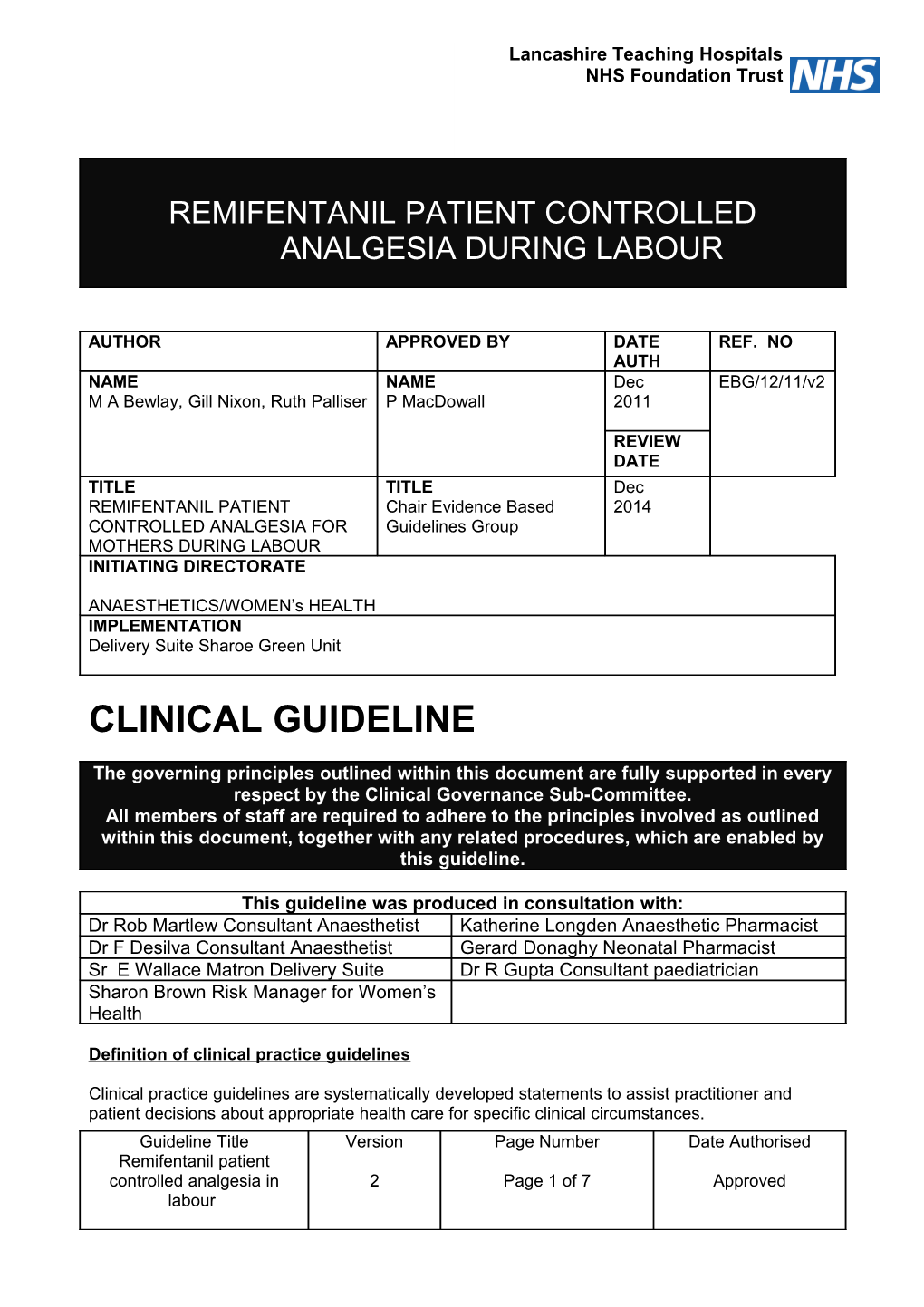
Lancashire Teaching Hospitals NHS Foundation Trust
REMIFENTANIL PATIENT CONTROLLED ANALGESIA DURING LABOUR
AUTHOR APPROVED BY DATE REF. NO AUTH NAME NAME Dec EBG/12/11/v2 M A Bewlay, Gill Nixon, Ruth Palliser P MacDowall 2011
REVIEW DATE TITLE TITLE Dec REMIFENTANIL PATIENT Chair Evidence Based 2014 CONTROLLED ANALGESIA FOR Guidelines Group MOTHERS DURING LABOUR INITIATING DIRECTORATE
ANAESTHETICS/WOMEN’s HEALTH IMPLEMENTATION Delivery Suite Sharoe Green Unit
CLINICAL GUIDELINE
The governing principles outlined within this document are fully supported in every respect by the Clinical Governance Sub-Committee. All members of staff are required to adhere to the principles involved as outlined within this document, together with any related procedures, which are enabled by this guideline.
