Evaluating the Oral Health Knowledge and the Status of Visually Impaired Children Using Braille 1Anand Tavargeri, 2Sapna S Kudtarkar
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HŒ臬 A„簧綟糜恥sµ, Vw笑n® 22.12.2019 Š U拳 W
||Om Shri Manjunathaya Namah || Shri Kshethra Dhamasthala Rural Development Project B.C. Trust ® Head Office Dharmasthala HŒ¯å A„®ãtÁS®¢Sµ, vw¯ºN® 22.12.2019 Š®0u®± w®lµu® îµ±°ªæX¯Š®N®/ N®Zµ°‹ š®œ¯‡®±N®/w®S®u®± š®œ¯‡®±N® œ®±uµÛ‡®± wµ°Š® wµ°î®±N¯r‡®± ªRq® y®‹°£µ‡®± y®ªq¯ºý® D Nµ¡®w®ºruµ. Cu®Š®ªå 50 î®±q®±Ù 50 Oʺq® œµX®±Ï AºN® y®lµu®î®Š®w®±Ý (¬šµ¶g¬w®ªå r¢›Š®±î®ºqµ N®Zµ°‹/w®S®u®± š®œ¯‡®±N® œ®±uµÛSµ N®xÇ®Õ ïu¯ãœ®Áqµ y®u®ï î®±q®±Ù ®±š®±é 01.12.2019 NµÊ Aw®æ‡®±î¯S®±î®ºqµ 25 î®Ç®Á ï±°Š®u®ºqµ î®±q®±Ù îµ±ªæX¯Š®N® œ®±uµÛSµ N®xÇ®Õ Hš¬.Hš¬.HŒ¬.› /z.‡®±±.› ïu¯ãœ®Áqµ‡µ²ºvSµ 3 î®Ç®Áu® Nµ©š®u® Aw®±„Â®î® î®±q®±Ù ®±š®±é 01.12.2019 NµÊ Aw®æ‡®±î¯S®±î®ºqµ 30 î®Ç®Á ï±°Š®u®ºqµ ) î®±±ºvw® œ®ºq®u® š®ºu®ý®Áw®NµÊ B‡µ±Ê ¯l®Œ¯S®±î®¼u®±. š®ºu®ý®Áw®u® š®Ú¡® î®±q®±Ù vw¯ºN®î®w®±Ý y®äqµã°N®î¯T Hš¬.Hº.Hš¬ î®±²©N® ¯Ÿr x°l®Œ¯S®±î®¼u®±. œ¯cŠ¯u® HŒ¯å A„®ãtÁS®¢Sµ A†Ãw®ºu®wµS®¡®±. Written test Sl No Name Address Taluk District mark Exam Centre out off 100 11 th ward near police station 1 A Ashwini Hospete Bellary 33 Bellary kampli 2 Abbana Durugappa Nanyapura HB hally Bellary 53 Bellary 'Sri Devi Krupa ' B.S.N.L 2nd 3 Abha Shrutee stage, Near RTO, Satyamangala, Hassan Hassan 42 Hassan Hassan. -

Secret Ballot Election 2020- Final Voter List
SOUTH WESTERN RAILWAY HUBBALLI DIVISION FINAL VOTER LIST Booth Sl. No Name Post/ Designation PF.No./ NPS Working Under STN Remarks Sl. No. 1 1 VIJAY RAMESH CHUTAKE CCC 424N0750361 COMMERCIAL RBG 1.KUD 2 2 PRIYANKA.V.DESAI CCC 424N0950168 COMMERCIAL KUD 1.KUD 3 3 NIRMALA PUNDALEEK VADEYAR COML.CLERK 424N1150049 COMMERCIAL UGR 1.KUD 4 4 NAZIR AHAMED H AZARATH KHAN COML.CLERK 424N1250118 COMMERCIAL CNC 1.KUD 5 5 SHASHI SHEKAR KUMAR COML.CLERK 424N1550300 COMMERCIAL KUD 1.KUD 6 6 RAVI KUMAR SINGH COML.CLERK 424N1550302 COMMERCIAL KUD 1.KUD 7 7 MOHAN KUMAR COML.CLERK 424N1550304 COMMERCIAL GPB 1.KUD 8 8 GOPESH KUMAR MEENA Sr.COML.CLERK TR350510066 COMMERCIAL RBG 1.KUD 9 9 G DATTATRAYA CCC 42407271268 COMMERCIAL GPB 1.KUD 10 10 K DANAM PAUL CCC 42407286417 COMMERCIAL GPB 1.KUD 11 11 SAHADEV BELAGALI Sr.COML.CLERK 15215MAS235 COMMERCIAL RBG 1.KUD 12 12 BHIMAPPA MEDAR CCC 42429802590 COMMERCIAL KUD 1.KUD 13 13 ANTHONY MARVEL AUGUSTINE COML.CLERK 42429804093 COMMERCIAL UGR 1.KUD 14 14 AMAR M BADODE CCC 42529801575 COMMERCIAL UGR 1.KUD 15 15 DUNDESH AGASAGI PORTER(COML) 42429805008 COMMERCIAL GPB 1.KUD 16 16 LAKSHMAN PANDIT KAMBLE SR.TE 424N1250686 COMMERCIAL GPB 1.KUD 17 17 HUKAM LAL MEENA SR.TE 424N1251254 COMMERCIAL GPB 1.KUD 18 18 DEEPAK SAMAPT TRACKMAN 00302666479 ENGINEERING VJR 1.KUD 19 19 NINGAPPA VITHAL TRACK MNTR-III 00606456686 ENGINEERING KUD 1.KUD 20 20 YEMANAPA LAGAMAPA TRACK MNTR-III 42406427157 ENGINEERING GPB 1.KUD 21 21 BHEEMAPPA BALAPPA TRACK MNTR-II 42406430235 ENGINEERING KUD 1.KUD 22 22 SRINIVAS NAGARHALI TRACK MNTR-II 42406432554 -

