Gastrointestinal Motility Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pathophysiology and Management of Diabetic Gastroenteropathy
Pathophysiology and management of diabetic gastroenteropathy Meldgaard, Theresa; Keller, Jutta; Olesen, Anne Estrup; Olesen, Søren Schou; Krogh, Klaus; Borre, Mette; Farmer, Adam; Brock, Birgitte; Brock, Christina; Drewes, Asbjørn Mohr Published in: Therapeutic Advances in Gastroenterology DOI: 10.1177/1756284819852047 Publication date: 2019 Document version Publisher's PDF, also known as Version of record Document license: CC BY-NC Citation for published version (APA): Meldgaard, T., Keller, J., Olesen, A. E., Olesen, S. S., Krogh, K., Borre, M., Farmer, A., Brock, B., Brock, C., & Drewes, A. M. (2019). Pathophysiology and management of diabetic gastroenteropathy. Therapeutic Advances in Gastroenterology, 12, 1-17. https://doi.org/10.1177/1756284819852047 Download date: 01. Oct. 2021 TAG0010.1177/1756284819852047Therapeutic Advances in GastroenterologyT Meldgaard, J Keller 852047review-article20192019 Therapeutic Advances in Gastroenterology Review Ther Adv Gastroenterol Pathophysiology and management of 2019, Vol. 12: 1–17 DOI:https://doi.org/10.1177/1756284819852047 10.1177/ diabetic gastroenteropathy 1756284819852047https://doi.org/10.1177/1756284819852047 © The Author(s), 2019. Article reuse guidelines: Theresa Meldgaard, Jutta Keller, Anne Estrup Olesen, Søren Schou Olesen, Klaus Krogh, sagepub.com/journals- Mette Borre, Adam Farmer, Birgitte Brock, Christina Brock and Asbjørn Mohr Drewes permissions Abstract: Polyneuropathy is a common complication to diabetes. Neuropathies within the Correspondence to: Theresa Meldgaard enteric nervous system are associated with gastroenteropathy and marked symptoms that Mech-Sense, Department of Gastroenterology and severely reduce quality of life. Symptoms are pleomorphic but include nausea, vomiting, Hepatology, Aalborg dysphagia, dyspepsia, pain, bloating, diarrhoea, constipation and faecal incontinence. The University Hospital, aims of this review are fourfold. First, to provide a summary of the pathophysiology underlying Denmark Department of Clinical diabetic gastroenteropathy. -

Total Pancreatectomy for Chronic Pancreatitis
Gut: first published as 10.1136/gut.29.3.358 on 1 March 1988. Downloaded from Gut, 1988, 29, 358-365 Total pancreatectomy for chronic pancreatitis I P LINEHAN, M A LAMBERT, D C BROWN, A B KURTZ, P B COTTON, AND R C G RUSSELL From the Departments ofSurgery, Gastroenterology and Medicine, The Middlesex Hospital and Medical School, London SUMMARY The operation oftotal pancreatectomy is performed rarely. Its role in the management of patients with chronic pancreatitis remains to be elucidated. We have reviewed our series of 29 total pancreatectomies for benign disease [14 women median age 39 years; 15 men median age 34 years]. Twelve underwent standard total pancreatectomy, in 17 duodenum preserving total pancreatectomy (DPTP) was performed. There was one death (mortality 3.4%). In no patient was the total pancreatectomy the first operative procedure. The patients were compared with age and sex matched diabetic control subjects selected on a best fit basis from the diabetic clinic database. The aetliology of the pancreatitis was idiopathic nine, pancreas divisum nine, alcohol eight and other causes three. The indication for surgery was pain 27, acute pancreatitis one and cholangitis with pancreatitis one. The complications ofthe procedures were mainly caused by infection [wound three, chest six and central line sepsis four] and in two there was a leak from the duodenum; no patient required re-operation. The postoperative stay [standard total, median 21 days (range 13-98) DPTP median 31 days (range 17-49)] has lengthened over the period due to greater attention to analgesic, diabetic and enzyme deficiency control before discharge. -

