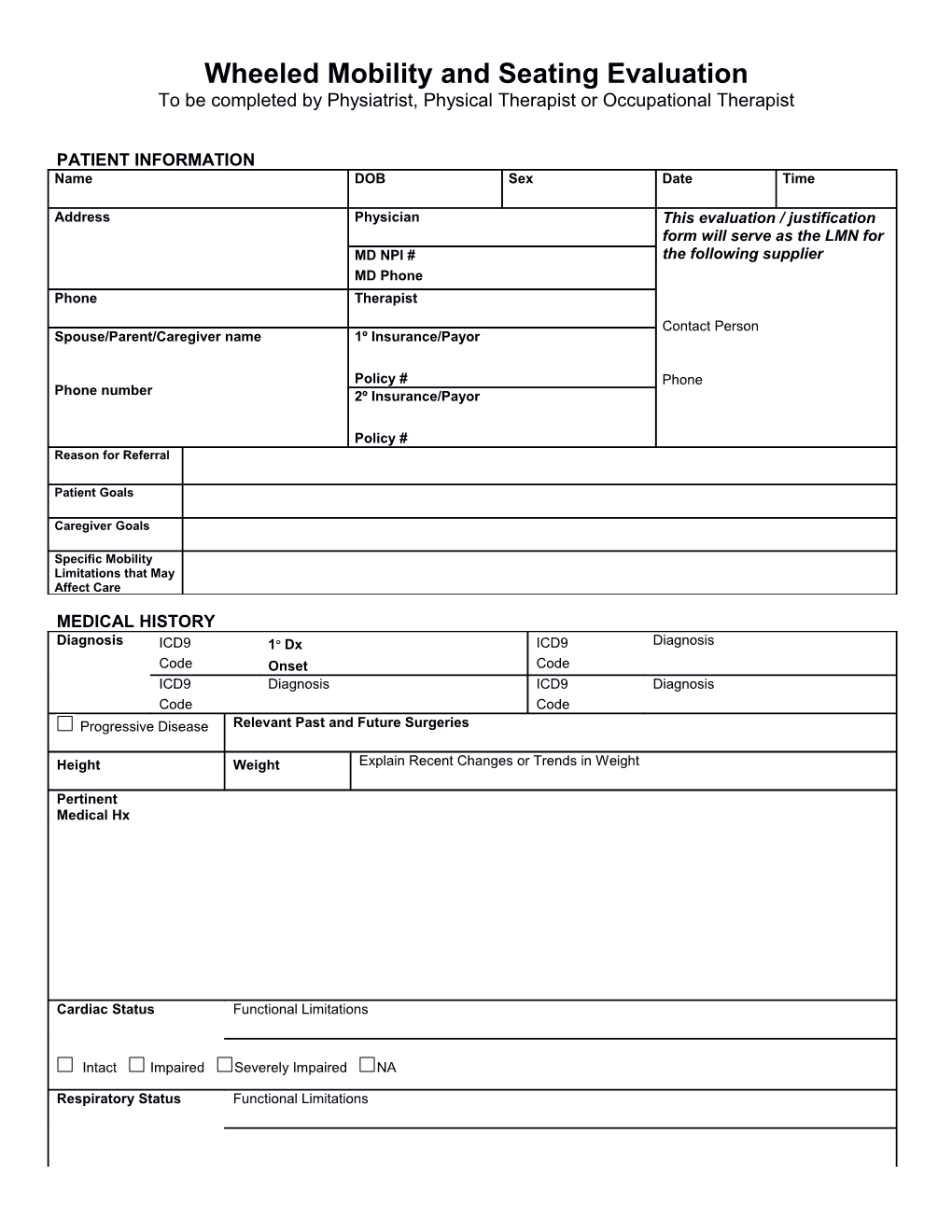
Wheeled Mobility and Seating Evaluation To be completed by Physiatrist, Physical Therapist or Occupational Therapist
PATIENT INFORMATION Name DOB Sex Date Time
Address Physician This evaluation / justification form will serve as the LMN for MD NPI # the following supplier MD Phone Phone Therapist Contact Person Spouse/Parent/Caregiver name 1º Insurance/Payor
Policy # Phone Phone number 2º Insurance/Payor
Policy # Reason for Referral
Patient Goals
Caregiver Goals
Specific Mobility Limitations that May Affect Care
MEDICAL HISTORY Diagnosis ICD9 1o Dx ICD9 Diagnosis Code Onset Code ICD9 Diagnosis ICD9 Diagnosis Code Code Progressive Disease Relevant Past and Future Surgeries
Height Weight Explain Recent Changes or Trends in Weight
Pertinent Medical Hx
Cardiac Status Functional Limitations
Intact Impaired Severely Impaired NA
Respiratory Status Functional Limitations Patient Name
Intact Impaired Severely Impaired O2 L / Min.
