University of Port Harcourt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Final (Report) Word Doc Embedding Environmental
EMBEDDING ENVIRONMENTAL PROTECTION and HEALTH VALUES for SUSTAINABLE DEVELOPMENT in GREATER PORT HARCOURT COMMUNITIES Anthony Wakwe Lawrence* and Ibisime Etela** *Community Inter-Relations and Conciliation Initiative (CIRCI) http://www.circi-ngo.org **University of Port Harcourt (UniPort) http://www.uniport.edu.ng with support from Prof. Onyewuchi Akaranta1 RCE Port Harcourt http://www.uniport.edu.ng Abstract Rapid environmental degradation, oil pollution and resource erosion in the Niger Delta of Nigeria prompted Shell Petroleum Development Company of Nigeria Limited (SPDC) to sponsor a series of awareness campaigns and two-day workshops in rural communities on aspects of the new Sustainable Development Goals for 18 rural communities in Greater Port Harcourt and neighboring areas of Rivers State. About 1,200 participants (elders; women; youths) from 18 rural communities were trained on principles of sustainable development, benefits of protecting the environment, and in some of the communities this included healthy stress-free living lifestyle. Participants appreciated biodiversity conservation, dangers of illicit drug and alcohol use, prevention of and care for people living with HIV/AIDS, and the dangers associated with oil pipeline vandalism. More strategic partnerships and increased funding support from more governmental and nongovernmental partners are needed Paper presented at the 6th African RCE Conference, jointly organised by NEMA-Kenya and UNU-IAS, Tokyo, Japan from 24-26 August 2016, Kenyatta University, Nairobi, Kenya. to conduct post-training impact assessment studies and for project scale-up via Train-the-Trainers workshops to new and the 18 communities already visited. Introduction The Regional Centre of Expertise (RCE) Port Harcourt, formally, acknowledged on 24th June 2015 by the United Nations University - Institute of Advanced Study of Sustainability (UNU-IAS), Tokyo Japan. -

Ikwerre Intergroup Relations and Its Impact on Their Culture
83 AFRREV VOL. 11 (2), S/NO 46, APRIL, 2017 AN INTERNATIONAL MULTI-DISCIPLINARY JOURNAL, ETHIOPIA AFRREV VOL. 11 (2), SERIAL NO. 46, APRIL, 2017: 83-98 ISSN 1994-9057 (Print) ISSN 2070-0083 (Online) DOI : http://dx.doi.org/10.4314/afrrev.v11i2.7 Ikwerre Intergroup Relations and its Impact on Their Culture Chinda, C. Izeoma Department of Foundation Studies Port Harcourt Polytechnic, Rumuola Phone No: +234 703 667 4797 E-mail: [email protected] --------------------------------------------------------------------------- Abstract This paper examined the intergroup relations between the Ikwerre of the Niger Delta, South-South geopolitical zone of Nigeria and its impact on their culture. It analyzed the Ikwerre relations with her Kalabari and Okrika coastal neighbours, as well as the Etche, Eleme, Ekpeye, Ogba Abua and the Igbo of Imo state hinterland neighbours. The paper concluded that the internal developments which were stimulated by their contacts impacted significantly on their culture. Key words: Ikwerre, Intergroup Relations, Developments, Culture, Neighbour. Introduction Geographical factors aided the movement of people from one ecological zone to another in migration or interdependent relationships of trade exchange. These exchanges and contacts occurred even in pre-colonial times. The historical roots of inter-group relations of the Ikwerre with her neighbours, dates back to pre-colonial times but became prevalent from the 1850 onward when the Atlantic trade became emphatic on agrarian products as raw materials to the industrial western world. This galvanized the hitherto existing inter-group contact between the Ikwerre and her neighbouring potentates. Copyright © International Association of African Researchers and Reviewers, 2006-2017: www.afrrevjo.net. -