Fluoroscopic Characterization of Colonic Dysmotility Associated to Opioid and Cannabinoid Agonists in Conscious Rats
J Neurogastroenterol Motil, Vol. 25 No. 2 April, 2019 pISSN: 2093-0879 eISSN: 2093-0887 https://doi.org/10.5056/jnm18202 JNM Journal of Neurogastroenterology and Motility Original Article Fluoroscopic Characterization of Colonic Dysmotility Associated to Opioid and Cannabinoid Agonists in Conscious Rats Susana Díaz-Ruano,1 Ana E López-Pérez,1,5 Rocío Girón,2,3,4,5 Irene Pérez-García,2 María I Martín-Fontelles,2,3,4,5 and Raquel Abalo2,3,4,5* 1Unidad de Dolor, Servicio de Anestesiología, Hospital General Universitario Gregorio Marañón, Madrid, Spain; 2Departamento de Ciencias Básicas de la Salud, Facultad de Ciencias de la Salud, Universidad Rey Juan Carlos, Alcorcón, Madrid, Spain; 3Unidad Asociada I+D+i al Instituto de Investigación en Ciencias de la Alimentación, CIAL (CSIC), Madrid, Spain; 4Unidad Asociada I+D+i al Instituto de Química Médica, IQM (CSIC), Madrid, Spain; and 5Grupo de Excelencia Investigadora URJC-Banco de Santander-Grupo Multidisciplinar de Investigación y Tratamiento del Dolor (i+DOL), Madrid, Spain Background/Aims Gastrointestinal adverse effects have a major impact on health and quality of life in analgesics users. Non-invasive methods to study gastrointestinal motility are of high interest. Fluoroscopy has been previously used to study gastrointestinal motility in small experimental animals, but they were generally anesthetized and anesthesia itself may alter motility. In this study, our aim is to determine, in conscious rats, the effect of increasing doses of 2 opioid (morphine and loperamide) and 1 cannabinoid (WIN 55,212-2) agonists on colonic motility using fluoroscopic recordings and spatio-temporal maps. Methods Male Wistar rats received barium sulfate intragastrically, 20-22 hours before fluoroscopy, so that stained fecal pellets could be seen at the time of recording. -

Gastroparesis and Dumping Syndrome: Current Concepts and Management
Journal of Clinical Medicine Review Gastroparesis and Dumping Syndrome: Current Concepts and Management Stephan R. Vavricka 1,2,* and Thomas Greuter 2 1 Center of Gastroenterology and Hepatology, CH-8048 Zurich, Switzerland 2 Department of Gastroenterology and Hepatology, University Hospital Zurich, CH-8091 Zurich, Switzerland * Correspondence: [email protected] Received: 21 June 2019; Accepted: 23 July 2019; Published: 29 July 2019 Abstract: Gastroparesis and dumping syndrome both evolve from a disturbed gastric emptying mechanism. Although gastroparesis results from delayed gastric emptying and dumping syndrome from accelerated emptying of the stomach, the two entities share several similarities among which are an underestimated prevalence, considerable impairment of quality of life, the need for a multidisciplinary team setting, and a step-up treatment approach. In the following review, we will present an overview of the most important clinical aspects of gastroparesis and dumping syndrome including epidemiology, pathophysiology, presentation, and diagnostics. Finally, we highlight promising therapeutic options that might be available in the future. Keywords: gastroparesis; dumping syndrome; pathophysiology; clinical presentation; treatment 1. Introduction Gastroparesis and dumping syndrome both evolve from a disturbed gastric emptying mechanism. While gastroparesis results from significantly delayed gastric emptying, dumping syndrome is a consequence of increased flux of food into the small bowel [1,2]. The two entities share several important similarities: (i) gastroparesis and dumping syndrome are frequent, but also frequently overlooked; (ii) they affect patient’s quality of life considerably due to possibly debilitating symptoms; (iii) patients should be taken care of within a multidisciplinary team setting; and (iv) treatment should follow a step-up approach from dietary modifications and patient education to pharmacological interventions and, finally, surgical procedures and/or enteral feeding. -