District Census Handbook, Dharwad, Part XII-A, Series-11
CENSUS OF INDIA 1991 Series -11 KARNATAKA DISTRICT CENSUS HANDBOOK DHAR\VAD DISTRICT PART XII-A "IU.AGE ANHTOWN DIRELJORY SOBIIA NAMBISAN DH-ector of Census Operations, Kurnataka CONTENTS Page No. FOREWORD vii-viii PREFACE lX-X IMPORTANT STATISTICS ANALYTICAL NOTE Section-I - VHl&lge DiI'cctm'Y Explanatory Notc Alphabelical List of Villages - Bpdgi C.O.Blm:k Village Directory Statemcnt - B).tdgi C.D.Blud. Alphabetical List of Villages - Dhafwad CoD. Rlock Village Dircctory Statemcnt - Dharwad C.D.Block Alphahctical Liht of Villagch - (jadag C.O.BlI)(:k Village Directory Statement - Gadag CD.Block ()X- 105 Alphabetical Lihl of Villages - Hallgal C.D.Bhld: )1)1)- I 12 Village Directory Statement - Hangal CD.Block 11-1-1-11 Alphabetical Liht of Villages - Ha .... eri C.D.Block 145-147 Village Directory Stah:mcnl - 11a\L~ri C.D.Blod. 1-1X- J(,.1 Alphabetical Lihl of Vilbgl.: .... - } lirdcr lit' C.D.Block 1(,7-170 Village Directory Slal<.:m..:nl - I-lird. ..:rur C.D.BhK'1-.. 11'2-1:-;1) Alphabetical List of Villageh - lillbli C.D.BhlCk 1'J.1-194 ViI1age Directory Slat<.:ment - Hubli C.D.Block 1')(>-205 Alphabetical Liht of Villages - Kalg:h;tlgi C.D.Block 2()')- 21 I Village Dircctory Statcment - K4Ilghatgi CO.Block 212-225 Alphabclit'al List of Villages - K lInd;I~()1 CD.Block 22()-23() Village Directory Stat<.:ml'nt - Kundagul C.D.Block Alphabetical List of Villageh - MlInd,lrgi CD.B1o,:h Village Directory Statcl1ll:nt - l\lulllbrgi CO.Blnd P"g_L' l'< ll. Alphahctical Li~t 01" Villages - N :1I·g.und C [). -

Dist Name Taluk Name GP Name New Accoun No Bank Name
ANNEXURE Releases to Dharwar Dist Dist_name taluk_name GP_name New Accoun no Bank_name Branch name IFSC code rel_amount Dharwar Dharwad Arwatagi 5743 Karnataka Vikasa Grameena Bank (KVGB) ARWATAGI 1.00 Dharwar Dharwad Belur 135001010006162 Vijaya Bank KOTUR VIJD0001350 1.00 Dharwar Dharwad Benachi 5741 Karnataka Vikasa Grameena Bank (KVGB) ARWATAGI 2.00 Dharwar Dharwad Devarhubbali 9726 Karnataka Vikasa Grameena Bank (KVGB) NIGADI 3.00 Dharwar Dharwad Garag 11194 Indian Overseas Bank (IOB) GARAG IOBA0000308 1.00 Dharwar Dharwad Halligeri 9722 Karnataka Vikasa Grameena Bank (KVGB) NIGADI 2.00 Dharwar Dharwad Hangarki 11195 Indian Overseas Bank (IOB) GARAG IOBA0000308 2.00 Dharwar Dharwad Hebballi 841710100008076 Bank of India (BOI) HEBBALLI BKID0008417 5.00 Dharwar Dharwad Honnapur 5746 Karnataka Vikasa Grameena Bank (KVGB) ARWATAGI 5.00 Dharwar Dharwad Kalakeri 7347 Karnataka Vikasa Grameena Bank (KVGB) MUGAD 3.00 Dharwar Dharwad Kanakur 5572 Karnataka Vikasa Grameena Bank (KVGB) SHIVALLI 2.00 Dharwar Dharwad Kotabagi 11211 