Orthotics
Prosthetics
Page 2 of 25 Patient Name
CURRENT SEATING / MOBILITY Current Mobility Base None Stroller Manual w/c Manual with tilt Manual with recline Scooter
Power Power w/ tilt Power w/ recline Power w/ tilt & recline w/ seat elevator w/ stand
Type of Control Manufacturer Model Serial # Color Age Additional Components
Seat Height Seat Width Seat Depth Condition of Current Mobility Base Problems with Current Mobility Base
Current Seating System Age of Seating System COMPONENT MANUFACTURER / CONDITION Seat Base Mounting Hardware Cushion Pelvic Support Thigh Support Knee Support Foot Support Foot Strap / Heel Loop Back Mounting Hardware Lateral Trunk Supports Chest / Shoulder Support Head Support Mounting Hardware UE Support Mounting Hardware Other Other When Relevant Overall Seat Height Overall W/C Length Overall W/C Width Describe Posture in Present Seating System
CURRENT MRADL STATUS (with present Mobility Assistive Equipment) Inde Assist Not Comments / Equipment p asses sed Dressing
Eating
Grooming/Hygiene
Page 3 of 25 Patient Name Toileting
Bathing
IADLS Bowel Mgmt Continent Incontinent Accidents Comments
Bladder Mgmt Continent Incontinent Accidents Comments
DESCRIBE WHAT HAS CHANGED TO REQUIRE NEW AND/OR DIFFERENT MOBILITY ASSISTIVE EQUIPMENT
Page 4 of 25 Patient Name
HOME ENVIRONMENT House Condo/Town Home Apartment Asst Living LTCF SNF Own Rent
Lives Alone / No Caregivers Lives Alone / Caregiver Asst Lives with Caregiver Hours Home Alone
Comments Home is Accessible to Equipment Storage of Wheelchair In Home Other
Stairs Yes No Ramp Yes No
Comments
COMMUNITY ADL TRANSPORTATION Car Van Public Transportation Adapted W/C Lift Ambulance Other Sits in Wheelchair During Transport
Tie Downs Where is W/C Stored During Transport? Self Driver Drive While in Wheelchair Yes No Passenger only Yes No
Employment Specific requirements pertaining to mobility
School Specific requirements pertaining to mobility Other
STRENGTH / RANGE OF MOTION Gross Overall Strength Gross Range of Motion Upper Extremity Lower Extremity Shoulder
Normal 5 / 5 Normal 5 / 5 Elbow
Good 4 / 5 Good 4 / 5 Wrist
Fair 3 / 5 Fair 3 / 5 Hand
Poor 2 / 5 Poor 2 / 5 Hip
Trace 1/ 5 Trace 1/ 5 Knee
No Movement No Movement Ankle
Manual Muscle Test on file/noted on pages 6 & 7 Goniometric Measurements on file/noted on page 6 & 7
Manual Muscle Test not on file Goniometric Measurements not on file
Patient has sufficient strength and range of motion to ambulate and participate in MRADLs.
Patient does not have sufficient strength and/or range of motion to ambulate and participate in MRADLs.
Patient has sufficient strength and range of motion to propel a manual W/C and participate in MRADLs.
Patient does not have sufficient strength and/or range of motion to propel a manual W/C and participate in MRADLs.
Patient has sufficient strength and range of motion to operate a POV and participate in MRADLs.
Patient does not have sufficient strength and/or range of motion to operate a POV and participate in MRADLs.