Akt Phosphorylation of Neuronal Nitric Oxide Synthase Regulates Gastrointestinal Motility in Mouse Ileum
Akt phosphorylation of neuronal nitric oxide synthase regulates gastrointestinal motility in mouse ileum Damian D. Guerraa, Rachael Boka, Vibhuti Vyasa, David J. Orlickyb, Ramón A. Lorcaa, and K. Joseph Hurta,c,1 aDivision of Reproductive Sciences, Department of Obstetrics and Gynecology, University of Colorado Anschutz Medical Campus, Aurora, CO 80045; bDepartment of Pathology, University of Colorado Anschutz Medical Campus, Aurora, CO 80045; and cDivision of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, University of Colorado Anschutz Medical Campus, Aurora, CO 80045 Edited by Solomon H. Snyder, Johns Hopkins University School of Medicine, Baltimore, MD, and approved July 15, 2019 (received for review April 5, 2019) Nitric oxide (NO) is a major inhibitory neurotransmitter that mediates receptor activation (18–20). Some evidence suggests that phosphor- nonadrenergic noncholinergic (NANC) signaling. Neuronal NO syn- ylation of the equivalent Akt/PKA consensus site in nNOS, ser- + thase (nNOS) is activated by Ca2 /calmodulin to produce NO, which ine1412 (S1412), also stimulates neuronal NO synthesis (21). Because + causes smooth muscle relaxation to regulate physiologic tone. nNOS nNOS activity is more sensitive to [Ca2 ](21),andnNOSismore serine1412 (S1412) phosphorylation may reduce the activating rapidly dephosphorylated than eNOS (22), it is technically difficult to 2+ Ca requirement and sustain NO production. We developed and evaluate nNOS S1412 phosphorylation in vivo. Nonetheless, studies S1412A characterized a nonphosphorylatable nNOS knock-in mouse implicate nNOS S1412 phosphorylation in hippocampal excitotoxicity and evaluated its enteric neurotransmission and gastrointestinal (4), penile erection (22), and luteinizing hormone release (23). (GI) motility to understand the physiologic significance of nNOS Enteric neurons express high levels of nNOS, Akt, and PKA S1412 phosphorylation. -
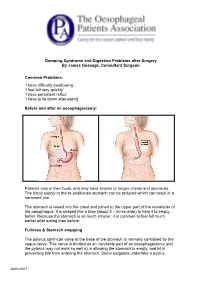
Dumping Syndrome and Digestion Problems After Surgery by James Gossage, Consultant Surgeon Common Problems: 'I Have Difficulty
Dumping Syndrome and Digestion Problems after Surgery By James Gossage, Consultant Surgeon Common Problems: ‘I have difficulty swallowing’. ‘I feel full very quickly’ ‘I have persistent reflux’ ‘I have to lie down after eating’ Before and after an oesophagectomy: Patients vary in their build, and may have shorter or longer chests and stomachs. The blood supply to the re-positioned stomach can be reduced which can result in a narrowed join. The stomach is raised into the chest and joined to the upper part of the remainder of the oesophagus. It is shaped like a tube (about 5 – 6cms wide) to help it to empty better. Because the stomach is so much smaller, it is common to feel full much earlier after eating than before. Fullness & Stomach emptying The pylorus sphincter valve at the base of the stomach is normally controlled by the vagus nerve. This nerve is divided as an inevitable part of an oesophagectomy and the pylorus may not work so well a) in allowing the stomach to empty, and b) in preventing bile from entering the stomach. Some surgeons undertake a pyloric 26/01/2017 myotomy (cutting the muscles to increase its capacity) as part of the main surgery; others prefer to wait and see if a problem develops, and then treat it by stretching it with an endoscope. Difficulty in Swallowing: Difficulty in Swallowing Narrow join Acid reflux leading to inflammation Fungal infection (candidiasis) Treatment options can be: Endoscopic dilation – acid suppression – sucralfate (binds the stomach) – antifungals Motility agents (domperidone, metoclopramide (good anti-sickness medication but needs 6 weeks to be fully effective; erythromycin). -

Ocreotide and Its Effects on Steroid Resistant Crohn's Disease
2ND YEAR RESEARCH ELECTIVE RESIDENT’S JOURNAL Volume III, 1998-1999 Octreotide and its effects on Steroid resistant Crohn’s Disease Bonnie Wolf A. Introduction The treatment of Crohn’s disease continues to be a challenge as its pathogenesis remains obscure. Compounded by the increased incidence of Crohn's disease in the past twenty years incidence of 5/100,000, prevalence of 50/100,000), we are faced with an ever increasing number of treatment failures. The pathogenesis of inflammatory bowel disease stems from a dysregulation of the immune system, with persistent amplification of inflammatory cytokines, ultimately leading to tissue destruction and disease. Conventional treatment continues to be sulphasalazine or 5-ASA and glucocorticoids. For early disease and maintenance therapy, these medications have proven to be satisfactory and widely tolerated. Yet by the nature of this disease, patients relapse. They require increasing doses of medications thereby becoming resistant and simultaneously developing side effects. Sulphasalazine was shown to be more effective than placebo in controlling active disease, but was not as efficacious as steroids (2,3). In addition, not all patients can tolerate 5-ASA secondary to mild side effects including diarrhea, dizziness, nausea, and headache. Glucocorticoids are still considered to be very effective and are the most popular prescribed medications for acute active disease. The National Cooperative Crohn’s Disease Study showed that 47% of patients achieved remission and 60% improvement under therapy with varying doses of prednisilone. (2) Despite it effectiveness, glucocorticoids have a wide and significant side effect profile, and are considered unsafe to be used with frequent exacerbations and moreover as maintenance therapy.(1) Most recently, immunosuppressive agents such as azathioprine (Imuran) and Purinethanol (6- mercaptopurine.) have been introduced as potential therapies for patients who have chronic active disease or who are steroid dependent. -

