NONINVASIVE VENTILATION DURING THE WEANING PROCCESS
IN CHRONICALLY CRITICALLY ILL PATIENTS
Online Supplemental Material
Jesus Sancho1, Emilio Servera1,2, Luis Jara-Palomares3, Emilia Barrot3, Raquel
Sanchez-Oro-Gómez3, F Javier Gómez de Terreros4,5, M Jesús Martín-Vicente4,5,
Isabel Utrabo4,5, M Belen Núñez5,6, Alicia Binimelis5,6, Ernest Sala5,6, Enrique
Zamora7, Gonzalo Segrelles7, Angel Ortega-Gonzalez8, Fernando Masa4,5. Spanish
Respiratory Intermediate Care Units Group
1Respiratory Care Unit. Respiratory Medicine Department. Hospital Clínico
Universitario, Valencia. Spain. INCLIVA Institute of Health Reasearch. Valencia. Spain
2Universitat de Valencia. Spain
3Unidad Médico-Quirurgica de Enfermedades Respiratorias. Hospital Virgen del Rocio.
Sevilla. Spain
4Servicio de Neumología. Hospital San Pedro Alcántara. Cáceres. Spain
5Centro de Investigación Biomédica de Enfermedades Respiratorias (CIBERES). IS
CIII. Madrid. Spain
6Servicio de Neumología. Hospital Son Espases. Palma de Mallorca. Spain
7Intermediate Care Unit. Pulmonology Department. La Princesa Institute for Health
Research. Hospital Universitario de La Princesa. Madrid. Spain
8Servicio de Neumología. Hospital Nuestra Señora del Prado. Talavera de la Reina.
Spain
Conflict of Interest: authors have no financial relationship with any commercial entity that has an interest in the subject of this manuscript.
Corresponding Author:
Jesus Sancho Respiratory Care Unit. Respiratory Medicine Department
Hospital Clínico Universitario
Blasco Ibañez 17
46010 Valencia. Spain [email protected]
Key words: noninvasive ventilation, prolonged mechanical ventilation, chronic critical illness, weaning, respiratory failure. MATERIAL AND METHOD
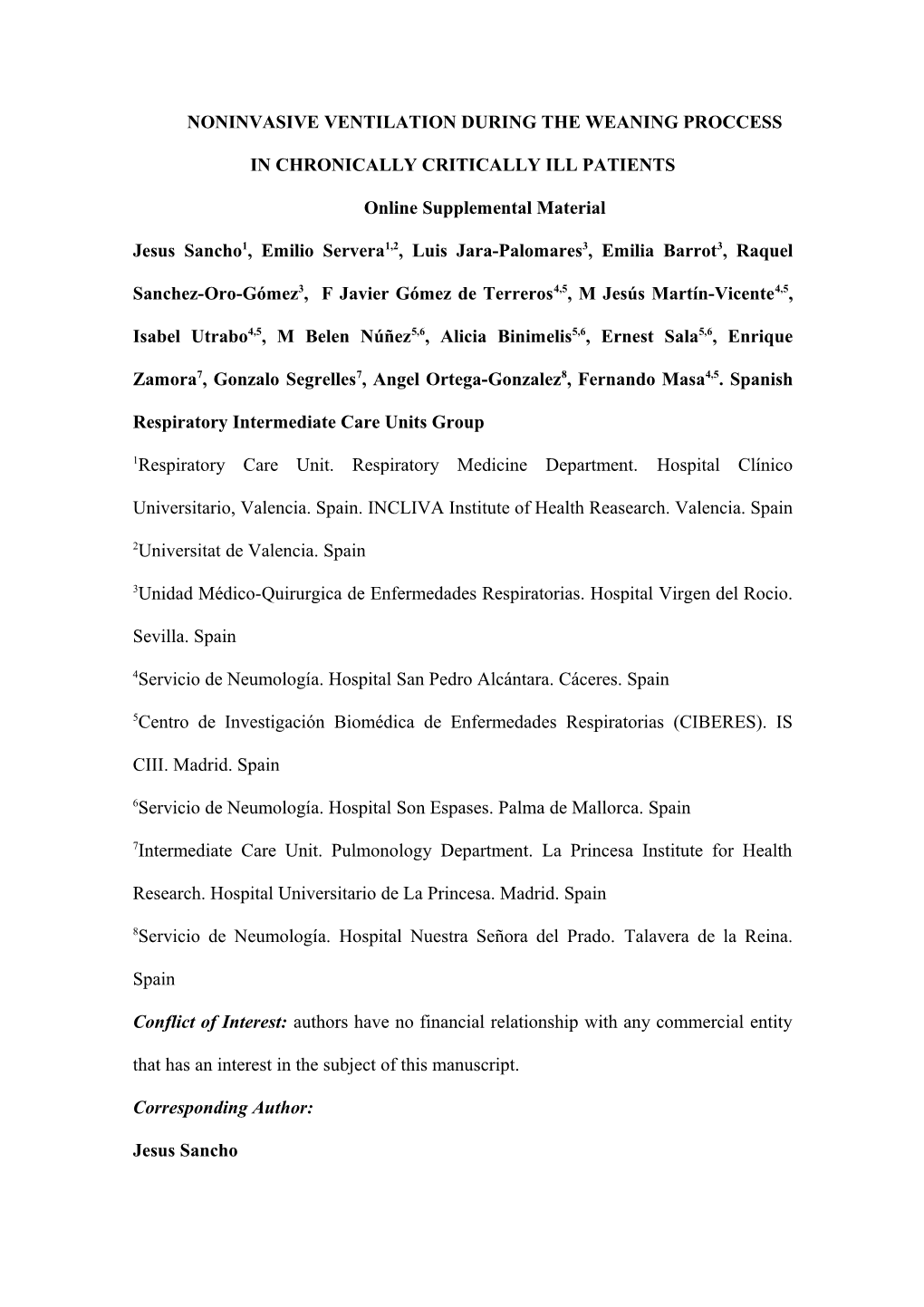
Those patients whose weaning process could not be completed due to the need for
MV during the night were transferred to NIV. The criteria for transfer to NIV were: when it proved impossible to increase the duration of SBT beyond 18 hours during 5 consecutive days.5 Two different techniques were used to effect the transfer to NIV. In some RCUs, the tracheostomy was replaced by a tracheal button and NIV was initiated; in others, NIV was applied with the tracheostomy tube having been capped, its cuff deflated, and using a fenestrated inner cannula. A tracheal button (Figure S-1) is a stoma maintenance device that fits from the skin to just inside the anterior wall of the trachea; with this device the patient breaths through the upper airway, when is capped, and when necessary a catheter can be passed through the button for secretions removal.