Page 5 of 25 Patient Name Comments
BALANCE Static Sitting Dynamic Sitting Static Standing Dynamic Standing Normal / WFL Normal / WFL Normal / WFL Normal / WFL
Good / Min Asst Good / Min Asst Good / Min Asst Good / Min Asst
Fair / Mod Asst Fair / Mod Asst Fair / Mod Asst Fair / Mod Asst
Poor / Max Asst Poor / Max Asst Poor / Max Asst Poor / Max Asst
Unable/Dependant Unable/Dependant Unable/Dependant Unable/Dependant
Patient has sufficient balance to ambulate and participate in MRADLs.
Patient does not have sufficient balance to ambulate and participate in MRADLs.
Patient has sufficient balance to propel a manual W/C to participate in MRADLs.
Patient does not have sufficient balance to propel a manual W/C to participate in MRADLs.
Patient has sufficient balance and endurance to operate a POV and participate in MRADLs.
Patient does not have sufficient balance and/or endurance to operate a POV and participate in MRADLs.
Comments
Page 6 of 25 Patient Name
VISUAL / PERCEPTUAL and SENSORY PROCESSING SKILLS Right Eye Intact Left Eye Intact Comments Vision Right Eye Impaired Left Eye Impaired
Perceptual Perceptual Skills Intact Perceptual Skills Impaired Comments
Motor Planning Intact Impaired N/A or NT Comments
Handedness Right Left N/A Comments
Patient has sufficient vision, perception and motor planning to operate MAE and participate in MRADLs.
Patient does not have sufficient vision, perception and/or motor planning to safely operate MAE and participate in MRADLs.
Comments
SENSATION and SKIN INTEGRITY Sensation Pressure Relief Intact Impaired Absent Able to perform effective pressure relief Yes No Method Hyposensate Hypersensate If not, Why? Please describe
Skin Issues / Skin Integrity Current Skin Integrity History of Skin Issues Yes No Hx of Skin Surgery Yes No Intact Red Area Open Area
Where Where Where When When Size Scar Tissue At Risk -Prolonged Sitting Limited Sitting Tolerance Yes No Hours per Day Braden Score, if administered Complaint of Pain 0 1 2 3 4 5 6 7 8 9 10
VERBAL COMMUNICATION WFL Receptive WFL Expressive Understandable Difficult to Understand Sign Non-communicative
Uses an Augmentative Communication Device Manufacturer/Model
AAC Mount Needed
TRANSFERS and AMBULATION Transfers Ambulation Independent Independent all Distances & Terrains Standby/Contact Asst w/ device w/o device
Min Assist Indep. Short Distance ( ft.) Min Physical Asst w/ device w/o device
Mod Asst Indep. Smooth/Level Surfaces Mod Physical Asst w/ device w/o device
Max Asst Indep. with Device ( ft.) Max Physical Asst w/ device w/o device
Page 7 of 25 Patient Name Dependent Unable to Ambulate
Sliding Board Comments
Lift / Sling Required
Timed Up and Go Test sec. [60-69 y 8.1sec (7.1-9.0), 70-79 y 9.2 sec (8.2-10.2), 70-99 y 11.3 sec (10.0-12.7)]
EXPLAIN WHY PATIENT IS NON-AMBULATORY or NOT A FUNCTIONAL AMBULATOR
Page 8 of 25 Patient Name
WHEELCHAIR SKILLS (Shown by Trial) Indep Assist Dependent N/A Comments /Unable Manual W/C Propulsion Safe Functional Distance
UE or LE strength and endurance is sufficient to Method
participate in MRADLs using a manual wheelchair Arm Left Right Both UE or LE strength and/or endurance is not sufficient to Foot Left Right Both participate in MRADLs using a manual wheelchair Operate Scooter Safe Functional Distance
Strength, hand grip, balance, control & transfers are appropriate for scooter use.
Strength, hand grip, balance, control or transfers are not appropriate for scooter use.
Living environment is appropriate for scooter use.
Living environment is not appropriate for scooter use.
