Adult Emergency Nurse Protocol HYPEREMESIS GRAVIDARUM 20XX
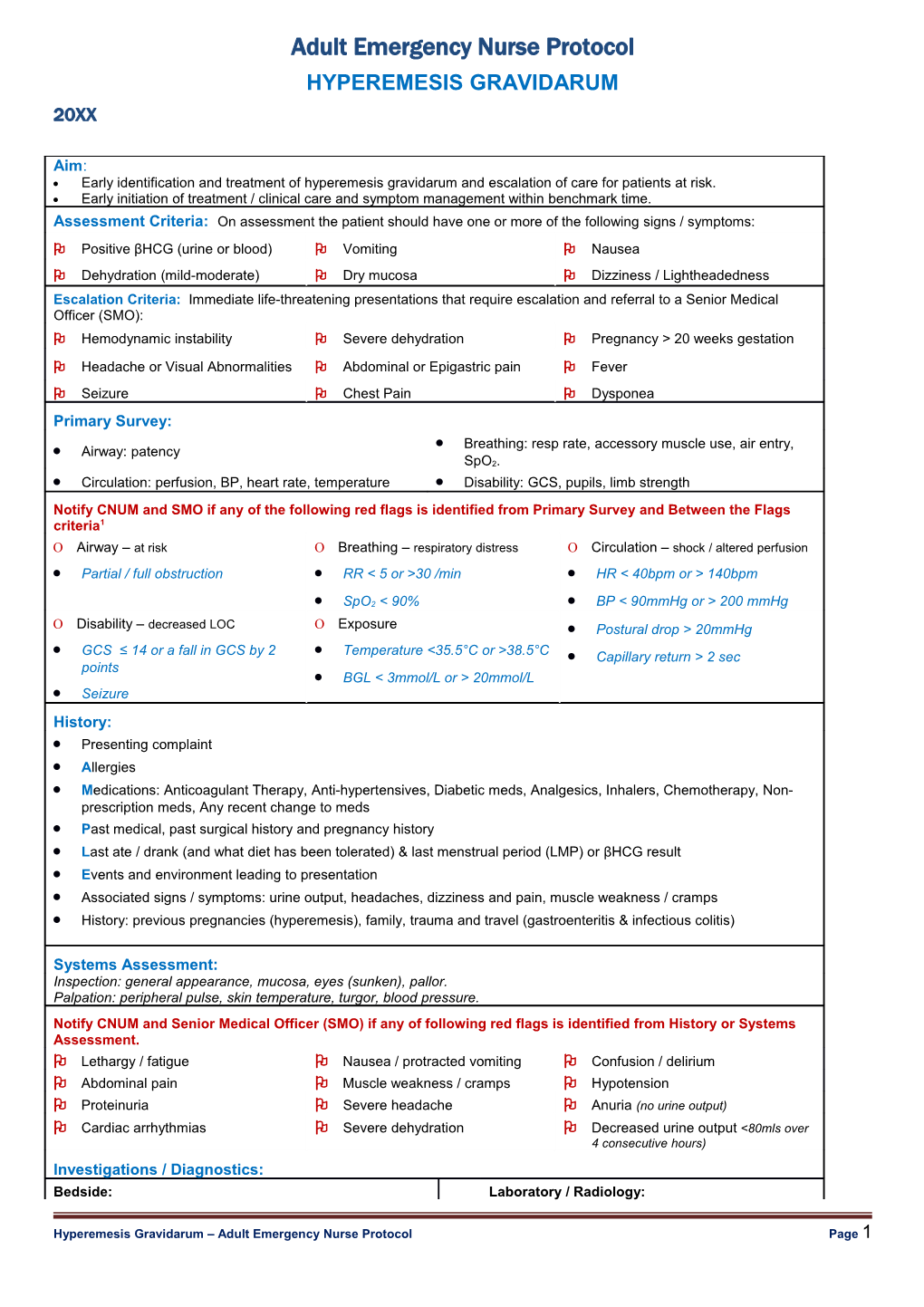
Aim: Early identification and treatment of hyperemesis gravidarum and escalation of care for patients at risk. Early initiation of treatment / clinical care and symptom management within benchmark time. Assessment Criteria: On assessment the patient should have one or more of the following signs / symptoms: Positive βHCG (urine or blood) Vomiting Nausea Dehydration (mild-moderate) Dry mucosa Dizziness / Lightheadedness Escalation Criteria: Immediate life-threatening presentations that require escalation and referral to a Senior Medical Officer (SMO): Hemodynamic instability Severe dehydration Pregnancy > 20 weeks gestation
Headache or Visual Abnormalities Abdominal or Epigastric pain Fever Seizure Chest Pain Dysponea Primary Survey: Breathing: resp rate, accessory muscle use, air entry, Airway: patency SpO2. Circulation: perfusion, BP, heart rate, temperature Disability: GCS, pupils, limb strength Notify CNUM and SMO if any of the following red flags is identified from Primary Survey and Between the Flags criteria1 Airway – at risk Breathing – respiratory distress Circulation – shock / altered perfusion Partial / full obstruction RR < 5 or >30 /min HR < 40bpm or > 140bpm
SpO2 < 90% BP < 90mmHg or > 200 mmHg Disability – decreased LOC Exposure Postural drop > 20mmHg GCS ≤ 14 or a fall in GCS by 2 Temperature <35.5°C or >38.5°C Capillary return > 2 sec points BGL < 3mmol/L or > 20mmol/L Seizure History: Presenting complaint Allergies Medications: Anticoagulant Therapy, Anti-hypertensives, Diabetic meds, Analgesics, Inhalers, Chemotherapy, Non- prescription meds, Any recent change to meds Past medical, past surgical history and pregnancy history Last ate / drank (and what diet has been tolerated) & last menstrual period (LMP) or βHCG result Events and environment leading to presentation Associated signs / symptoms: urine output, headaches, dizziness and pain, muscle weakness / cramps History: previous pregnancies (hyperemesis), family, trauma and travel (gastroenteritis & infectious colitis)
Systems Assessment: Inspection: general appearance, mucosa, eyes (sunken), pallor. Palpation: peripheral pulse, skin temperature, turgor, blood pressure. Notify CNUM and Senior Medical Officer (SMO) if any of following red flags is identified from History or Systems Assessment. Lethargy / fatigue Nausea / protracted vomiting Confusion / delirium Abdominal pain Muscle weakness / cramps Hypotension Proteinuria Severe headache Anuria (no urine output) Cardiac arrhythmias Severe dehydration Decreased urine output <80mls over 4 consecutive hours) Investigations / Diagnostics: Bedside: Laboratory / Radiology:
Hyperemesis Gravidarum – Adult Emergency Nurse Protocol Page 1 BGL: If < 3 or > 20mmol/L notify SMO Pathology: Refer to local nurse initiated STOP ECG: [as indicated] looks for changes suggesting FBC, UEC, LFTs (moderate-severe dehydration) hypokalaemia or hypocalcemia Group and Hold (if bleeding suspected) Blood Cultures (if Temp ≤35 or ≥38.5°C) Urinalysis / MSU (if indicated) Radiology: Not generally indicated
Hyperemesis Gravidarum – Adult Emergency Nurse Protocol Page 2 Adult Emergency Nurse Protocol HYPEREMESIS GRAVIDARUM 20XX
