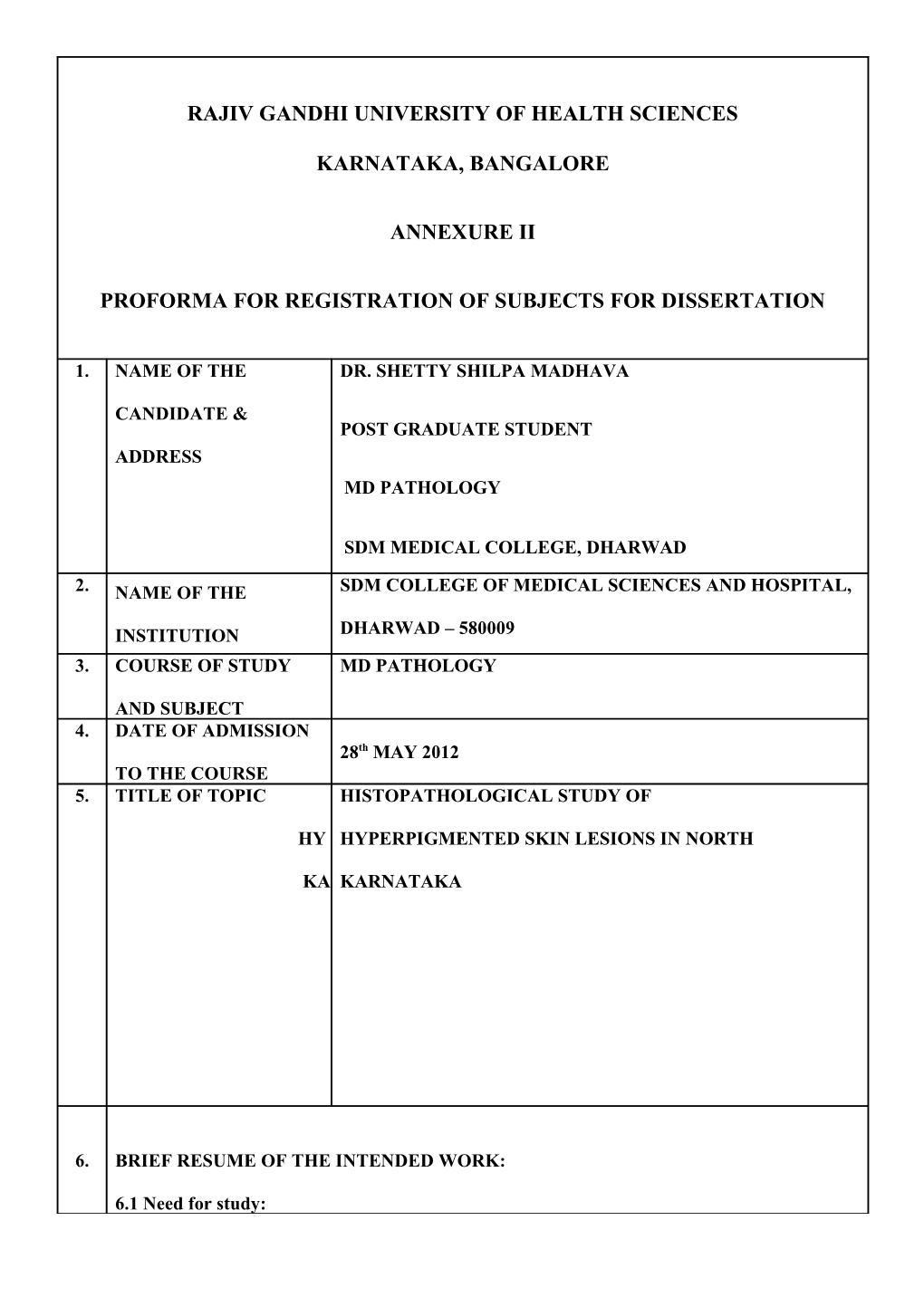
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
KARNATAKA, BANGALORE
ANNEXURE II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. NAME OF THE DR. SHETTY SHILPA MADHAVA
CANDIDATE & POST GRADUATE STUDENT ADDRESS MD PATHOLOGY
SDM MEDICAL COLLEGE, DHARWAD
2. NAME OF THE SDM COLLEGE OF MEDICAL SCIENCES AND HOSPITAL,
INSTITUTION DHARWAD – 580009 3. COURSE OF STUDY MD PATHOLOGY
AND SUBJECT 4. DATE OF ADMISSION 28th MAY 2012 TO THE COURSE 5. TITLE OF TOPIC HISTOPATHOLOGICAL STUDY OF
HY HYPERPIGMENTED SKIN LESIONS IN NORTH
KA KARNATAKA
6. BRIEF RESUME OF THE INTENDED WORK:
6.1 Need for study: Hyperpigmentary skin disorders may be defined as increased pigmentation of the skin and/or mucus membranes.1 Hyperpigmentation may be caused by abnormality in dermis or epidermis.
