitrogen, N I. D. Seeerian given for A11, He i and it, Zn i and rr. W. R. A. (Compt. rend., 1934, 198, 68—69).—An arc is struck Arc spectrum of silicon in the red and infra between parallel W wires 3 mm. diam. and 2—3 mm. red. C. C. Kiess (Bur. Stand. J. Res., 1933, 11, apart, N2 at the rate of 800—1000 litres per hr. being 775—782).—130 new lines have been measured in the passed around them. With a.c. of 46—50 amp. at arc spectrum of Si between 6125 and 11,290 A . These 110 volts the spectrum of N i is obtained (cf. A., 1929, include the strongest previously unidentified Fraun 1116; 1932, 103), and also two different continuous hofer line (6155 A.) and other solar spectral lines. -

Strictly, Especially the Occasional Inspection Of-Our Mem¬ Permit, At
years ; and this requirement, if it were carried out mittee appointed for that purpose; at least two men strictly, especially the occasional inspection of-our mem¬ should be required for the inspection of any school, and bers, would at once strengthen and broaden the influence the report should be in writing for future reference. of this association and commend it to the state board of 3. The interests of the association demand that the examiners, do much to quiet the present state of unrest work be divided up so as to utilize as many men and and dissatisfaction existing in many medical schools and their influence as possible, if we would broaden our field elevate medical teaching in the eyes of the public out of of usefulness in both higher educational and moral or its present questionable status. ethical standing sufficiently to make membership an Standards acceptable to examining boards could be honor so distinctive that all good schools will desire the established and the variable demand of the different connection. states be gradually molded into a universal and much- 4. At present the four-year high school, or the four¬ needed standard agreeable to all. The result would be teen units for entrance and a four-year strictly graded better-prepared and more uniformly educated physicians, course of study of 4,000 hours is as high as the condi¬ and more ethical relations between the profession and tions of education will permit. the people. The time is ripe for some organized body to 5. If an additional year is wise, then a fifth year assume command and restore confidence by combining following the present four-year plan, which shall be the good accomplished by the several organizations labor¬ strictly practical and bedside in hospital wards, is pre¬ ing in the field. -

Biological Activities of Nanomaterials (Bufadienolides, Peptides and Alkoloids) in the Skin of Amphibian on Gammarus Pulex L
Digest Journal of Nanomaterials and Biostructures Vol. 5, No 2, April 2010, p. 347 – 354 BIOLOGICAL ACTIVITIES OF NANOMATERIALS (BUFADIENOLIDES, PEPTIDES AND ALKOLOIDS) IN THE SKIN OF AMPHIBIAN ON GAMMARUS PULEX L. VAHDETTİN BAYAZİT* Muş Alparslan University, Faculty of Arts and Sciences, Department of Biology, 49100, Muş, Turkey, Phone The purpose of this sudy was to examine the toxic effects of bufadienolides of antimicrobial peptides and alkoloids on Gammarus pulex L.(Crustacea:Amphipoda:Gammaridae) Bufadienolides (Arenobufagin, Arenobufagin hemisuberate, Arinobufagin 3- sulfate, Bufalin, Bufalin hemisuberate, Bufoatlin 3-sulfate, Bufotalinin, Bufotalone, Cinobufagin, Cinobugagilon, Cinobufotalin, Desacetylcinobufagin, Gamabufotalin hemisuberoate, Gamabufotalin 3-sulfate, 15- hydroxybufalin, 19-hydroxybufalin, Marinobufagin, Marinoic acid, Marinosin and Resibufaginol), Amphibian peptides (Caerin 1.1, Caerin 1.9, Caerin 4.1, Dahlein 5.6, Dermaseptin, Esculentin-1ARb, Esculentin-2P, Maculatin 1.1, Magainin II, MRP, Palustrin-3AR, Ranatuerin-6, Ranatuerin-2P, Uperin 3.6, RCCP) and Alkoloids (Samandarine, Batrachotoxin, Histrionictoxin, Pumiliotoxin, Allopumiliotoxin, Homopumiliotoxin, Decahydroquinoline, Epibatidine) killed significantly the animals in the experimental groups (p< 0.01). (Received March 2, 2010; accepted April 21, 2010) Keywords: Bufadienolides,Amphibian peptides and alkoloids Gammarus pulex, 1. Introductıon Amphibian skin secretions are considered a rich source of biologically active compounds and are known to be rich in peptides, bufadienolides and alkaloids. Bufadienolides are cardioactive steroids from animals and plants that have also been reported to possess antimicrobial activities. Amphibian skin contains a remarkable spectrum of biologically active compounds, including biogenic amines, peptides, proteins, bufadienolides, tetrodotoxins and lipophilic alkaloids[1-7]. The lipophilic alkaloids include the samandarines and an incredible array of piperidine-based, pyrrolidine-based, and steroidal alkaloids. -