Operate PWC w/ Joystick & Standard Safe Functional Distance Programming Operate PWC w/ Joystick & Advanced Safe Functional Distance Programming Operate PWC w/ Alternative Control Safe Functional Distance
COMMENTS
MAT EVALUATION
Measurements in Sitting Left Right A Shoulder Width H Seat to Top of Shoulder B Chest Width I Acromium Process (Tip of Shoulder) C Chest Depth (Front – Back) J Inferior Angle of Scapula
Page 9 of 25 Patient Name D Hip width K Seat to Iliac Crest E Between Knees L Seat to Elbow F Top of Head M Upper leg length G Occiput N Lower leg length + Overall width (asymmetrical width for O Foot Length + windswept legs or scoliotic posture
Page 10 of 25 Patient Name
POSTURE COMMENTS Anterior / Posterior Obliquity Rotation-Pelvis P
E L V I S Neutral Posterior Anterior WFL R elev* L elev* WFL Right Left *viewed from behind Anterior Anterior
Non Reducible Other Non Reducible Other Non Reducible
Partly Reducible Partly Reducible Other Partly Reducible Reducible Reducible Reducible
TRUNK Anterior / Posterior Left / Right Rotation-shoulders and upper trunk
Neutral
WFL Thoracic Lumbar WFL Convex Convex Left-anterior Kyphosis Lordosis Left Right c-curve s-curve multiple Right-anterior
Non Reducible Other Non Reducible Other Non Reducible Other
Partly Reducible Partly Reducible Partly Reducible
Reducible Reducible Reducible
Position Windswept Hip ROM Limitations
H I P S Neutral Right Left Neutral ABduct ADduct Non Reducible Dislocated Non Reducible Other
Partly Reducible Subluxed Partly Reducible
Reducible Reducible
Knee Position Foot Position KNEES WFL L R WFL L R
Page 11 of 25 Patient Name & Limitations L R Limitations L R Dorsi-Flexed L R FEET Non Reducible L R Non Reducible L R Plantar Flexed L R
Partly Reducible L R Partly Reducible L R Inversion L R
Reducible L R Reducible L R Eversion L R
DESCRIBE REFLEXES/TONAL INFLUENCE ON BODY
Page 12 of 25 Patient Name
POSTURE COMMENTS Functional Good Head control Describe Tone//Movement of Head and Neck HEAD Flexed Extended Adequate Head Contol
& Rotated L Rotated R Limited Head Control NECK Lat Flexed Lat Flexed L Absent Head Control R Cervical Hyperextension
U SHOULDERS Describe Tone/Movement P Left Right of the Upper Extremities P E Functional Functional Good UE movement/control R Elevated Elevated Functional UE mvmt./control
Depressed Depressed Limited UE movement/control
Protracted Protracted Absent UE movement/control
E Retracted Retracted
X Subluxed Subluxed
T R E M ELBOWS I Left Right T Y & Fisting Fisting
HAND
Goals for Wheelchair Mobility Independence with mobility in the home with mobility related ADLs (MRADLs)
Independence with community mobility
Dependent mobility for safe transport
Other – describe
Goals for Seating System Optimize pressure distribution
Provide support needed to facilitate function or safety
Provide corrective forces to assist with maintaining or improving posture
Accommodate client’s posture- Current seated postures and positions are not reducible or will not tolerate corrective forces
Client to be independent with relieving pressure in the wheelchair
Page 13 of 25 Patient Name Enhance physiological function such as breathing, swallowing, digestion and/or bowel/bladder elimination
Other – describe
EQUIPMENT TRIALS AND RESULTS
Page 14 of 25 Patient Name
MOBILITY BASE RECOMMENDATIONS and JUSTIFICATION MOBILITY BASE JUSTIFICATION Manufacturer provide transport from point A to B width/depth necessary to Model Color promote independent mobility accommodate anatomical Seat Width measurement Seat Depth not a safe, functional ambulator
Length of need walker or cane inadequate
non-ambulatory
Lightweight Manual Wheelchair self propulsion
High-strength Lightweight MWC self propulsion lifting
full-time daily use requires features not available
on a lightweight manual wheelchair
Ultra-lightweight MWC improved UE access to wheels increase chair stability
Axle position adjustment efficient propulsion change angle for improved vertical (dump) horizontal postural stability rotational (camber)
Heavy-duty Manual Wheelchair user weight broken frame on previous chair
Extra Heavy-duty MWC extreme tone/excess movement
Scooter/POV non-ambulatory has adequate trunk stability
non-functional ambulator can safely operate & is willing to
cannot functionally propel manual can safely transfer
wheelchair
Power Wheelchair non-ambulatory requires speed adjustment
non-functional ambulator requires torque adjustability
cannot functionally propel manual requires sensitivity adjustability
wheelchair requires acceleration cannot functionally and safely adjustability operate scooter/POV requires braking adjustability home environment does not requires expandable electronics support the use of a POV requires alternative drive control can safely operate & is willing to required to negotiate an incline can safely transfer of required to negotiate a rise of
