PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY / PROCEDURE
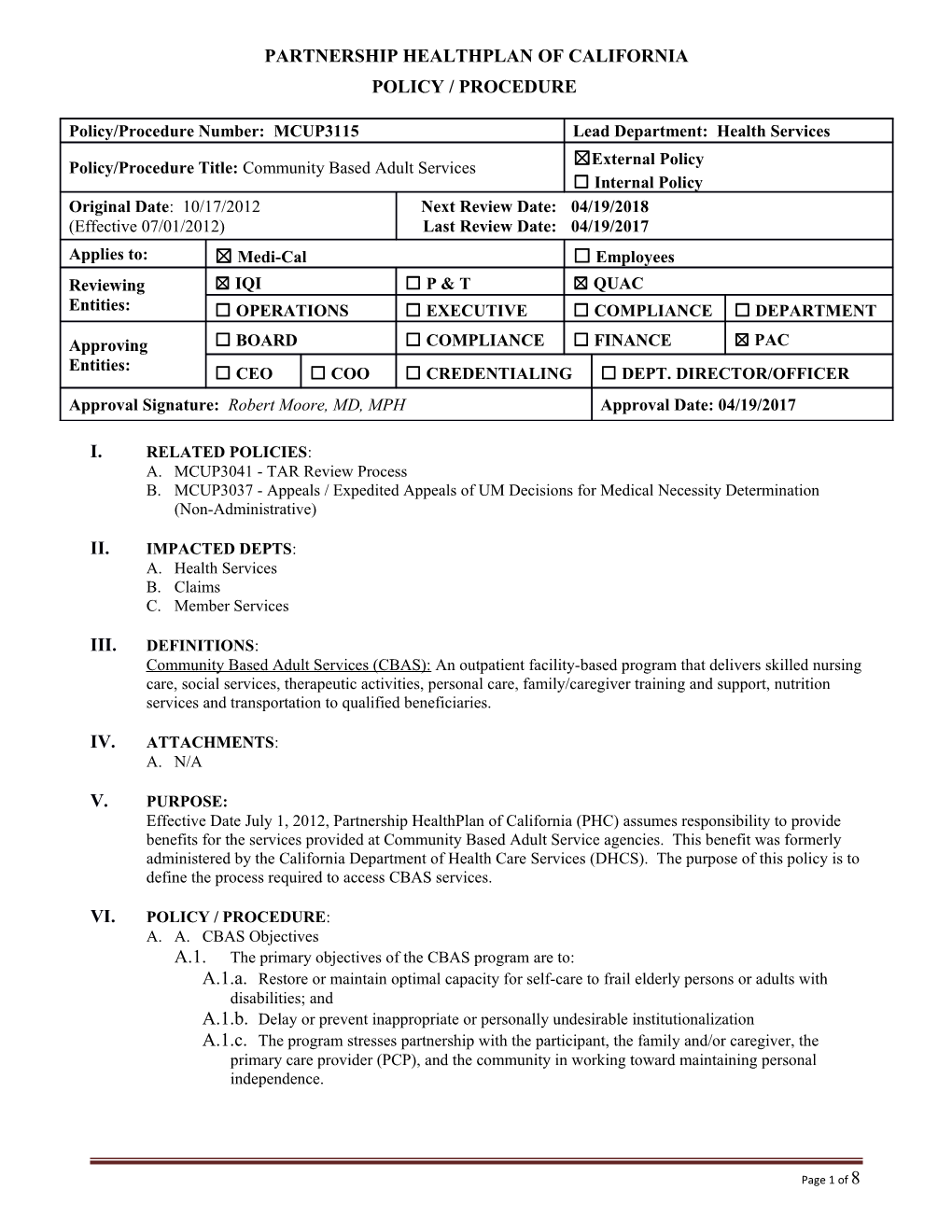
Policy/Procedure Number: MCUP3115 Lead Department: Health Services ☒External Policy Policy/Procedure Title: Community Based Adult Services ☐ Internal Policy Original Date: 10/17/2012 Next Review Date: 04/19/2018 (Effective 07/01/2012) Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees Reviewing ☒ IQI ☐ P & T ☒ QUAC Entities: ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT
Approving ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC Entities: ☐ CEO ☐ COO ☐ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approval Signature: Robert Moore, MD, MPH Approval Date: 04/19/2017
I. RELATED POLICIES: A. MCUP3041 - TAR Review Process B. MCUP3037 - Appeals / Expedited Appeals of UM Decisions for Medical Necessity Determination (Non-Administrative)
II. IMPACTED DEPTS: A. Health Services B. Claims C. Member Services
III. DEFINITIONS: Community Based Adult Services (CBAS): An outpatient facility-based program that delivers skilled nursing care, social services, therapeutic activities, personal care, family/caregiver training and support, nutrition services and transportation to qualified beneficiaries.