Effect of Exposure to Deltamethrin on the Bufadienolide Profiles in Bufo
RSC Advances View Article Online PAPER View Journal | View Issue Effect of exposure to deltamethrin on the bufadienolide profiles in Bufo bufo gargarizans Cite this: RSC Adv.,2019,9,1208 venom determined by ultra-performance liquid chromatography-triple quadrupole mass spectrometry Jing Zhou,* Huacong Zhao, Luyao Chen, Xiaowei Xing, Tingmei Lv, Xinyi Yang, Qinan Wu, Jinao Duan and Hongyue Ma * The population of Bufo bufo gargarizans Cantor in China has been alarmingly declining due to environmental pollution. Deltamethrin is a pyrethroid pesticide frequently used in agriculture and much of its residues are present in crops, soil and water. Deltamethrin has been shown to have toxicity to toads. Herein, we assumed that deltamethrin contamination might influence the biosynthesis of toxic Creative Commons Attribution 3.0 Unported Licence. substances present in toad venom. Bufadienolides present in venom are the toad's chemical defense and highly toxic to predators, and they are important for the survival of toad species against predators. In this study, we determined the contents of bufadienolides in toad venom using a HPLC-triple quadrupole mass spectrometer to evaluate the change in bufadienolide profiles in toad venom before and after cutaneous exposure to deltamethrin. The results indicated that toads exposed to high concentration of deltamethrin survive the least, do not exuviate, and their movements are stiff. Furthermore, it was observed that high level of deltamethrin contamination induces a marked decrease in the levels of toxic Received 21st September 2018 bufadienolides in toad venom. These changes in the toxin profiles could lead to the compromised Accepted 2nd December 2018 chemical defense of toad, leading to more susceptible to attack by predators. -

Occurrence of Marinobufotoxin and Telocinobufotoxin Homologs in the Skin of Bufo Bankorensis Borbour1) KAZUTAKE SHIMADA, YOSHI
2300 Vol. 35 (1987) Chem. Pharm. Bull. 35( 6 )2300-2304(1987), Occurrence of Marinobufotoxin and Telocinobufotoxin Homologs in the Skin of Bufo bankorensis BORBOuR1) KAZUTAKESHIMADA, YOSHIHIRO SATO, and TOSHIONAMBARA* PharmaceuticalInstitute, Tohoku University, Aobayama, Sendai 980, Japan (ReceivedNovember 13, 1986) The occurrenceof marinobufagin3-succinyl-L-arginine and 3-glutaryl-L-arginineesters, and telocinobufagin3-glutaryl-L-arginine ester, together with seven known bufogenins, in the skinof Bufo bankorensisBORBOUR, is reported. The structureswere elucidatedby degradativemeans and/ordirect comparisonwith authenticsamples. These compounds were assayed for inhibitory activitytowards guinea pig heart Na+, K+-adenosine triphosphatase. Keywords-Bufo bankorensis;toad venom; bufogenin;marinobufotoxin homolog; telo- cinobufotoxinhomolog; sodium-potassium-activated ATPase inhibition In a series of studies on toad venom,2) we characterized the cardiac steroids in the skin of Formosan toad, Bufo bankorensis BORBOUR, and assayed them for Na +-adenosine triphosphatase (Na+, K +-ATPase; EC 3.6.1.3) inhibitory activity.3) Five toads were sacrificed by freezing in dry ice, and the skins were immediately flayed off and extracted with ethanol. The ethanolic extract was concentrated in vacuo and the residue was subjected to column chromatography on silica gel. Subsequent separation of the bufogenin and bufotoxin mixture was repeatedly done by high-performance liquid chromat- ography (HPLC) on a reversed-phase column. Three new bufotoxins (5a, 5b, 10) were isolated as colorless amorphous substances, which gave negative ninhydrin and positive Sakaguchi tests. Upon hydrolysis with 6 N hydrochloric acid, arginine was produced and identified by thin-layer chromatography (TLC). When subjected to enzymic hydrolysis with a hog pancreas lipase preparation followed by methylation with diazomethane, these bufotoxins afforded bufogenin 3-hemi- carboxylate methyl esters (3a, 3b, 8). -