In both cases, NIV was applied through a nasal or oronasal mask in pressure support mode and with oxygen added if necessary. The ventilator was initially set up so as to attain a tidal volume of about 8-10 mL/Kg. The back-up respiratory rate was set at 12 to
16 bpm and the inspiratory trigger sensitivity at –1 cmH2O. The ventilatory parameters were then readjusted in order to achieve effective ventilation (PaCO2 <45mmHg and time spent with SpO2 below 90% at night using NIV <5%). Once NIV was tolerated by the patient and effective ventilation had been achieved the tracheal button or tracheostomy tube was removed and the tracheostomy was closed.
RESULTS
In 24 patients a capped tracheostomy tube was used to transfer to NIV and in 16 a tracheal button; no statistical differences were found between the two groups in hospital mortality (8.33% vs 6.25%, p=0.760), stay at RCU (34.43+19.81 vs 56.64+43.81 days, p=0.096) and time from NIV initiation to tracheostomy closure (1.42+1.13 vs 2.30+2.18 days, p=0.307). (Table E1, E2) Legends:
Figure S-1: Tracheal button Tracheal button Capped tracheostomy p n=16 tube n=24 Gender (Male/Female) 8/8 13/19 0.265 Age (years) 67.53+12.04 63.60+15.47 0.972 Cause of Critical illness 11/5 19/5 0.549 (medical/surgical) Charlson Index 1.73+1.22 2.09+1.30 0.087 APACHE II 15.00+3.27 13.11+2.80 0.164 Intensive care stay 43.54+22.46 38.57+20.63 0.643 (days) MV in intensive care 34.81+18.45 35.96+20.69 0.606 (days) Weaning time at RCU 31.33+18.93 43.00+21.73 0.087 (days) pH 7.39+0.04 7.39+0.08 0.972 PaO2 (mmHg) 105.50+28.33 78.28+19.64 0.006 PaCO2 (mmHg) 49.50+0.04 53.60+7.09 0.288 FiO2 0.36+0.07 0.39+0.09 0.413 Leukocytes (per L) 10034.66+2878.06 9810.00+3832.71 0.850 Neutrophils (%) 72.54+12.74 71.75+11.12 0.886 Hemoglobin (g/dL) 9.38+1.54 10.27+1.60 0.205 Hematocrit (%) 28.13+4.92 30.87+5.33 0.230 Platelets (per L) 300600.00+15800.00 234000.00+76967.52 0.278 Sodium (mmol/L) 138.53+6.61 140.62+4.90 0.442 Potassium (mmol/L) 4.08+0.39 4.17+0.77 0.718 Blood urea nitrogen 53.53+40.99 75.25+35.06 0.375 (mg/dL) Creatinine (mg/dL) 0.91+0.85 0.87+0.69 0.908 Serum albumin (g/dL) 3.06+0.69 3.30+0.51 0.347 C-reactive protein 45.66+44.21 22.31+20.80 0.175 (mg/L)
Table E-1
Demographic and clinical data at RCU admission
of the CCI patients who need NIV during weaning process.
APACHE: Acute Physiology and Chronic Health Evaluation; CCI: Chronically critically Ill; MV: Mechanical ventilation; NIV: Noninvasive ventilation; RCU:
Respiratory Care Unit
Tracheal button Capped tracheostomy tube p n=15 n=22 pH 7.42+0.04 7.43+0.03 0.701 PaO2 (mmHg) 80.46+19.98 71.90+10.47 0.209 PaCO2 (mmHg) 41.60+4.32 44.72+6.92 0.169 FiO2 0.21+0.1 0.21+0.01 0.880
Table E-2
Arterial Blood Gases at Hospital discharge of the Chronically CritilalIy Ill patients
who need noninvasive ventilation to achieve weaning success.