Indian Overseas Bank (IOB) GARAG IOBA0000308 2.00 Dharwar Dharwad Kotur 135001010006183 Vijaya Bank KOTUR VIJD0001350 3.00 Dharwar Dharwad Lokur 1692 Karnataka Vikasa Grameena Bank (KVGB) UPPIN BETAGERI 3.00 Dharwar Dharwad Madhanbhavi 8655 Karnataka Vikasa Grameena Bank (KVGB) TADAKOD 3.00 Dharwar Dharwad Managundi 137201010004389 Vijaya Bank HOSAYAL NAGAR DHARWAD VIJB0001372 3.00 Dharwar Dharwad Mandihal 7317 Karnataka Vikasa Grameena Bank (KVGB) MUGAD 4.00 Dharwar Dharwad Maradagi 5561 Karnataka Vikasa Grameena -

Responsible for Plague in Bombay Province, Though They Have Been
Bull. Org. mond. Sante Bull. World Hlth Org.J 1951, 4, 75-109 SPREAD OF PLAGUE IN THE SOUTHERN AND CENTRAL DIVISIONS OF BOMBAY PROVINCE AND PLAGUE ENDEMIC CENTRES IN THE INDO-PAKISTAN SUBCONTINENT a M. SHARIF, D.Sc., Ph.D., F.N.I. Formerly Assistant Director in Charge of Department of Entomology, Haffkine Institute, Bombay b Manuscript received in September 1949 The findings of the Plague Recrudescence Inquiry in Sholapur and Adjoining Districts, conducted by Sharif & Narasimham11 12 in the districts of Sholapur and Dharwar during 1940 to 1943, do not support the idea that wild rodents help to carry plague infection from one place to another as in " temperate climes ".4 Wild rodents cannot be considered responsible for plague in Bombay Province, though they have been shown to be so in Transbaikalia, Mongolia, South-Eastern Russia, South Africa, and the western parts of the USA.17 In Bombay Province, the domestic rat perpetuates the plague infection. In some suitable places the infection among domestic rats goes on throughout the year. The infection is not apparent during the hot and dry season, its intensity being diminished because of the ill effect of prevailing climatic conditions on the wanderings of adult rat-fleas ; it pursues the course of a slow subterranean enzootic from burrow to burrow. The conclusion of the off-season is characterized by the advent of the rainy season, which exerts its influence in two ways first, it causes the rats from outside shelters to herd into burrows indoors and remain there perforce, which results in a considerable increase in the rat population within houses; secondly, it brings down the temperature and increases the humidity to such an extent as to result in a striking rise in the flea population and to allow rat-fleas to come out of burrows to attack human beings. -

Gram Panchayat Human Development