Post-Whipple: a Practical Approach to Nutrition Management
NINFLAMMATORYUTRITION ISSUES BOWEL IN GASTROENTEROLO DISEASE: A PRACTICALGY, SERIES APPROACH, #108 SERIES #73 Carol Rees Parrish, M.S., R.D., Series Editor Post-Whipple: A Practical Approach to Nutrition Management Nora Decher Amy Berry The classic pancreatoduodenectomy (PD), also known as the Kausch-Whipple, and the pylorus- preserving pancreatoduodenectomy (PPPD) are most commonly performed for treatment of pancreatic cancer and chronic pancreatitis. This highly complex surgery disrupts the coordination of tightly orchestrated digestive processes. This, in combination with a diseased gland, sets the patient up for nutritional complications such as altered motility (gastroparesis and dumping), pancreatic insufficiency, diabetes mellitus, nutritional deficiencies and bacterial overgrowth. Close monitoring and attention to these issues will help the clinician optimize nutritional status and help prevent potentially devastating complications. 63-year-old female, D.D., presented to the copper, zinc, selenium, and potentially thiamine University of Virginia Health System (UVAHS) (thiamine was repleted before serum levels were Awith weight loss and biliary obstruction. She was checked). A percutaneous endoscopic gastrostomy with diagnosed with a large pancreatic serous cystadenoma jejunal extension (PEG-J) was placed due to intolerance and underwent a pancreatoduodenectomy (PD) of gastric enteral nutrition (EN). After several more (standard Whipple procedure with partial gastrectomy) hospitalizations, prolonged rehabilitation in a nursing with posterior anastomosis and cholecystectomy. Seven home, 7 months of supplemental nocturnal EN, and months later she was admitted to UVAHS with nausea, treatment of pancreatic insufficiency with pancreatic vomiting, diarrhea and a severe weight loss of 47lbs enzymes (with her meals and EN), D.D. was able to (33% of her usual body weight). -

The Plasmapheresis in the Treatment of Guillain-Barré Syndrome
Merit Research Journal of Medicine and Medical Sciences (ISSN: 2354-323X) Vol. 7(2) pp. 066-072, February, 2019 Available online http ://www.meritresearchjournals.org/mms/index.htm Copyright © 2019 Merit Research Journals Case Report The Plasmapheresis in the Treatment of Guillain-Barre ́ Syndrome Associated with Primary Enteric Neuropathy, Case Report. Up-Date Data from Literature Lungu Mihaela 1* and Sapira Violeta 2 Abstract 1Assoc. Prof., Head of Neurological The article presents a case with a particular clinical situation that has Department, Emergency Clinical associated an enteric neuropathy with an evolution of over two months, with Hospital Galati, Romania; Faculty of a Guillain-Barré syndrome (Landry type), both remitted after Medicine and Pharmacy, “Dunarea de plasmapheresis. A 53 year old male patient has been admitted in our Jos” University of Galati, Romania Neurological Department with dehydration, syncope and orthostatic 2Assist. Prof., Neurological hypotention, due to an enteric neuropathie, complicated in 8 days with a Department, Emergency Clinical Guillain Barré syndrome-GBS. This type of associated diseases is rarely Hospital Galati, Romania; Faculty of described in the literature, being well known that GBS can be precede with Medicine and Pharmacy, “Dunarea de two weeks in advance by a diarrheic episode. In our case, a chronic Jos” University of Galati, Romania diarrheic sufferance was involved- an enteric neuropathy. Both types of neurological manifestations had an obvious improvement after *Corresponding Author’s -
Chronic Intestinal Pseudo-Obstruction As an Expression Of
GE Port J Gastroenterol. 2014;21(6):254---257 www.elsevier.pt/ge CLINICAL CASE Chronic intestinal pseudo-obstruction as an expression of inflammatory enteric neuropathy a,∗ a a b a Rita Pimentel , Marta Salgado , Maria João Magalhães , Ana Accarino , Isabel Pedroto a Gastroenterology Department, Centro Hospitalar do Porto, Hospital de Santo António, Porto, Portugal b Gastroenterology Department, Hospital Universitari Vall d’Hebron, Barcelona, Spain Received 22 December 2013; accepted 28 July 2014 Available online 22 November 2014 KEYWORDS Abstract Chronic intestinal pseudo-obstruction (CIPO) is characterised by inadequate diges- tive tract motility and can lead to severely disordered motility. CIPO manifests as recurrent Chronic intestinal pseudo-obstruction; episodes of intestinal sub-occlusion without an anatomical obstruction. We present the case Neuropathy; of a 41-year-old female, with severe chronic constipation and several episodes of intesti- Bowel nal sub-occlusion. Investigation revealed colonic inertia and marked distension of the small bowel and colon with no evidence of stenosis or obstructive lesions, compatible with CIPO. After several treatments were tried (domperidone, erythromycin, cisapride, octreotide, total enteral nutrition), with partial or no response, further work-up was done trying to identify an etiology. Gastrointestinal manometry showed neuropathic type abnormalities, transmural biopsy of the jejunum revealed degenerative enteric neuropathy and anti-HU antineuronal antibody screen was positive, suggesting an autoimmune type neuropathy with diffuse involve- ment of the digestive tract. Corticosteroids showed partial improvement of short duration and azathioprine was also tried but discontinued due to intolerance. Marked dietary intolerance and malnutrition lead to total parenteral nutrition (TPN) at home since October 2011. -