This guideline was produced in consultation with: Dr Rob Martlew Consultant Anaesthetist Katherine Longden Anaesthetic Pharmacist Dr F Desilva Consultant Anaesthetist Gerard Donaghy Neonatal Pharmacist Sr E Wallace Matron Delivery Suite Dr R Gupta Consultant paediatrician Sharon Brown Risk Manager for Women’s Health
Definition of clinical practice guidelines
Clinical practice guidelines are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 1 of 7 Approved labour 1. Title Remifentanil Patient Controlled Analgesia Guideline for Mothers in Labour 2. Adaptation New Guideline 2. Major Recommendations
Patients must be counselled and advised by an anaesthetist in the antenatal period. This should be on a one to one basis with planned usage of the drug so that the appropriate drug quantity can be ordered for delivery suite at the appropriate time. Important that the mother is aware that remifentanil is not licensed for use in pregnancy but that much research has safely been undertaken. Inclusions patients in who epidural is contraindicated and women in whom intramuscular injections are contraindicated. Explanation of technique including possible side effects and other analgesic options available should be explained to patient. Explanation of neonatal/fetal side effects such as reduced fetal heart rate and potential neonatal respiratory depression.
Delivery Ward staff must complete their PCA competency, attend training session on induction and receive annual updates.
Staff should be familiar with the hospital resuscitation policies.
An anaesthetist sets up the PCA.
The PCA syringe should only be filled and replaced by an anaesthetist or nurse competent in the administration of remifentanil.
Always clamp the PCA line when changing the syringe to avoid accidentally giving a bolus dose of remifentanil to the patient.
Delivery Suite should possess their own PCA key, which will be kept on the CD key ring. Never leave the key unsupervised whilst it is in the PCA pump.
A dedicated remifentanil sticker should be placed in the mother’s intrapartum care pathway on commencement of the PCA. ( Appendix 1)
Midwifery/Nursing staff must: Not press the button for the patient Not alter the pump settings or prescription Not give any other opioid drugs when the PCA is in situ unless directed by anaesthetist or acute pain team. Not continue to use the PCA if the patient becomes confused and unable to press the button Not allow relatives to press the button for the patient
Maternity on call anaesthetist bleep 4154.
4. Clinical Algorithms Remifentanil Patient Controlled Analgesia algorithm enclosed in this document
Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 2 of 7 Approved labour 5. Disease/condition/target population Labouring mothers in whom an epidural or intramuscular analgesic injection is contraindicated. 6. Implementation strategy Delivery suite sisters. Pain updates and teaching sessions 7. Interventions
INDICATIONS FOR USE: For the management of labour pain in whom epidural analgesia or intramuscular analgesic injection is contraindicated.
CONTRA-INDICATIONS FOR PRESCRIBING A PCA: Absolute Confused or demented patient. Patient refusal < 36 weeks pregnant Multiple pregnancy Pre-eclampsia Opioids within the last 2 hours including epidural opioids. Allergy to remifentanil
Relative Patient unable to press patient demand button due to physical impairment. Patients who are unable to grasp the concept of PCA, either due to the language or intellect barrier Please discuss the above with the anaesthetist or acute pain team
PCA PROGRAMME:
Ensure that the PCA is prescribed on the drug prescription chart.
Use a becton dickinson luer-lock 60ml syringe (no anti-emetic to be added to syringe) Patient weight at booking or pre- pregnancy : Kg Analgesic drug: REMIFENTANIL 2mg made up to 50mls in normal Saline Concentration: 40mcg/ml PCA dose: 40 mcg ( 1 ml) Lock out Period: 2 minutes
Background Infusion: 0.025 – 0.05 mcg/kg/min added in if bolus doses not adequate.
INFORMATION FOR PATIENT AND MIDWIFE
It is administered in a safe and controlled fashion. A small amount does enter the babies system but that because it is broken down quickly there are no side effects. The bolus is administered over about a minute but then has to circulate to the brain and so it’s effect does not happen until 2 -3 minutes after pressing the button. Therefore often best to press the button immediately at the end of the previous contraction. If this is not adequate a background supplement can be given. Administration of the drug should stop once pushing begins. This gives time for the baby to eliminate the drug. After the pump is stopped Remifentanil is rapidly removed from the mother. About 30 Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 3 of 7 Approved labour minutes after stopping the pump no Remifentanil remains in the body of the mother or baby
NURSING OBSERVATIONS:
The continued presence of midwifery staff in the mothers delivery room and at least 30 minutes thereafter Following commencement of the PCA pulse oximetry/saturation monitoring must be in place continually. In addition BP, heart rate, respiratory rate and sedation observations need to be undertaken every 15 mins for the first hour, and thereafter half hourly until discontinuation of the PCA pump. Continuous fetal heart monitoring If there is a problem observations may need to be carried out more frequently until the patient is stable. The nursing observations must be documented on the intrapartum care pathway. Observations should be continued for 30 minutes after discontinuation of remifentanil. . PAIN:
Check pump for any malfunction for example not plugged in Check patency of intravenous cannula Check patient can understand principle of PCA Assess pain regularly and consistently
IF RESPIRATORY RATE < 8 AND/OR SEDATION SCORE MORE THAN 2
Stop PCA and seek urgent advise from nurse in charge/ on call anaesthetist out of hours (bleep 4154) Give oxygen at 15 litres via non-rebreathe bag Ensure naloxone available – 0.4mg(1ml) and 3ml of normal saline in syringe – give 0.1mg (1ml) increments until respiratory rate >12/min and sedation score less than 2 Check sedation score and BP.