IV. ATTACHMENTS: A. N/A
V. PURPOSE: Effective Date July 1, 2012, Partnership HealthPlan of California (PHC) assumes responsibility to provide benefits for the services provided at Community Based Adult Service agencies. This benefit was formerly administered by the California Department of Health Care Services (DHCS). The purpose of this policy is to define the process required to access CBAS services.
VI. POLICY / PROCEDURE: A. A. CBAS Objectives A.1. The primary objectives of the CBAS program are to: A.1.a. Restore or maintain optimal capacity for self-care to frail elderly persons or adults with disabilities; and A.1.b. Delay or prevent inappropriate or personally undesirable institutionalization A.1.c. The program stresses partnership with the participant, the family and/or caregiver, the primary care provider (PCP), and the community in working toward maintaining personal independence.
Page 1 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees B. Eligibility Criteria B.1. To be eligible for CBAS services through Partnership HealthPlan of California, the person must be at least 18 years of age. They must be an eligible member of PHC’s Medi-Cal program. B.2. The member must also meet all the following criteria: B.2.a. Must have one or more chronic or post-acute medical, cognitive, or mental health conditions. B.2.b. A physician, nurse practitioner or other health care provider has, within his/her scope of practice, requested CBAS services for the person. B.2.c. The person requires ongoing or intermittent protective supervision, skilled observation, assessment or intervention by a skilled health provider to improve, stabilize, maintain, or minimize deterioration of the medical, cognitive or mental health condition. B.2.d. The person requires CBAS services that are individualized and planned to support the individual and his or her family or caregiver in the living arrangement of his/her choice and to avoid or delay the use of institutional services, including but not limited to, hospital services, inpatient mental health services or placement in a nursing or intermediate care facility for the developmentally disabled providing continuous nursing care. B.2.e. Any person who is a resident of an Intermediate Care Facility for the Developmentally Disabled/Habilitative (ICF/DD-H) shall be eligible for CBAS care services if that resident has disabilities and a level of functioning that are of such a nature that without supplemental intervention through CBAS care, placement to a more costly institutional level of care would likely occur. B.3. Medical Necessity Criteria B.3.a. Except for participants residing in an ICF/DD-H, authorization or reauthorization of a CBAS Treatment Authorization Request (TAR) shall be approved only if the participant meets all of the following medical criteria: B.3.a.1) The participant has one or more chronic or post-acute medical, cognitive, or mental health conditions that are identified by the participant’s personal health care provider as requiring one or more of the following, without which the participant’s condition will likely deteriorate and require emergency department visits, hospitalization or other institutionalization: B.3.a.1.a) Monitoring B.3.a.1.b) Treatment B.3.a.1.c) Intervention B.3.a.2) The participant’s network of non-adult day health care support is insufficient to maintain the individual in the community, demonstrated by at least one of the following: B.3.a.2.a) Participant lives alone and has no family or caregivers available to provide sufficient and necessary care or supervision B.3.a.2.b) Participant resides with one or more related or unrelated individuals, but they are unwilling or unable to provide sufficient and necessary care or supervision to the participant B.3.a.2.c) Participant has family or caregivers available, but those individuals require respite in order to continue providing sufficient and necessary care or supervision to the
Page 2 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees participant. B.3.a.2.d) A high potential exists for the deterioration of the Participant’s medical, cognitive, or mental health condition or conditions in a manner likely to result in emergency department visits, hospitalization, or other institutionalization if CBAS services are not provided.
Page 3 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees C. CBAS Authorization Process C.1. Initial Request: A request for initiation of CBAS services may come from one of the following sources: C.1.a. Community Based Adult Services Center C.1.b. Physician C.1.c. Nursing Facility C.1.d. Hospital C.1.e. Individual member C.1.f. Family member C.1.g. Community Based Organization C.2. To recommend a member for CBAS services, the requesting entity must contact PHC. The initial inquiry request must be submitted to PHC before any assessment or services are provided by the CBAS agency, and prior to submission of a Treatment Authorization Request. This inquiry may be done verbally or in writing. The following information should be included at the time of the request: C.2.a. Member’s Name C.2.b. Identification Number C.2.c. Date of Birth C.2.d. Contact Information of member, caregiver and referring agent. (Name, address, phone number) C.2.e. Reason the member needs CBAS services (Specific information may vary by the requesting entity) D. CBAS Eligibility Interview D.1. Following receipt of a standard request for inquiry regarding a potential CBAS evaluation, PHC will send a written acknowledgement of the request to the requestor and the member, and within five (5) business days of the request PHC staff will make the first attempt to contact the member and/or caregiver to arrange for a face-to-face interview with the member. If initially unable to reach the member, two additional attempts will be made between five (5) and eight (8) business days of the request. D.2. If still unable to reach the member, a final attempt to schedule a face-to-face interview will be made in writing at 14 calendar days of receipt of the request. If the member does not schedule an appointment within 14 calendar days from the date of inquiry, PHC will advise the member and the requesting entity, in writing, that if the member continues to need CBAS services a new request will be required. D.3. Members who are reached will have an appointment scheduled for a face-to-face interview no more than 14 calendar days from the receipt of the initial request. This meeting will take place either at the member’s home or at the CBAS Center of the member’s choice. The face-to-face interview must be completed using the Comprehensive Evaluation Determination Tool (CEDT) within 30 days from the initial inquiry. D.4. If a nursing facility or hospital identifies a potential need for expedited CBAS services in the discharge plan and the provider submits a request to begin the CBAS assessment process, a face-to- face meeting with the member will take place within five (5) business days from the initial inquiry.