Gram Panchayat Human Development Index Ranking in the State - Districtwise Rank Rank Rank Standard Rank in in Health in Education in District Taluk Gram Panchayat of Living HDI the the Index the Index the Index State State State State Bagalkot Badami Kotikal 0.1537 2186 0.7905 5744 0.7164 1148 0.4432 2829 Bagalkot Badami Jalihal 0.1381 2807 1.0000 1 0.6287 4042 0.4428 2844 Bagalkot Badami Cholachagud 0.1216 3539 1.0000 1 0.6636 2995 0.4322 3211 Bagalkot Badami Nandikeshwar 0.1186 3666 0.9255 4748 0.7163 1149 0.4284 3319 Bagalkot Badami Hangaragi 0.1036 4270 1.0000 1 0.7058 1500 0.4182 3659 Bagalkot Badami Mangalore 0.1057 4181 1.0000 1 0.6851 2265 0.4169 3700 Bagalkot Badami Hebbali 0.1031 4284 1.0000 1 0.6985 1757 0.4160 3727 Bagalkot Badami Sulikeri 0.1049 4208 1.0000 1 0.6835 2319 0.4155 3740 Bagalkot Badami Belur 0.1335 3011 0.8722 5365 0.5940 4742 0.4105 3875 Bagalkot Badami Kittali 0.0967 4541 1.0000 1 0.6652 2938 0.4007 4141 Bagalkot Badami Kataraki 0.1054 4194 1.0000 1 0.6054 4549 0.3996 4163 Bagalkot Badami Khanapur S.K. 0.1120 3946 0.9255 4748 0.6112 4436 0.3986 4187 Bagalkot Badami Kaknur 0.1156 3787 0.8359 5608 0.6550 3309 0.3985 4191 Bagalkot Badami Neelgund 0.0936 4682 1.0000 1 0.6740 2644 0.3981 4196 Bagalkot Badami Parvati 0.1151 3813 1.0000 1 0.5368 5375 0.3953 4269 Bagalkot Badami Narasapura 0.0902 4801 1.0000 1 0.6836 2313 0.3950 4276 Bagalkot Badami Fakirbhudihal 0.0922 4725 1.0000 1 0.6673 2874 0.3948 4281 Bagalkot Badami Kainakatti 0.1024 4312 0.9758 2796 0.6097 4464 0.3935 4315 Bagalkot Badami Haldur 0.0911 4762 -

A Unique Approach to Retain Dentures in a Patient with Hypohidrotic Ectodermal Dysplasia
entistry Tavargeri et al., Dentistry 2016, 6:2 D DOI: 10.4172/2161-1122.1000362 Dentistry ISSN: 2161-1122 Case Report Open Access A Unique Approach to Retain Dentures in a Patient with Hypohidrotic Ectodermal Dysplasia Anand K Tavargeri1*, Satyabodh S Guttal2, Garima Jain3, Shruti Patil2, Rajesh Anegundi2, Vijay Trasad1 and Prashanth Battepatti1 1Department of Pedodontics, SDM College of Dental Sciences and Hospital, Dharwad, Karnataka, India 2Department of Prosthodontics, SDM College of Dental Sciences and Hospital, Dharwad, Karnataka, India 3Uttaranchal Dental and Medical Research Institute, Dehradun, Uttarakhand, India Abstract Ectodermal dysplasia is a large complex group of disorders resulting in abnormal development of two or more ectodermal structures. Oral manifestations include partial or complete anodontia and poor bony bases affecting aesthetics and function. Dental management in such patients is difficult and requires intervention throughout the growth period of the patient, until a definitive treatment is rendered. This case report describes the prosthetic rehabilitation of a young patient with total anodontia, which is a rare event in contrast to partial anodontia. A unique approach was devised to improve the retention and stability of compromised ridges. Conventional dentures were delivered to the patient with like-pole magnets incorporated in the occlusal surface of posterior denture teeth of upper and lower denture facing correspondingly which resulted in repulsive force. This enhanced retention and stability of the dentures. Keywords: Ectodermal dysplasia; Complete denture; Magnets (Figures 2a and 2b). The ridges were atrophied, reduced both in height and width for his age. The mucosa was slightly dry. Tongue was enlarged. Introduction The absence of teeth was confirmed with an orthopantomograph which Ectodermal Dysplasia (ED) is a large, complex group of clinical and showed absence of tooth buds (Figure 2c). -