BLOOD PRESSURE/HEART RATE:
If systolic blood pressure below 90mgHg, contact the Doctor and or Anaesthetist. If heart rate less than 50 bpm call anaesthetist bleep 4154
Lie flat with left lateral tilt and give oxygen.
Do not draw the conclusion that the intravenous remifentanil is necessarily the cause.
SIDE EFFECTS:
MOTHER The problem of side effects from the PCA should also be observed, because they are distressing for the patient.
Sedation Nausea and vomiting – antemetic to be prescribed Itching or pruritis – usually responds to treatment. Chlorphenamine 4 mg orally/10 - 20 mg
Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 4 of 7 Approved labour IM or IV. Urinary retention – a urinary catheter may be necessary.
FETUS
Potential problems include Decreased heart rate Respiratory depression These are uncommon
There is NO contraindication to breast feeding.
PCA ADMINISTRATION SETS:
The intravenous line used must be via dedicated intravenous access and a dedicated PCA line. The PCA line includes an anti-siphon valve that prevents the accidental siphoning of the contents of the remifentanil syringe into the patient and an anti-reflux valve, which prevents remifentanil infusing backwards along the secondary line. The side arm of PCA administration set to should infuse crystalloid fluid to ensure flow of remifentanil. PCA administration sets must be changed every 24 hours The position of the PCA pump should not be higher than patient chest level. The co-administration of remifentanil PCA and blood via the same intravenous access are only to be used when there is limited intravenous access and restricted to packed red cells. The PCA administration set and blood administration set must be both used in this situation.
PCA MALFUNCTION:
Stop PCA, disconnect from patient and replace with a new PCA pump Notify acute pain team (bl 2436) or anaesthetist on call for maternity (bl 4154) Send pump to medical engineering for check and repair Complete critical incident form
LENGTH OF TIME PCA TO REMAIN INSITU:
PCA opioid syringes prepared in clinical areas should be renewed every 24 hours.
DISPOSAL OF SYRINGE CONTENTS: A registered nurse should dispose of the remaining opioid, witnessed by a member of the nursing staff Safe prescribing and Administration of Medicines Trust Policy Liquid medications should be disposed of using a doop pot. The amount wasted should be documented onto the prescription chart, timed, dated and signed. The pump should then be cleaned, returned to theatre recovery area.
8. Major Outcomes Patient Controlled analgesia will be delivered in a safe and effective manner on delivery suite.
Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 5 of 7 Approved labour 9. Reference(s) Can J Anaesth. 2007 Aug;54(8):626-33 Remifentanil patient-controlled analgesia for labour: optimizing drug delivery regimens.Balki M, Kasodekar S, Dhumne S, Bernstein P, Carvalho JC. Can J Anaesth. 2001 March P 175 -78. Obstetrical and Pediatric Anaesthesia Patient-controlled intravenous analgesia using remifentanil in the parturient. Fabienne Roelants MD, Emmanuelle De Franceschi MD, Francis Veyckemans MD, Patricia Lavand’homme MD PhD.
BJA 2001; 87: 415 – 20 Patient Controlled analgesia for labour using remifentanil: a feasibility study. Blair J M, Hill D A
BJA 2000; 84:411. Patient Controlled analgesia in labour using remifentanil in two parturients with platelet abnormalities. Thurlow J A, Waterhouse P.
BJA 2005 95 (4): 504–9 Maternal and neonatal side-effects of remifentanilpatient-controlled analgesia in labour. I. Volikas1*, A. Butwick2, C. Wilkinson3, A. Pleming4 and G. Nicholson2
10. Guideline Availability Intranet. Delivery Suite, Antenatal Clinic 11. Companion Documents None 12. Patient Resources Counselling by anaesthetist in antenatal period.
Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 6 of 7 Approved labour APPENDIX 1
Lancashire Teaching Hospitals NHS Foundation Trust REMIFENTANIL PCA IN USE Please tick !
Explanation of the technique given to mother
Concentration of remifentanil made as per guideline
Maternal monitoring as per guideline -continuous saturations, HR,BP, RR, Sedation
Fetal Heart Rate Monitoring as per guideline Signature Date Time
Guideline Title Version Page Number Date Authorised Remifentanil patient controlled analgesia in 2 Page 7 of 7 Approved labour