Nursing Interventions / Management Plan: Resuscitation / Stabilisation: Symptomatic Treatment: Oxygen therapy & cardiac monitor [as indicated] Antiemetic: as per district standing order IV Cannulation (16-18gauge if unstable) Analgesia: as per district standing order IV Fluids: Sodium Chloride 0.9% 1 Litre IV stat (discuss IV Fluids: as per district standing order with SMO)
Supportive Treatment: Fluid Balance Chart (FBC) Nil By Mouth (NBM) or Urinalysis: Ketones and Specific Gravity Trial of Fluids Bowel chart [as indicated] Monitor vital signs as clinically indicated Consider devices: IDC, Nasogastric tube [as indicated] (BP and postural BP, HR, T, RR, SpO2) Monitor pain assessment / score Practice Tips / Hints: Defined as persistent vomiting, volume depletion, ketosis, electrolyte disturbances and weight loss.2 Typical Presentation in weeks 4-7 after LMP2 Concentrations of sodium, potassium and chloride may be reduced from low intake resulting in hypokalemic alkalosis.3 ECG changes suggesting Hypokalaemia include; ST segment depression, decrease in amplitude of T wave and increase in amplitude in U wave. Arrhythmias may also be present.4 ECG changes suggesting Hypocalemia include a prolonged QT interval. The patient may also experience hypotension. 5 Preelampsia exhibits signs and symptoms of headache, visual abnormalities, abdominal pain, epigastric pain, chest pain and dyspnea. Observe for ketotic (acetone) breath.2 Pregnant women should avoid > 12hrs without meals to avoid hypoglycaemia.3 Delay in treatment in hyperemesis can cause intrauterine growth restriction. 3 Patient education is important as most of the treatment includes dietary changes. Patient factsheets can be located through the UpToDate website or http://www.uptodate.com/contents/hyperemesis- gravidarum-the-basics?source=search_result&search=hyperemesis+gravidarum&selectedTitle=3%7E73 Further Reading / References: 1. SESLHD Patient with Acute Condition for Escalation (PACE): Management of the Deteriorating Adult and Maternity Inpatient SESLHD/PR283. http://www.seslhd.health.nsw.gov.au/Policies_Procedures_Guidelines/Clinical/Other/SESLHDPR283-PACE- MgtOfTheDeterioratingAdultMaternityInpatient.pdf. 2. BMJ: http://bestpractice.bmj.com.acs.hcn.com.au/best-practice/monograph/999.html 3. Pillitteri, A. 2003. Maternal & Child Health Nursing: Care of the Childbearing & Childrearing Family, 4th ED. Lippincott Williams & Wilkins, Philadelphia. 4. UpToDate (2013) Clinical Manifestations and Treatment of Hypokalemia. Accessed 2014, from: http://www.uptodate.com/contents/clinical-manifestations-and-treatment-of-hypokalemia? source=search_result&search=hypokalemia&selectedTitle=1%7E150 (2013) 5. UpToDate (2013) Clinical Manifestations of Hypocalcemia. Accessed 2014, from : http://www.uptodate.com/contents/clinical-manifestations-of-hypocalcemia? source=search_result&search=hypocalcemia&selectedTitle=4%7E150 (2013) 6. UpToDate (2013) Pre-eclampsia, clinical features and diagnosis. Accessed 2014, from: http://www.uptodate.com/contents/preeclampsia-clinical-features-and-diagnosis?source=see_link (2014)
Acknowledgements: SESLHD Adult Emergency Nurse Protocols were developed & adapted with permission from: Murphy, M (2007) Emergency Department Toolkits. Westmead Hospital, SWAHS Hodge, A (2011) Emergency Department, Clinical Pathways. Prince of Wales Hospital SESLHD. Revision & Approval History Date Revision No. Author and Approval
Hyperemesis Gravidarum – Adult Emergency Nurse Protocol Page 3 Hyperemesis Gravidarum – Adult Emergency Nurse Protocol Page 4