Of 68 Office of the General Manager Telecom, Dharwad Telecom District
NIT No: PLG/E-Tender/9-105/AMC of AC Units/16-17/1 dated at Hubli, the 18.04.2016 Office of the General Manager Telecom, Dharwad Telecom District, 4th Floor, ‘Sanchar Sadan’, Station Road, Hubballi-580020. E- TENDER DOCUMENT for “ANNUAL MAINTENANCE CONTRACT OF WINDOW/SPLIT AC UNITS IN DHARWAD SSA” NIT No: PLG/E-Tender/9-105/AMC of AC Units/16-17/1 dated 18.04.2016. Cost of Tender Document: Rs.573/- (Rs.500+73 VAT @ 14.5%)-Non Refundable Date and Time of e-Bid Opening: 15:30 hours of 12.05.2016. Telephone Nos: 0836 2252155 or 2252044 Website: www.karnataka.bsnl.co.in Name of the Bidder ……………………………………………………………….. Page 1 of 68 NIT No: PLG/E-Tender/9-105/AMC of AC Units/16-17/1 dated at Hubli, the 18.04.2016 TABLE OF CONTENTS Section Content Page Nos QUALIFYING BID DOCUMENT Table of contents 2 Check List for Tenderers 3 1 : Part-A Detailed Notice Inviting Tender (DNIT) 4-7 1 : Part-B News Paper Notice Inviting Tender (NNIT) 8 2 Bid Form 9 3 : Part-A Bidder's Profile 10 3 : Part-B Certificates/ Undertakings 11-12 4 : Part-A General Instructions to Bidders(GIB) 13-23 4 : Part-B E-tendering Instructions to Bidders 24-29 5 : Part-A General (Commercial) Conditions of Contract (GCC) 30-38 5 : Part-B Special Conditions of Contract (SCC) 39-48 6 : Part-A Scope of work & Specification 49-51 6 : Part-B Location details 52-60 7 : Part-A Agreement Specimen 61-62 7 : Part-B Proforma for Performance Security Deposit Bank Guarantee 63-64 8 : Part-A Letter of Authorization to attend bid opening 65 8 : Part-B Details of Electronic Fund Transfer 66 FINANCIAL BID DOCUMENT 67 9 Financial Bid- Price Schedule (BOQ) 68 Page 2 of 68 NIT No: PLG/E-Tender/9-105/AMC of AC Units/16-17/1 dated at Hubli, the 18.04.2016 Check List for Tenderers Have you submitted the following documents with your Qualifying/ Financial bid? Please confirm. -

Kalghatgi Assembly Karnataka Factbook
Editor & Director Dr. R.K. Thukral Research Editor Dr. Shafeeq Rahman Compiled, Researched and Published by Datanet India Pvt. Ltd. D-100, 1st Floor, Okhla Industrial Area, Phase-I, New Delhi- 110020. Ph.: 91-11- 43580781-84 Email : [email protected] Website : http://www.indiastatelections.com Online Book Store : www.indiastatpublications.com Report No. : AFB/KA-075-0121 ISBN : 978-93-87130-78-4 First Edition : January, 2018 Third Updated Edition : January, 2021 Price : Rs. 11500/- US$ 310/- © Datanet India Pvt. Ltd. All