China Medical Journal
THE China Medical Journal P u b l is h e d by m The China Medical Missionary Association 1918 S H A N G H A I : P r i n t e d by t h e P resbyterian M issio n P r ess 1918 INDICES TO Wut €lún<t Jtttbiml Journal Volume XXXII, 1918. G e n e r a l I n d e x . Page. Abdominal cavity, Phagocytosis in, (277) ......................... ... 50 Abdominal surgery under local anaesthesia ... .............. .................... 282 Wall, Cy»t in, Containing Ascarides ......................... ... Dr. D a l e . 131 Abdominal Wounds ........................................................... ••• ••• ... 76 Abortion, Corpus luteurn extract to prevent ....................... 389 Acidity, Gastric, of healthy Japanese, (330)......................... ... 174 Atropin test for typhoid fe v e r ................................................ 382 Andrenalin Injections, and Viscosity of Blood, (328) ... 174 Adrenalin Content of Suprarenals in Beri-beri, (334) ... 177 In extirpation of Pancreas, (421)..................................... 473 Adenoma, Papillary, of Jejunum ..................................... Dr. L u d l o w . 425 Age, Foetal, as Determined by Dried Skeleton, (371) 263 Aged, Surgery o f ....................................................................... 591 “ Akamuslii,” Vectur of Japanese River Fever, (301) ... 57 Albumin, Serum, Anaphylaxis induced by, (358) ... ... 259 Alcohol, Moderate Use of as Beverage ......................... ... 167 Resolutions 011 Use of ................................................ 165 Alcoholism in China ........................................................... -

The Spinal Microglial IL-10/Β-Endorphin Pathway Accounts for Cinobufagin-Induced Mechanical Antiallodynia in Bone Cancer Pain F
Apryani et al. Journal of Neuroinflammation (2020) 17:75 https://doi.org/10.1186/s12974-019-1616-z RESEARCH Open Access The spinal microglial IL-10/β-endorphin pathway accounts for cinobufagin-induced mechanical antiallodynia in bone cancer pain following activation of α7-nicotinic acetylcholine receptors Evhy Apryani, Usman Ali, Zi-Ying Wang, Hai-Yun Wu, Xiao-Fang Mao, Khalil Ali Ahmad, Xin-Yan Li* and Yong-Xiang Wang* Abstract Background: Cinobufagin is the major bufadienolide of Bufonis venenum (Chansu), which has been traditionally used for the treatment of chronic pain especially cancer pain. The current study aimed to evaluate its antinociceptive effects in bone cancer pain and explore the underlying mechanisms. Methods: Rat bone cancer model was used in this study. The withdrawal threshold evoked by stimulation of the hindpaw was determined using a 2290 CE electrical von Frey hair. The β-endorphin and IL-10 levels were measured in the spinal cord and cultured primary microglia, astrocytes, and neurons. Results: Cinobufagin, given intrathecally, dose-dependently attenuated mechanical allodynia in bone cancer pain rats, with the projected Emax of 90% MPE and ED50 of 6.4 μg. Intrathecal cinobufagin also stimulated the gene and protein expression of IL-10 and β-endorphin (but not dynorphin A) in the spinal cords of bone cancer pain rats. In addition, treatment with cinobufagin in cultured primary spinal microglia but not astrocytes or neurons stimulated the mRNA and protein expression of IL-10 and β-endorphin, which was prevented by the pretreatment with the IL- 10 antibody but not β-endorphin antiserum. Furthermore, spinal cinobufagin-induced mechanical antiallodynia was inhibited by the pretreatment with intrathecal injection of the microglial inhibitor minocycline, IL-10 antibody, β- endorphin antiserum and specific μ-opioid receptor antagonist CTAP. -