Democracy and Poverty Reduction in Nigeria: a Case Study of Rivers State: 1999 – 2007
Journal of Language, Technology & Entrepreneurship in Africa, Vol.2. No.2 2010 DEMOCRACY AND POVERTY REDUCTION IN NIGERIA: A CASE STUDY OF RIVERS STATE: 1999 – 2007 Nekabari Johnson Nna & Prince Ikechukwu Igwe ABSTRACT This paper seeks to examine the extent to which Nigeria’s democratic experience (1999-2007) has elevated the living standards of the majority of the people. It specifically aimed at search lighting the impact of the regime’s key poverty reduction strategies vis-à-vis the overall poverty situation in the country in general and Rivers State in particular. The study focused on two poverty reduction strategies: National Poverty Eradication Programme (NAPEP) and the Rivers State Economic Empowerment and Development Strategy (RIVSEEDS). The study utilized the primary and secondary sources of data in realizing its central objective. The Participatory Poverty Assessment (PPA) method was also adopted in the course of this research work. The sample population was drawn from ten Local Government Areas (LGAs) of Rivers State; Port Harcourt, Obio/Akpor, Ikwerre, Emohua, Etche, Omuma, Ahoada East, Ahoada West, Abua/Odual and Ogba-Egbema-Ndoni LGAs. The research work employed the Political Economy (P.E.) method of analysis. The PE approach elucidates in very clear terms how the policies and reforms of successive governments in Nigeria have debilitated the productive forces of a great number of her population. The findings of this study showed that the democratic experience has impacted little to the poverty situation of the people of Rivers State. It also revealed that the present government’s poverty reduction programme is yet to be complemented by other macroeconomic policies to yield the desired results of poverty reduction, wealth creation and capacity building. -

World Bank Document
SFG2386 V4 Public Disclosure Authorized ENVIRONMENTAL AND SOCIAL MANAGEMENT PLAN (ESMP) Draft Report For PUBLIC WORKS – Road Maintenance Public Disclosure Authorized (90 Lots) in Twenty-three Local Government Areas, Rivers State Public Disclosure Authorized By Public Disclosure Authorized Rivers State Employment and Expenditure for Results Project (SEEFOR), Ministry of Budget & Economic Planning Under the World Bank Assisted Project and European Union July, 2017 SEEFOR Intervention Works, Road Maintenance, Rivers State Table of Contents Content Page Title Cover i Table of Contents ii List of Tables iii List of Acronyms iv Executive Summary v CHAPTER ONE: Introduction 1 1.1 Background 1 1.2 The Project Invention Locations 1 1.3 Description of Proposed Activities 1 1.4 Need for ESMP 2 1.5 Approaches for Preparing the ESMP 2 1.5.1 Literature Review 2 1.5.2 Field Visits 2 CHAPTER TWO: Institutional and Legal Framework for Environmental Management 3 2.1 Introduction 3 2.2 Federal Policy/Legislation 3 2.2.1 National Policy on Environment 3 2.2.2 Federal EIA Act No. 86, 1992 3 2.3 Rivers State Environment Protection Law No. 2, 1994 3 2.4 World Bank Safeguards Policy Triggered by SEEFOR & the Proposed Project 3 CHAPTER THREE: Biophysical Environment 4 3.1 Introduction 4 3.2 Project Location 4 3.3 Geology and Ecological Zones 4 3.4 Climate and Rainfall 4 3.5 Waste and Waste Management 4 3.6 Air Quality and Noise Level 4 3.7 Population of the Intervention Areas 4 3.8 Economy and Source of Livelihood 4 3.9 Culture of the People ` 4 3.10 Social Structure -

Background to Environmental Degradation in Ogoniland
Background to Environmental Degradation in Ogoniland An Ogoni woman draws water from an open well. With a rich and diverse culture, the Ogoni have lived in the Niger Delta for hundreds of years © UNEP UNEP ENVIRONMENTAL ASSESSMENT OF OGONILAND Agbada Formation and Akata Formation. The Background to Benin Formation is comprised of multiple layers Environmental of clay, sand, conglomerate, peat and/or lignite, all of variable thickness and texture and covered by Degradation in overburden soil. Clay beds are discontinuous and groundwater is therefore present both as localized Ogoniland aquifers or in hydraulically interconnected aquifers. The ground characteristics are consistent Ogoniland is characterized by typically deltaic with deltaic environments, where erosion and features: uneven terrain, numerous creeks, shallow deposition of sediments constantly shift the course brackish water bodies and a variety of vegetation of channels, tributaries and creeks. types including swamp forest. The following section describes in detail Ogoniland’s environmental Groundwater setting and oil industry operations. Ogoniland’s aquifers are a crucial resource upon 2.1 Environmental setting in which the region’s entire population depends for Ogoniland and the Niger Delta drinking water. The protection of these aquifers is therefore vital. These aquifers are very shallow, with Geology the top-most groundwater levels occuring anywhere between close to the surface and a depth of 10 The Niger Delta is the product of both fluvial metres. To tap the aquifers, Ogoni communities and marine sediment build-up since the upper typically construct open, hand-dug wells about Cretaceous period, some 50 million years ago. 60 cm in diameter and water is abstracted either Over time, up to 12,000 metres of shallow manually or with pumps. -