Dumping Syndrome Diet
4 The Dumping Syndrome Diet What foods can I eat after stomach surgery? Foods in the “Recommended” list are usually well tolerated after stomach surgery. Remember to drink unsweetened liquids 30 to 60 minutes after eating solid foods. Type of Food Recommended Avoid Milk and milk Milk, plain yogurt, artificially Sweetened milk, chocolate milk, The Dumping Syndrome Diet products sweetened yogurt, cottage milkshakes, sweetened condensed cheese, cream cheese, sugar free milk; ice cream, puddings, custard, pudding, cheese, cream soups fruit flavoured yogurt, frozen yogurt After a stomach resection, you may feel sick when you finish your meal. Breads and Whole wheat breads, whole wheat Cereals with a sugar coating, granola, You will need to make some changes to your diet while your body heals cereals pasta, unsweetened cereals, sweet breads, rolls, cakes, cookies, after surgery. potatoes, rice, crackers, pretzels sweet baked goods, pancakes and Esophagus waffles with syrup, doughnuts Meats and Meat, poultry, fish, eggs, lunch Casseroles and dishes prepared with Bile Duct alternatives meat, tofu, peanut butter, nuts, sweet sauces legumes Fruits and Fruits – fresh fruit, unsweetened Canned fruit in syrup, sweetened fruit Duodenum Stomach vegetables canned or frozen fruit, juice, dried fruit Jejunum unsweetened fruit juice Vegetables cooked in sweet sauces Vegetables – all types Fats and oils Butter, margarine, oil, salad None Bile dressings Beverages All unsweetened drinks such as Sweetened drinks like Kool-aid, (limit to 4 oz Crystal Light, water, -

The British Society of Gastroenterology
Gut: first published as 10.1136/gut.12.10.853 on 1 October 1971. Downloaded from Gut, 1971, 12, 853-870 The British Society of Gastroenterology The 32nd annual general meeting of the British Society of Gastroenterology was held at Newcastle upon Tyne from 23 to 25 September 1971 under the Presidency of Professor A. A. Harper. The programme included the abstracts that follow and in addition symposia on 'Aetiology and epidemiology of carcinoma of the colon and rectum' and 'Ischaemic colitis', and a progress re- port by Professor E. L. Blair on 'Measurement of gastrointestinal hormones'. A report on the business ofthe meeting is printed on page 871. Gastroenterostomy-An Obsolete Operation? Preparation and Characterization of Lateral and Basal Plasma Membranes of the Rat Enterocyte W. P. SMALL, C. W. A. FALCONER, A. N. SMITH, J. P. A, MCMANUS, AND W. SIRCUS (Gastro-Intestinal Unit, A. P. DOUGLAS, R. KERLEY, R. CORNELL, AND K. J. Western General Hospital, Edinburgh) Gastro- ISSELBACHER (Royal Postgraduate Medical School. enterostomy fell from favour once its association University of London, London, W.12, and Massa- with a high incidence of jejunal ulceration became chusetts General Hospital, Boston, USA) Ana- recognized. It has never regained popularity, tomical and physiological studies suggest there is a although some surgeons have recommended its distinct polarity in the enterocyte. These considera- further trial (Tanner, 1969) and although surgeons tions suggest there may well be differences between who could look back to the heyday of gastroentero- the plasma membrane (PM) of the brush border and stomy claimed that, when uncomplicated by jejunal that of the lateral and basal boundaries of the cell.