rights reserved. No part of this book may be reproduced, stored in a retrieval system or transmitted in any form or by any means, mechanical photocopying, photographing, scanning, recording or otherwise without the prior written permission of the publisher. Please refer to Disclaimer at page no. 185 for the use of this publication. Printed in India Contents No. Particulars Page No. Introduction 1 Assembly Constituency - (Vidhan Sabha) at a Glance | Features of Assembly 1-2 as per Delimitation Commission of India (2008) Location and Political Maps Location Map | Boundaries of Assembly Constituency - (Vidhan Sabha) in 2 District | Boundaries of Assembly Constituency under Parliamentary 3-10 Constituency - (Lok Sabha) | Town & Village-wise Winner Parties- 2019, 2018, 2014, 2013 and 2009 Administrative Setup 3 District | Sub-district | Towns | Villages | Inhabited Villages | Uninhabited 11-18 Villages | Village Panchayat | Intermediate Panchayat Demographics 4 Population | Households | Rural/Urban Population -

Pllunp Special Interim
PETRONET LNG LIMITED ‐ SPECIAL INTERIM UNPAID/UNCLAIMED DIVIDEND DETAILS FOR FY 2018‐19 AS ON 31ST DECEMBER, 2018 DPID CLIENTID NAME AMOUNT SHARES 13200 1201320000021453 DILAWAR SINGH 1947.00 354 13200 1201320000102834 SHYAMA DEVI DUBEY 2200.00 400 23900 1202390000169048 JINCY LIYO . 2530.00 460 23900 1202390000237922 PAUL FRANCIS . 2200.00 400 17701 1201770100042919 MOHINI DEVI MEENA 2200.00 400 IN301330 18742064 RAJ PATI DEVI 7700.00 1400 IN302349 10132589 AVTARJIT SINGH MADAN 2200.00 400 IN300394 13712024 MAYANK JAISWAL 4400.00 800 IN301477 20059626 PARTHA PRATIM DHEKIAL 2200.00 400 IN301477 20059556 SUMIT GUPTA 3300.00 600 IN301209 10136043 SARDARI LAL CHOPRA 5500.00 1000 IN300394 13580586 SARITA DOTANIA 4400.00 800 IN300206 10651861 MUKTA JAIN 3300.00 600 IN301127 16324062 PRAVEEN KUMAR JAIN 2200.00 400 IN300118 10432748 BHAGIRATH HUF 2200.00 400 IN300118 10432843 SHIV NARAIN HUF 2200.00 400 IN301774 10573135 RAJEEV DEEWAN 2200.00 400 IN300394 13295433 SURJEET SINGH FLORA 2200.00 400 IN301766 10024830 GULSHAN KUMAR KUMRA 2200.00 400 IN300095 10345027 Jyoti Mukhi 2200.00 400 IN301143 10357542 SURINDER SINGH 2200.00 400 IN301127 15340129 PROMODH CHOPRA 1870.00 340 IN300142 10021901 SUMAN BAHL 2200.00 400 IN300394 13662004 V K POPLI 13200.00 2400 IN301127 16115427 SURJIT SINGH VIRDI 2200.00 400 IN300360 21081209 ANIL SHARMA 4400.00 800 IN300206 10216792 GAURA JOSHI 5500.00 1000 IN300118 10605912 WILLIAM TETE 2200.00 400 IN301143 10358262 JAI ARORA 3300.00 600 IN300214 12526791 PAMIT SINGH 3300.00 600 IN300888 14941037 TAPAN BIMALENDU -

(MRS). AB SALI 2 HUB0453 Dr. Amit S Galgali 3 HUB0002 DR