Page 15 of 25 Patient Name Stroller Base infant/child non-functional ambulator
unable to propel manual non-functional UE
wheelchair
Tilt Base or Tilt Feature Added change position against transfers
Forward Rearward gravitational force on head and management of tone shoulders Powered tilt on power chair change position for pressure rest periods
Powered tilt on manual chair redistribution/cannot weight shift control edema
Manual tilt on manual base facilitate postural control
Manual tilt on power base
Recline accommodate femur to back angle rest periods
Power recline on power base bring to full recline for ADL care repositioning for transfers or
Power recline on manual base change position for pressure clothing/diaper/catheter management Manual recline on manual base redistribution/cannot weight shift head positioning
Manual recline on power base
Power Seat Elevator increase Indep in transfers
Power Standing Feature increase Indep in ADLs
Page 16 of 25 Patient Name
MOBILITY BASE COMPONENTS JUSTIFICATION Armrests provide support with elbow at 90 remove for transfers fixed adjustable height removable provide support for w/c tray allow to come closer to table top swing away flip back reclining change height/angle for ADLs remove for access to tables full length desk length tubular
Footrests/ Leg rests provide LE support manage tone/spasticity 60 70 80 90 heavy duty accommodate knee ROM enable lateral transfers fixed lift off swing away elevate legs w/tilt and/or recline decrease edema elevating articulating elevating provide change in position for legs physically unable to operate power elevating legrests maintain feet on footplate manual elevating legrests power articulating elevating legrests
Foot Platform provide LE support elevate legs w/ tilt and/or recline flip up power elevating accommodate hip abduction change in position for legs power articulating elevating minimize turning radius decrease edema
maintain feet on footplate
enable transfers
Foot support provide foot support transfers flip up fixed/rigid accommodate ankle ROM adjustable angle R L allow foot to go under w/c base multi-adjustable angle R L
Drive/propulsion wheel size increase access to wheel increase propulsion ability Wheel style mag spokes allow seating system to fit on base maintenance free
Wheel rims/ hand rims increase self-propulsion with hand standard plastic coated other weakness/decreased grasp projections oblique vertical
Drive/propulsion tires decrease maintenance decrease pain pneumatic semi-pneumatic prevent frequent flats decrease spasms flat free inserts solid increase shock absorbency
Caster housing maneuverability decrease pain Caster size Style stability of wheelchair decrease spasms pneumatic semi-pneumatic increase shock absorbency allow feet under wheelchair base flat free inserts solid
Page 17 of 25 Patient Name durability seat to floor height
maintenance
Specific seat height foot propulsion accommodation of leg length Front Back transfers
postural stability
Shock absorbers decrease vibration
decrease pain
Spoke protector protect hand/fingers from spokes
Side guards prevent skin tears/abrasions
One armed drive attachment R L enable propulsion of manual
wheelchair with one arm Anti-tippers prevent rearward displacement
Amputee adapter increase rearward stability
Wheel locks indep in applying wheel locks push pull scissor
Extension R L
Transportation tie-down option provide crash tested brackets
Push handles caregiver access allows “hooking” to enable extended angle adjustable caregiver assist increased ability to perform ADLs, standard maintain balance or pressure relief
Angle adjustable back postural control UE functional control
control of tone/spasticity accommodate seating system
accommodate range of motion
Crutch/Cane holder IV hanger
Cylinder holder Vent tray
Page 18 of 25 Patient Name
Page 19 of 25 Patient Name MOBILITY BASE COMPONENTS JUSTIFICATION POWER WHEELCHAIR CONTROLS provides access for controlling Proportional wheelchair Type
Body Part(s) Left Right
lacks motor control to operate
Non-Proportional/switches proportional drive control Type unable to understand proportional controls Body Part(s) programming for accurate control
Upgraded/Expandable Electronics progressive disease/changing
condition to operate power seat function(s)
through drive control
Display box to see which mode and drive the wheelchair is set necessary for alternate controls
Digital Interface Electronics to allow the w/c to operate when
using alternative drive controls Head Array to operate wheelchair through
switches placed in tri-panel headrest Sip and puff w/ Tubing Kit needed to operate sip and puff