Hyperpigmentation, whether regional or generalized, is the result of stimulation of melanocytes by a variety of stimuli, such as sunlight, heat, drugs, hormones (as in pregnancy), dietary deficiency (as in Kwashiorkar), metabolic disorders (such as Gaucher disease), scars, and a variety of dermatoses (generically referred to as post inflammatory hyperpigmentation).2
In the US, malignant melanoma accounts for more than 85% of all skin cancer deaths.3 In
Caucasians, the most common complaints about photoaged skin are fine wrinkles and telangiectasia. In Asians, hyperpigmentation is the most common cosmetic complaint.4
In Indian scenario, acquired hyperpigmentation is difficult to diagnose and more difficult to treat satisfactorily. There is paucity of literature regarding the clinico-histopathological study of hyperpigmentary skin disorders in North Karnataka. This area being the tropical part of the country, people have to face intense summers, thus because of increased exposure to sun and sweating, people are predisposed to hyperpigmentation and fungal infection.
The incidence of histopathological study in hyperpigmented skin lesions are comparatively less in this part of Karnataka.
6.2 REVIEW OF LITERATURE:
Hyperpigmentary skin disorders may be broadly classified into two groups, epidermal which is characterized by ‘brown hyperpigmentation’ and dermal which is known as ‘blue hyperpigmentation’ or ‘ceruloderma’.1
Kurita M et al, classified hyperpigmented lesions into seven categories based on pathological features, especially on the degree of hyperkeratosis and epidermal melanin deposits, and on the existence of melanin incontinence and the location of dermal melanocytes. Histopathology report revealed, epidermal pigmentation was the commonest finding followed by dermal pigmentation and hyperkeratosis in the epidermis. The histology based treatment principles may be helpful for establishing a standardized treatment algorithm for hyperpigmented skin lesions.4
Plensdorf S et al , states that common hyperpigmentation disorders include post-inflammatory hyperpigmentation, melasma, solar lentigines, ephelides and Café-au-lait macules. Fitzpatrick system was used to divide skin type into 6 categories ( type I – VI).5
According to Stulberg D et al, a localized hyperpigmented or irregularly pigmented lesion that is new in onset, arises within a congenital nevus, or causes pain or itching could be a malignant melanoma. When possible, suspicious lesions should be excised totally for pathologic evaluation.