An Assessment of Socio-Economic Benefits of Improved Rural Road in a Nigeria L.G.A
IOSR Journal of Environmental Science, Toxicology and Food Technology (IOSR-JESTFT) e-ISSN: 2319-2402,p- ISSN: 2319-2399.Volume 13, Issue 6 Ser. II (June. 2019), PP 25-31 www.iosrjournals.org An Assessment of Socio-Economic Benefits of Improved Rural Road in A Nigeria L.G.A. Ubani Princewill1, Adiele Kinsley Chinyere2, Neebee Bonny3 1Department of Urban and Regional Planning, Ken Saro - Wiwa Polytechnic Bori, Nigeria, 2Department of Building Technology, Captain ElechiAmadi Polytechnic, Port Harcourt Nigeria 3Department of Urban and Regional Planning, Ken Saro - Wiwa Polytechnic Bori, Nigeria, Corresponding Author: Ubani Princewill1 Abstract: This research assessed and x-rays the relationship between resident’s socio-economic benefit and the improved rural road project in omuma local government area of Rivers state Nigeria. Two specific objectives measured were; to identify socioeconomic benefits of improved rural community road from the study area, andexamine the relationship between improved rural community road and socio- economic benefits of residents in the study area (improved income, quantity of high institutions, human population increase and quantity of churches). The questionnaire structured on 5 likert scalewas used to drawn information from residents while other information was obtained throughfield observation and environmental contact. The study identify the socio- economic benefits and found out thataccessibility to market/connectivity, foreign investors association, importation and exportation of agrarian product, employment increase, reduction of transportation cost, eradication of poverty rate, improved income, human population increase, reduction in cost of food, increase of social relation, land value appreciation, quantity of educational institution and increase in number of churches are the 13 identified socioeconomic benefit of improved rural road in omuma. -

Invitation to Tender River State Universal Basic Education Board (Rsubeb)
INVITATION TO TENDER RIVER STATE UNIVERSAL BASIC EDUCATION BOARD (RSUBEB) The Government of Rivers State of Nigeria has received the 2017 FGN/ UBE Intervention Funds from the Federal Government of Nigeria towards the cost of Universal Basic Education Intervention Projects and intends to apply part of the funds to cover eligible payments under the Contract for the Construction and Reconstruction of Early Child Care Development Education (E.C.C.D.E.), Primary & Junior Secondary Schools; Fencing & Landscaping of Schools; Fabrication and Supply of Pupils and Students Desks, Teachers/ Headmasters/Principals Furniture; Procurement and Supply of Sports, Agricultural Equipment and the Procurement and Supply of Office Furniture and Equipment for which this invitation is issued. The Rivers State Universal Basic Education Board, Port Harcourt now invites sealed Tenders from reputable Contractors/ Suppliers for the above mentioned Projects as in the Schedule below: 2017 Civil Works: PHYSICAL INFRASTRUCTURE FOR E.C.C.D.E PRIMARY AND JUNIOR SECONDARY SCHOOLS CIVIL INFRASTRUCTURE) E.C.C.D.E.) 2017 FGN/UBE INTERVENTION PROJECTS LANDSCAPING AND EXTERNAL PACKAGE 1: WORKS Lot SCHOOL DESCRIPTION/ CONTRACT ID. NO. LOCATION DURATION No LOCATION Landscaping and External Works at PORT CP.S. O rom Ineke, PH, UPE MPS 1 RSUBEB/2017/ECCOE/CW/l/l HARCOURT& 12 WEEKS Borikiri, PH and S.P.S. III ENEKA, OBIO/AKPOR OBA LGA REHABILITATION OF 10 PACKAGE 2 CLASSROOM B LOCKS WITH BOREHOLE RSUBEB/2017/ 10-Classroom Blocks at Special 1 ECCDE/RC/2/1 School, for Handicapped KAA, KHANA 12 WEEKS KHANA RECONSTRUCTION OF 9 AND 12 PACKAGE 3 CLASSROOM BLOCKS RSUBEB/2017/ 4- Classroom Blocks at Special 1 E CCDE/RC/3/1 School for Handicapped Creek PHALGA 12 WEEKS Road, PHALGA CIVIL INFRASTRUCTURE (PRIMARY) 2017 FGN/UBE INTERVENTION PROJECTS COMPLETION OF 14 PACKAGE 1: CLASSROOM BLOCKS WITH TOILET AND BOREHOLE LOT SCHOOL CONTRACT ID. -
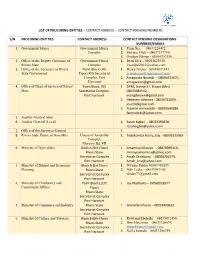
List of Procuring Entities – Contact Address – Contact Persons/Numbers
LIST OF PROCURING ENTITIES – CONTACT ADDRESS – CONTACT PERSONS/NUMBERS S/N PROCURING ENTITIES CONTACT ADDRESS CONTACT PERSONS-DESIGNATIONS- NUMBERS/EMAILS 1. Government House Government House 1. Perm Sec. – 08037224492 Complex 2. Margret Dick – 08037277770, 3. Oyoboy Edman - 08036757330 2. Office of the Deputy Governor of Government House 1. Iwari Jack – 08055625938, Rivers State Complex [email protected] 3. Office of the Secretary to Rivers Point Block (4th 1. Henry Nzeka – 08038831847, State Government Floor),R/S Secretariat [email protected] Complex, Port 2. Amagwula Nnamdi – 08064525671, Harcourt [email protected] 4. Office of Head of Service of Rivers Point Block, R/S 1 DPRS, Inyingi S.I. Brown (Mrs) - State Secretariat Complex, 08033384942, Port Harcourt [email protected] 2 Hekerem Adanma - 08036721069, [email protected] 3 Franklin Aminadoki – 08035640289 [email protected] 5. Auditor -General State 6. Auditor General (Local) 1. Sarah Kigbel - 08033393878 [email protected] 7. Office of the Surveyor-General 1. 8. Rivers State House of Assembly House of Assembly 1. Tubokomba Harry, Esq. - 08033125065 Complex Moscow Rd, PH 9. Ministry of Agriculture Block A (5th Floor) 1. Amamina Minaiyo - 08078969110, Rivers State [email protected] Secretariat Complex 2. Amah Christiana - 08036702579, Port Harcourt [email protected] 3. Ministry of Budget and Economic Block B (1st Floor) 1. Nwume Friday 08039382679 Planning Rivers State 2. Ndii Ledee - 08033097140 Secretariat Complex [email protected] Port Harcourt 4. Ministry of Chieftaincy and Point Block (11th 1. Joy Wariboko – 07068018977 Community Affairs Floor) Rivers State Secretariat Complex Port Harcourt 5. Ministry of Commerce and Industry Rivers State 1. Granville Elfreda – 08033409613 Secretariat Complex Port Harcourt 6. -