Elsberg's Surgery of the Spinal Cord
Vol. XXX, No. 6. NOVEMBER, 1916 Published Bi-Mpnthly by the MEDICAL MISSIONARY ASSOCIATION OF CHINA. Editor, K. M. Merrinj, M.D., St. J ohn?s University, Shanghai. Husinesa Manager, D f. R . 1 C , Beebe, 5 Qulnsan Qasdeasy, Shanghai. «**''*'' Sec'y and Treas., H. H. Morris, M.D., 4B Minghàng Road, / f*, Shanghai. r 1 1 -- TABLE OF CONTENTS. ORIGINAL : Page. Page. ^ s s a r V’ On the Evils of Chinese Foot-binding. The EducationaPStaadaFdofucationarStaadaFdof ’Ffe-Medi- i J. Preston Maxwell, M.D., F.R.C.S. 393 cal and Medical, of Mission Medical Schools. Edward M. Merrins.M.D. 421 Acute Complete Inversion of the Uterus. EDITORIAL: Chinese Medicine and Sur M. h. Hanington, M.B., M.D., C.M. 396 gery. C. M. M. A., Constitution and By laws. Medical Education in China.- Re Ovarian Tumours and Ovariotomy. M. port of First Meeting of ünion Committee Edith Bryson, M.B., Ch.B., and J. on Medical Terminology. National Health, H. Montgomery, M.B., Ch.B. ... 400 Essay Contest ... ... ... 432-441 Plastic Closure of Buccal Cavity Follow Medical Reports ... .............. ... 442 ing Gun-shot Injury. Carl A. Hed- Medical and Surgical Progress ... ... 448 blom, M.D. ............... 407 “ Needling ” Painful Spots, as Practised Japanese Medical Literature ... ... 460 by the Chinese. James Cantlie, M.A., Book Reviews ... ... 466 M.B., F.R.C.S........................... ... 410 Clinical Notes ........................................ 413 Correspondence ... f 73 Customs Medical Report: Health of News and Comment ... ...474 Chinkiang. By Hermann Balean, M.D.i B.Sc. (Lond.), F.R.C.S. ... 417 Nurses’ Association of China ... ... 476 V JUST READY Elsberg’s Surgery of the Spinal Cord There is no other book published like this by Dr* IJlsberg. -
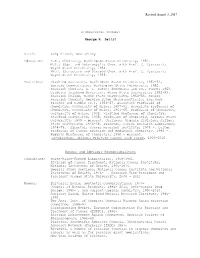
Revised August 3, 2017
Revised August 3, 2017 BIOGRAPHICAL SUMMARY George R. Pettit Birth: Long Branch, New Jersey Education: B.S., Chemistry, Washington State University, 1952. M.S., (Syn. and Heterocyclic Chem. with Prof. C. Djerassi), Wayne State University, 1954. Ph.D. (Structure and Steroid Chem. with Prof. C. Djerassi), Wayne State University, 1956. Positions: Teaching Assistant, Washington State University, 1950-52, Lecture Demonstrator, Washington State University, 1952. Research Chemist, E. I. DuPont deNemours and Co., Summer 1953. Graduate Teaching Assistant, Wayne State University, 1952-53. Research Fellow, Wayne State University, 1954-56. Senior Research Chemist, Norwich Eaton Pharmaceuticals, Inc.(now Procter and Gamble Co.), 1956-57. Assistant Professor of Chemistry, University of Maine, 1957-61. Associate Professor of Chemistry, University of Maine, 1961-65. Professor of Chemistry, University of Maine, 1965. Visiting Professor of Chemistry, Stanford University, 1965. Professor of Chemistry, Arizona State University, 1965 - present. Chairman, Organic Division, Arizona State University, 1966-68. Director, Cancer Research Laboratory, 1974-75. Director, Cancer Research Institute, 1975 -. Dalton Professor of Cancer Research and Medicinal Chemistry, 1986 -. Regents Professor of Chemistry, 1990 - present. Co-Director, Arizona Prostate Cancer Task Force, 2000-2010. Honors and Advisory Responsibilities Consultant: Smith-Kline-French Laboratories, 1959-1961. Division of Cancer Treatment, National Cancer Institute, National Institutes of Health, 1965-1976. Special Study Sections, National Cancer Institute and National Institutes of Health, 1976- . Research Vice President and President Oregon State University, 2006 - 2011 Member: Editorial Board, Synthetic Communications, 1970- Journal of Natural Products, l984- 2011, Anti-Cancer Drug Design, 1990- , and Current Organic Chemistry, 1997-2010. Advisory Board, Walter Reed Medical Research Institute, 1985- 1990.