If size or location precludes complete excision, incisional biopsy is performed( usually punch biopsy).6
Edwards V et al, studied that pigmented skin lesions comprise a large component of most histopathologist’s work load. Therefore, it is important to approach all melanocytic and pigmented lesions in a consistent manner. Age of the patient, anatomical location of the lesion, site of biopsy are the important factors to be considered. Various lesions described fall into following categories – non melanocytic lesions that can mimic melanocytic lesions, benign melanocytic lesions that can mimic melanoma, malignant melanoma that can mimic benign lesions, epidermotrophic metastatic melanoma that can mimic primary melanoma or naevi, atypical melanocytic lesions that are difficult to categorize. These wide spectrum of histological appearances of melanocytic lesions should be interpretated after considering the clinical features.7
Davis E C et al, mentions that acne vulgaris, atopic dermatitis and impetigo are the very common causes of post-inflammatory hyperpigmentation which worsens with UV irradiation and persistent or recurrent infection. Melanocyte stimulating properties of Leukotrienes(LT –C4,D4);
Prostaglandins E2,D2; thromboxane 2; Interleukin 1,6; Tumor necrosis factor α, Epidermal growth factor and Nitric oxide play a role in the pathogenesis.8
Kanwar A J et al, in his study on 124 patients has shown that Lichen planus pigmentosus was commonly seen among Indians. Commonest site involved was face and neck with female preponderance. Pattern of pigmentation most commonly seen was diffuse(77.4%) followed by reticular(9.7%) and blotchy(7.3%). Histopathological study revealed hyperkeratosis, thinning of the epidermis, basal cell degeneration, perivascular infiltrate, melanophages and band like infiltrate in the upper dermis.9 According to Sarvjot V et al, following a study on 43 cases, melasma is more common in females than in males and epidermal type(48.8%) was more common than dermal type(34.8%). Solar elastosis was the single most common histological finding(55.8%) apart from increased melanin concentration, epidermal flattening and dermal lymphomononuclear inflammation.10
Lee H Y et al, had studied cutaneous melanoma on 48 cases retrospectively, and found that it was the most common cause of mortality amongst skin cancer in Caucasian population whereas the incidence of cutaneous melanoma in Asians was lower. Age range was 29years – 95years with male:female ratio of 1.3:1. Commonest site involved was palms and soles. Commonest histological subtype was acral lentiginous melanoma(50%). All patients had received surgical excision as the primary form of therapy. Mean duration to diagnosis of acral lentiginous melanoma was an average of 27months as compared to 12months in other histological subtypes.
Thus, a significant delay in diagnosis of melanoma was noted particularly in Asians which highlights the need for adapted education programmes.11
Tadiparthi S et al, studied that incidence of skin malignancy is increasing world-wide and excision biopsy plays an important role to diagnose, stage and to determine treatment and prognosis of malignant melanoma. In their study, age group of the patients was 18-91 years, commonest presenting complaint being hyperpigmentation and punch biopsy was commonly performed. The study states that incisional biopsy is not fully accessible for histological assessment and other biopsies like punch, shave and curettage are not recommended.12
Sina B et al, has mentioned in his study in order to render an accurate histopathological diagnosis, skin biopsies must contain adequate specimen to include the three basic components of the skin, i.e. epidermis, dermis and subcutaneous tissue. It is essential to select a representative area of the lesion devoid of artifact, with proper fixation in adequate fixative and prompt transport of the specimen to the histology laboratory.13
6.3 Objectives of study:
1.It is a prospective and retrospective, histopathological study of hyperpigmented skin lesions.
2.To assess age wise, sex wise, site wise, size wise and location wise distribution of various hyperpigmented skin lesions.
2.To draw necessary conclusions and compare the results with those available in the literature.
7. MATERIALS AND METHODS:
7.1 Source of data:
Patients with hyperpigmented skin lesions in all age groups attending the department of
Dermatology, in whom skin biopsy has been taken and is received by Pathology department at
SDM College of Medical Sciences and Hospital, Dharwad. The skin biopsy specimen of
Hyperpigmented skin lesions sent by Department of Dermatology and received by Department of
Pathology in our institution is in a range of 15-20 per year. Study will be done on the basis of
percentage of distribution of hyperpigmented skin lesions in this part of North Karnataka.
7.2 Methods of collection of data:
Period of study is between June 1st 2009 - June 1st 2014, being 3 years retrospective and 2
years prospective study.
Study will be done on approximately 75 cases.
1.For retrospective study, details of patients with hyperpigmented skin lesions will be
retrieved from old records following which slides and blocks will be collected for review.
2. For prospective study, the biopsy would be taken by the Dermatologist and it will be fixed
in formalin and taken through paraffin processing followed by routine hematoxylin and eosin
staining. Special stains would be used wherever necessary.
Masson Fontana stain for melanin to know dermal and epidermal hyperpigmentation.
3. Detailed Histopathological examination of the samples will be conducted and lesions will
be assessed based on age wise, sex wise, site wise, size wise and location wise distribution
following which, the data will be compared with available literature.
Inclusion Criteria: Hyperpigmentary lesions like developmental, inflammatory, infectious,
metabolic, endocrine and neoplastic lesions.