Preventing Election Violence in Rivers State
THE FUND FOR PEACE PARTNERSHIPS INITATIVE IN THE NIGER DELTA NIGER DELTA PARTNERSHIP INITIATIVE Time is of the Essence: Preventing Election Violence in Rivers State Special Issue Briefing: August 2018 Rivers recorded the highest number of reported insecurity specific to each senatorial district going fatalities within the Niger Delta in 2015 and was into 2019. sustained in 2016, with fatalities in the state finally decreasing in 2017. Rise of Political Violence in Rivers Prior to the 2011 election cycle, Rivers had few As gubernatorial candidates vie for control of reports of political violence. The Peoples Rivers in 2019, ongoing grievances within each of Democratic Party (PDP) was the only viable the state’s three senatorial districts -- Rivers South political party then and political competition was -East, Rivers West, and Rivers East -- will likely fuel relatively low. In the intervening years leading up violence. The senatorial zoning system has to the 2015 elections, support for the All increased perceptions of group marginalization Progressives Congress (APC) emerged, and it within certain communities, which could be a key became a somewhat viable opposition to the PDP Rivers State, Nigeria driver of election violence. in the state. A spike in political and election- Politics in the Niger Delta has often been related violence during the 2015 elections was the This report examines the senatorial zoning system characterized as high stakes issue and contest outcome of this opposition. in Rivers and outlines the challenges and drivers of between personalities as much as it is between their platforms. Election cycles in Rivers State have recently been marred by violence, especially Political Violence in Rivers State during gubernatorial and local contests. -