HUBLI - DHARWAD OBST & GYN SOCIETY 2015 SR.NO. FOGSI Membership Number TITLE NAME 1 HUB0001 DR (MRS). A.B. SALI 2 HUB0453 Dr. Amit S Galgali 3 HUB0002 DR (MRS). AMITHA .V. KAMAT 4 HUB0479 Dr. Anitha S 5 HUB0003 DR (MRS). ANJALI .S. NAREGAL 6 HUB0542 Dr. Annapurna Sambrani 7 HUB0474 Dr. Anuradha Pikle 8 HUB0446 Dr. Apurva Satish Amarnath 9 HUB0276 DR (MRS). ASHA NEERAVI 10 HUB0524 Dr. Asha M D 11 HUB0480 Dr. Asha Malladad 12 HUB0530 Dr. B S Mashal 13 HUB0277 DR. B.R.BARAKOL 14 HUB0531 Dr. S.N.Babaji 15 HUB0533 Dr. Basavaraj M.Kolli 16 HUB0006 DR BASAVARAJ SAJJAN 17 HUB0008 DR (MRS). BHARATHI .S. KORLHALLI 18 HUB0009 DR (MRS). BHARATI PUJARI 19 HUB0481 Dr. Bhavani K 20 HUB0011 Dr, Chandrika R. G. 21 HUB0482 Dr. Chandana Murthy S R 22 HUB0521 Dr. Deepa B V 23 HUB0537 Dr. Deepak V.Bhat 24 HUB0554 Dr. Dhanalakshmi Srinivas 25 HUB0013 DR (MRS). DRAKSHAYANI .S. PATIL 26 HUB0483 Dr. G. Shaila 27 HUB0525 Dr. Gayatri Hegde 28 HUB0411 Dr. Geeta Uttur 29 HUB0018 DR GOVIND P. MIRAJ 30 HUB0545 Dr. Harsha B 31 HUB0484 Dr. Hema Patil 32 HUB0019 DR (MRS). HEMALATHA .K.R. 33 HUB0023 DR (MRS). INDIRA .S. PATIL 34 HUB0465 Dr. Ishwar Malode 35 HUB0126 DR (MRS). JAMUNA KANAKARAYA 36 HUB0403 DR JAYALAXMI V KAMAT 37 HUB0149 DR (MRS). JAYASHREE DESHPANDE 38 HUB0249 DR. (MRS). JAYASHREE U. SAMBRANI 39 HUB0354 Dr. Jyothi Hiremath 40 HUB0539 Dr. Jyothi M.R. 41 HUB0469 Dr. K S Patil 42 HUB0029 DR K.P. WALVEKAR 43 HUB0030 DR (MRS). -
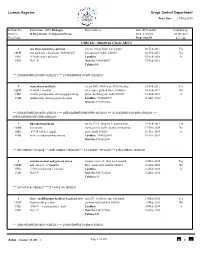
Dharwad Circle-ADC2
Licence Register Drugs Control Department Print Date : 31-Mar-2020 Sr/Firm No Firm Name , I.C / Manager Firm Address Issue Dt,Validity Cold Storage District / R.Pharmacist , Competent Person Dt,Renewal Dt, 24 Hr Open Firm Cons. Inspection Dt Lic App CIRCLE : Dharwad Circle-ADC2 1 m/s shree banashree pharma site no.190,gr.floor, narayanpur 03-Feb-2011 Yes 11151 smt parimala v kulakarni, 9880348607 oni,amargol, hubli. 580025 02-Feb-2021 No HB2 -52460-banu v kulkarni Landline. 03-Feb-2016 A PRO No C.P Mob No:9880348607 27-Feb-2016 Taluka:043 *** 20-KA/DWR/20/1397~02/02/21 *** 21-KA/DWR/21/1397~02/02/21 2 vigneshwar medicals cts.no 3007-3008, b.no.3105-06,shop 21-Feb-2011 Yes 11197 vinayak t. anaskar no.8, upper ground floor, madhura 20-Feb-2021 No HB2 -38043-pushpalatha shivayogappa shedg plaza, daziban peth, hubli 580028 21-Feb-2016 A PAR pushpalatha shivayogappa shedgali Landline. 9740606399 15-May-2017 Mob No:9972396062 *** 20-KA/DWR/20/1400~20/02/21 *** 20B-KA/DWR/20B/1059~20/02/21 *** 21-KA/DWR/21/1400~20/02/21 *** 21B-KA/DWR/21B/1008~20/02/21 3 bhavikatti medicals cts.no.172/1, shop no.5, ground floor, 19-Feb-2015 Yes 11203 b n swamy eureka tower traffic island chennamma 17-Dec-2024 No HB2 -49714-vivek i jugali circle hubli 580029 18-Dec-2019 A PAR sri b. neelakanteshwar swamy Landline. 9945525841 19-Dec-2019 Mob No:9945525841 *** 20-129280~17/12/24 *** 20B-129622~18/02/20 *** 21-129281~17/12/24 *** 21B-129623~18/02/20 4 renuka medical and general stores property no.1/a3, shop no.2 ground 16-Mar-2016 Yes 11224 smt.