Exclusion Criteria: Hyperpigmentary lesions like genetic lesions and hypopigmented lesions
are excluded from the study.
7.3 Does the study require any investigation to be conducted on patients or animals? If so
please describe briefly.
No.
7.4 Has ethical clearances been obtained from ethical committee of your institution in
case of 7.3?
Yes, ethical clearance has been obtained from SDM institutional ethical committee, SDM
medical college, Dharwad.
8. LIST OF REFERENCES:
1.Dutta A K, Datta P K, Dhar S. Hyperpigmentary Disorders. In Valia R G, Valia A R. IADVL
Textbook and Atlas of Dermatology vol.1, 2nd edition. Mumbai:Bhalani; 2003. p.760.
2. Rosai J. Dermatoses, Tumors and tumorlike conditions. Rosai and Ackerman’s Surgical
Pathology vol.1, 10th edition. Missouri:Elsevier; 2011. p.171.
3.Costin G E, Hearing V J. Human skin pigmentation: melanocytes modulate skin color in
response to stress. FASEB J. 2007;21:976-994.
4. Kurita M, Kato H, Yoshimura K. A therapeutic strategy based on histological assessment of hyperpigmented skin lesions in Asians. Journal of Plastic, Reconstructive and Aesthetic Surgery
2009;62:955-963.
5. Plensdorf S, Martinez J. Common Pigmentation Disorders. Am Fam Physician 2009;79(2):109-
116.
6.Stulberg D L, Clark N, Tovey D. Common Hyperpigmentation Disorders in Adults:Part II.
Melanoma, Seborrheic Keratoses, Acanthosis Nigricans, Melasma, Diabetic Dermopathy, Tinea
Versicolor and Postinflammatory Hyperpigmentation. Am Fam Physician 2003;68:1963-8.
7.Edwards S L, Blessing K. Problematic pigmented lesions:approach to diagnosis. J Clin Pathol
2000;53:409-418.
8. Davis E C, Callender V D. Postinflammatory Hyperpigmentation A review of the
Epidemiology, Clinical Features and Treatment Options in Skin of Color. J Clin Aesthetic
Dermatol 2010;3(7):20-31.
9. Kanwar A J, Dogra S, Handa S, Parsad D, Radotrat B D. A study of 124 Indian patients with
lichen planus pigmentosus. Clinical and Experimental Dermatology 2003;28:481-485.
10. Sarvjot V, Sharma S, Mishra S, Singh A. Melasma:A clinicopathological study of 43 cases.
Indian Journal of Pathology and Microbiology 2009;52(3):357-359.
11. .Lee H Y, Chay W Y, Tang M B, Chio M T, Tan S H. Melanoma:Differences between Asian
and Caucasian Patients. Ann Acad Med Singapore 2012;41:17-20.
12. Tadiparthi S, Panchani S, Iqbal A. Biopsy for malignant melanoma-are we following the
guidelines? Ann R Coll Surg Engl 2008;90:322-325.
13. Sina B, Kao G F, Deng A C, Gaspari A A. Skin biopsy for inflammatory and common
neoplastic skin diseases:optimum time, best location and preferred techniques.A critical review. J
Cutan Pathol 2009;36:505-510.
9. Signature of the candidate
10. Remarks of the Guide This study will help in assessing the clinical and histopathological findings in hyperpigmented skin lesions. SDM College of Medical Sciences and Hospital , being a tertiary care hospital, all hyperpigmented lesions of skin alongwith clinical findings are submitted for the biopsy. This study will help the clinicians as well as histopathologists to know various entities available in this part of Karnataka.
11. NAME & DESIGNATION DR. VIDISHA S. ATHANIKAR MD 11.1 GUIDE PROFESSOR, DEPARTMENT OF PATHOLOGY, SDMCMSH, DHARWAD.
11.2 SIGNATURE
11.3 CO-GUIDE
11.4 SIGNATURE
11.5 HEAD OF THE DEPARTMENT DR. RAVIKALA RAO MD PROFESSOR & HEAD, DEPARTMENT OF PATHOLOGY, SDMCMSH, DHARWAD.
11.6 SIGNATURE
12. 12.1 REMARKS OF CHAIRMAN AND PRINCIPAL 12.2 SIGNATURE