Evaluation of Spatial Distribution of Public Secondary Schools in Rivers State, Nigeria
Asian Research Journal of Arts & Social Sciences 8(4): 1-11, 2019; Article no.ARJASS.35801 ISSN: 2456-4761 Politics of School Mapping: Evaluation of Spatial Distribution of Public Secondary Schools in Rivers State, Nigeria Emmanuel C. Ibara1* 1Department of Educational Management, Ignatius Ajuru University of Education, P.M.B. 5047, Port Harcourt, Nigeria. Author’s contribution The sole author designed, analyzed and interpreted and prepared the manuscript. Article Information DOI: 10.9734/ARJASS/2019/v8i430111 Editor(s): (1) Dr. David Perez Jorge, Professor, Department of Teaching and Educational Research, University of La Laguna, Spain. Reviewers: (1) Almir Martins Vieira, Methodist University of São Paulo, Brazil. (2) Dr. H. L. Garbharran, Durban University of Technology, South Africa. (3) Kiongo Pius, Kenyatta University, Kenya. Complete Peer review History: http://www.sdiarticle3.com/review-history/35801 Received 28 October 2017 Accepted 19 January 2018 Original Research Article Published 02 April 2019 ABSTRACT School mapping in secondary education has witnessed a lot of distortion in Nigeria largely because the allocation of educational resources is embedded in politics of education. Consequently, the paper examined trends in the politics of school mapping and spatial distribution of secondary schools in Rivers state. Three research questions guided the study. The document analysis research method was utilized which involved extensive analysis of records and documents. Data collected were descriptively analysed. Findings revealed spatial imbalance in the distribution of public secondary schools, and neglect of population factor in siting secondary schools in Rivers State. Recommendations aimed at enhancing even distribution of public secondary schools were proffered. The paper concluded that school distribution system that ignores basic school mapping process could undermine the overall educational development in Rivers State. -

Impact of Agricultural Education on Agricultural Productivity of Women Farmers in Omuma Local Government Area of Rivers State
International Journal of Innovative Psychology & Social Development 7(2):83-90, April-June, 2019 © SEAHI PUBLICATIONS, 2019 www.seahipaj.org ISSN: 2467-8546 Impact of Agricultural Education on Agricultural Productivity of Women Farmers in Omuma Local Government Area of Rivers State 1Nlebem, Bernard S. (Ph.D) & 2Okagwa Promise Omoruka 1Department of Vocational and Technology Education Faculty of Education Rivers State University Nkpolu-Oroworukwo, Port Harcourt, Nigeria [email protected]; Phone; 08036699137 2Department of Vocational and Technical Education Faculty of Education Rivers State University: Nkpolu-Oroworukwo Port-Harcourt, Nigeria [email protected] ABSTRACT The study investigated the impacts of agricultural education on agricultural productivity of educated and non-educated women farmers in Omuma Local Government Area of Rivers State. Taro Yemene formula were used to select a sample size of 850 out of 4890 registered educated and non-educated women farmers used as population from the ten wards in Omuma. Data was collected by the use of an instrument titled „Agricultural Productivity of Women Farmers Questionnaire” (APWFQ). 850 copies of the instrument were administered on the respondents out of which 800 copies were completed and returned. Data was analyzed using mean and standard deviation for the research questions and the hypotheses was tested using Z-test at 0.05 level of significance. Questionnaire was face validated by three experts, and the reliability was tested using Cronbach‟s alpha reliability estimate to determine the internal consistency of the questionnaire; this yielded a reliability coefficient (r) of 0.877. The findings revealed that timely application of pesticides to reduce pest attack and increase yield was rejected by both the educated and non-educated women farmers. -

Petro-Violence and the Geography of Conflict in Nigeria's
Spaces of Insurgency: Petro-Violence and the Geography of Conflict in Nigeria’s Niger Delta By Elias Edise Courson A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Geography in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Michael J. Watts, Chair Professor Ugo G. Nwokeji Professor Jake G. Kosek Spring 2016 Spaces of Insurgency: Petro-Violence and the Geography of Conflict in Nigeria’s Niger Delta © 2016 Elias Edise Courson Abstract Spaces of Insurgency: Petro-Violence and the Geography of Conflict in Nigeria’s Niger Delta by Elias Edise Courson Doctor of Philosophy in Geography University of California, Berkeley Professor Michael J. Watts, Chair This work challenges the widely held controversial “greed and grievance” (resource curse) narrative by drawing critical insights about conflicts in the Niger Delta. The Niger Delta region of Nigeria has attracted substantial scholarly attention in view of the paradox of poverty and violence amidst abundant natural resources. This discourse suggests that persistent resource- induced conflicts in the region derive from either greed or grievance. Instead, the present work draws inspiration from the political geography of the Niger Delta, and puts the physical area at the center of its analysis. The understanding that the past and present history of a people is etched in their socio-political geography inspires this focus. Whereas existing literatures engages with the Niger Delta as a monolithic domain, my study takes a more nuanced approach, which recognizes a multiplicity of layers mostly defined by socio-geographical peculiarities of different parts of the region and specificity of conflicts its people experience.