Page 4 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees Approval or denial of CBAS eligibility to conduct the Individual Care Plan assessment will be sent to the Center within one (1) business day of the decision. D.5. During the face-to-face interview with the member, the PHC Registered Nurse will complete the CEDT as provided by the Department of Health Care Services. PHC shall ensure that appropriate staff responsible for conducting, managing, and/or training for an initial assessment or reassessment of members for CBAS will receive training in the use of the CBAS assessment tool per DHCS protocols.
Page 5 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees E. TAR Submission E.1. Once PHC has approved the assessment, the CBAS agency will begin their Multi-disciplinary Team assessment process and complete the Individualized Plan of Care (IPC). When the evaluation and IPC is complete and CBAS staff determines the member to be appropriate for services, the CBAS agency must electronically submit a TAR to PHC. The TAR must include the codes and description of the services to be provided and a copy of the IPC, with anticipated level of service, as well as any other clinical documentation available (i.e. History and Physical). E.2. PHC will approve, modify or deny the requested CBAS services within five (5) business days of receipt of the TAR, in accordance with Health and Safety Code 1367.01. If the TAR is approved, the facility will be notified via copy of the authorization. E.3. If the TAR is modified or denied, a Notice of Action (NOA) letter will be sent to the member and CBAS provider. If the plan does not have sufficient information to make a determination, a pend letter requesting an additional 14 business days will be sent. If no additional requested information is received, the TAR may be denied via the Notice of Action letter. The letter will include appeal rights and responsibilities. F. Reassessment F.1. A CBAS center requests reassessment and submits a request to begin the CBAS reassessment process. F.1.a. Examples: F.1.a.1) Prior authorization end date is approaching F.1.a.2) Due to a change in level of service F.2. A TAR is created and sent to PHC with an IPC and a Level of Service recommendation. F.3. PHC receives the prior authorization request from the CBAS center, which includes a completed IPC and level of service recommendation. PHC will handle the recommendation through existing TAR process which includes: F.3.a. PHC will approve, modify or deny prior authorization request within five (5) business days, in accordance with Health and Safety Code 1367.01. F.3.b. If PHC cannot make a decision within five (5) business days, a 14-day pend letter will be sent to the member and center. F.3.c. PHC notifies the center within 24 hours of the decision. The plan notifies member within 48 hours of the decision. F.4. To deny or decrease the TAR request, the plan must conduct a face-to-face meeting with the member. F.4.a. Process must be completed in accordance with the Health and Safety Code 1367.01 and ensure timelines are met. F.5. CBAS services continue. G. CBAS Facility Selection G.1. The member may choose any CBAS Center as long as it is within the selected facility’s time and distance criteria for transportation. H. Discharge from CBAS Services H.1. PHC requires that CBAS providers complete a CBAS Discharge Plan for any member who has been determined to no longer need CBAS services. A copy of the discharge plan must be submitted
Page 6 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees to PHC for review. I. Unbundled Services I.1. If a member is determined to be eligible for CBAS services but there is no CBAS facility in the member’s service area, the member may choose to attend a CBAS facility of his or her choice. If there is no CBAS facility available, PHC will assist in arranging for those individual services that are PHC benefits and make appropriate referrals to other agencies for the unbundled services that are not PHC benefits. J. Enhanced Case Management J.1.Members who were considered members under the DHCS Darling vs Douglas litigation and were determined not to be eligible for CBAS services will continue to receive enhanced case management services as stipulated in the settlement agreement.
VII. REFERENCES: A. Welfare and Institutions Code, Sections 14525 and 14526.1 B. California Health and Safety Code Section 1367.01
VIII. DISTRIBUTION: A. PHC Department Directors B. PHC Provider Manual
IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Senior Director, Health Services
X. REVISION DATES: 08/20/14; 01/20/16; 11/16/16; 04/19/17
PREVIOUSLY APPLIED TO: N/A
***********************************
In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions:
Consistent with sound clinical principles and processes Evaluated and updated at least annually If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request
The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered
Page 7 of 8 Policy/Procedure Number: MCUP3115 Lead Department: Health Services Policy/Procedure Title: Community Based Adult Services ☒ External Policy ☐ Internal Policy Original Date: 10/17/2012
Next Review Date: 04/19/2018 Last Review Date: 04/19/2017 Applies to: ☒ Medi-Cal ☐ Employees
Page 8 of 8