drive controls Upgraded Tracking Electronics increase safety when driving
correct tracking when on uneven
Safety Reset Switches surfaces
to change modes and stop the
Single or Multiple Actuator Control wheelchair when driving in latch mode
Module to operate the power seat
function(s) through the drive control Mount for switches or joystick attaches switches to w/c midline for optimal placement
swing away for safe transfers provides for consistent access
Page 20 of 25 Patient Name Attendant controlled joystick safety compliance with transportation and mount long distance driving regulations
operation of seat functions
Battery power motors on wheelchair
Charger charge battery for wheelchair
Push rim active assist enable propulsion of manual enable propulsion of manual
wheelchair on sloped terrain wheelchair for distance Other
Other
Page 21 of 25 Patient Name
SEATING / POSITIONING COMPONENT RECOMMENDATIONS AND JUSTIFICATION COMPONENT Mfg/model/size JUSTIFICATION Seat cushion impaired sensation stabilize pelvis
decubitus ulcers present prevent pelvic extension
history of decubitus ulcers accommodate obliquity/rotation
increase pressure distribution accommodate multiple deformity
neutralize LE
Seat cushion- commercially available cushion cannot accommodate deformity
Custom Molded
Seat wedge accommodate ROM
aggressive seat shape to
decrease sliding down in the seat Cover replacement protect back or seat cushion
Mounting hardware fixed attach seat platform/cushion swing-away for safe transfers
lateral supports attach back platform/cushion flip-down/away for safe transfers swing headrest mount postural support(s) multi-axis for accurate positioning away medial thigh support & removal for safe transfers
back seat
Seat board support cushion to prevent attach cushion/back to base
Seat platform hammocking of upholstery accommodate seat to floor height
Back board
Back cushion provide posterior trunk support provide lumbar/sacral support
provide posterior/lateral trunk support trunk in midline
support pressure relief over spinous accommodate deformity processes accommodate or decrease tone
facilitate tone
Back cushion- commercially available back cannot accommodate deformity
Custom Molded
Lateral pelvic / R L pelvis in neutral accommodate tone
thigh support accommodate pelvis removable for transfers
Page 22 of 25 Patient Name position upper legs
Medial thigh decrease adduction remove for transfers
support accommodate ROM alignment
Foot support R L position foot stability
Foot box accommodate deformity decrease tone
Shoe holder control position
Ankle strap / support foot on foot support provide input to heel
heel loops decrease extraneous movement protect foot
Lateral trunk R L decrease lateral trunk leaning safety
supports accommodate asymmetry control of tone
contour for increased contact
Anterior chest decrease forward movement of added abdominal support
strap, vest, or shoulder alignment shoulder retractors accommodation of TLSO assistance with shoulder control decrease forward movement of trunk decrease shoulder elevation
Page 23 of 25 Patient Name COMPONENT Mfg/model/size JUSTIFICATION Headrest provide posterior head improve respiration
support placement of switches provide posterior neck safety support provide lateral head accommodate ROM
support accommodate tone provide anterior head improve visual support support during tilt and orientation
recline improve feeding
Neck support decrease neck rotation decrease forward neck
flexion
Upper extremity R L decrease edema decrease gravitational
support decrease subluxation pull on shoulders Arm trough provide midline control tone ______Hand support positioning provide work surface provide support for UE ½ tray placement for function Full tray provide hand support in AAC/Computer/EADL Swivel mount natural position
Pelvic positioner stabilize tone pad for protection over boney
Single pull belt decrease falling out of chair prominence prominence comfort Specialized belt prevent excessive rotation special pull angle to control SubASIS bar /other rotation Essential needs Holds diapers catheter/hygiene medicines special food bag or pouch ostomy supplies orthotics clothing changes
Other Other
Page 24 of 25 Patient Name Follow up / Plan of Care
Patient/Caregiver Signature Date Therapist Name Printed Therapist’s Signature Date Supplier’s Name Printed Supplier’s Signature Date
I agree with the above findings and recommendations of the therapist and supplier Physician’s Name Printed Date Physician’s Signature
This is to certify that I, the above signed therapist have the following affiliations This DME Supplier
Manufacturer of Recommended Equipment
Patient’s Long Term Care Facility
None of the above
Page 25 of 25