Cardio 19 – Homeostasis and Thrombosis Anil Chopra
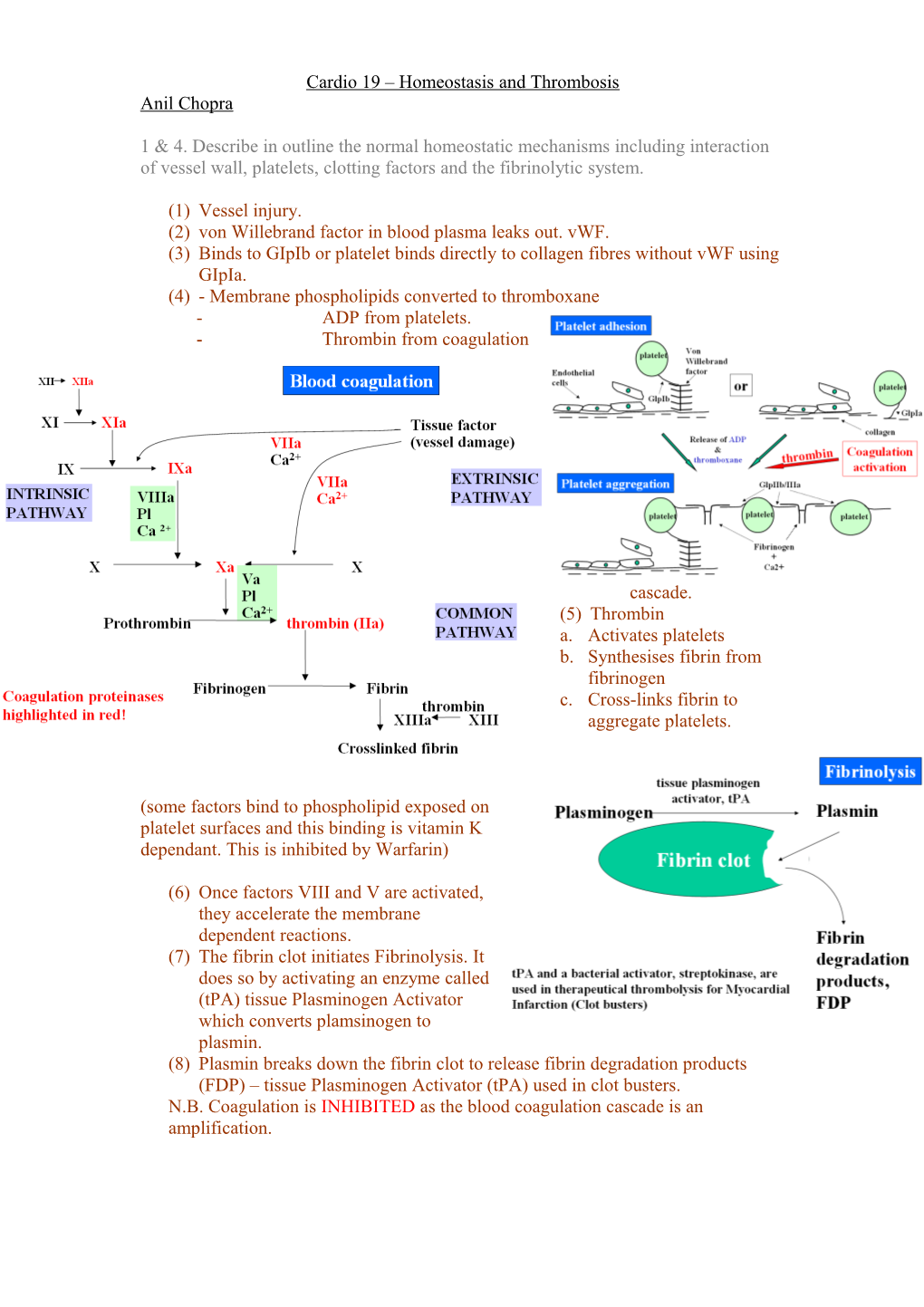
1 & 4. Describe in outline the normal homeostatic mechanisms including interaction of vessel wall, platelets, clotting factors and the fibrinolytic system.
(1) Vessel injury. (2) von Willebrand factor in blood plasma leaks out. vWF. (3) Binds to GIpIb or platelet binds directly to collagen fibres without vWF using GIpIa. (4) - Membrane phospholipids converted to thromboxane - ADP from platelets. - Thrombin from coagulation
cascade. (5) Thrombin a. Activates platelets b. Synthesises fibrin from fibrinogen c. Cross-links fibrin to aggregate platelets.
(some factors bind to phospholipid exposed on platelet surfaces and this binding is vitamin K dependant. This is inhibited by Warfarin)
(6) Once factors VIII and V are activated, they accelerate the membrane dependent reactions. (7) The fibrin clot initiates Fibrinolysis. It does so by activating an enzyme called (tPA) tissue Plasminogen Activator which converts plamsinogen to plasmin. (8) Plasmin breaks down the fibrin clot to release fibrin degradation products (FDP) – tissue Plasminogen Activator (tPA) used in clot busters. N.B. Coagulation is INHIBITED as the blood coagulation cascade is an amplification. I. Direct inhibition by antithrombin
Antithrombin is an inhibitor of coagulation factors such as Xa, XIa, IXa and thrombin. Its activity is enhanced by heparin sulphates. A drug Heparin enhances antithrombin’s actions.
II. Indirect inhibition by protein C
Thrombin binds to receptor on endothelial cell called thrombomodulin. This the activates protein C. Protein C then binds to protein S and together they inactivate factors Va and VIIIa, which downregulate thrombin production. People with factor V Leiden cannot easily deactivate it with protein C so they have increased thrombosis risk.
2 & 3. Describe the causes of bleeding disorders and the different types.
Essentially bleeding disorders are caused by increases in fibrinolytic factors and anticoagulant proteins. They can also be due to deficiency of coagulants. e.g. Haemophilia, von Willebrand disease, liver failure, autoimmune diseases, drugs (NSAIDs)
Defect in collagen, von Willebrand factor or platelets (thrombocytopenia) leads to bleeding tendancy. Symptoms include easy bruising, long (>20mins) nosebleeds, gum bleeding, menorrhagia (excessive heavy periods), small red dots. Haemophilia is deficiency in coagulation factors. o Haemophilia A factor VIII deficiency o Haemophilia B factor IX deficiency (both are sex-linked) Symptoms of Haemophilia include haemoarthrosis (bleeding into joints). In blood coagulation disorders, the platelet plug is sufficient for small vessel injury whereas in larger vessels, the plug will fall apart. Superficial cuts do not bleed due to the action of platelets, however spontaneous bleeding can occur, deep within muscles and joints. Liver failure can result in the deficiency of coagulation factors as they are synthesised in the liver. DIC - disseminated intravascular coagulation is where coagulation and Fibrinolysis are activated. They are associated with sepsis, major tissue damage and inflammation so all coagulation factors are used up. Drugs such as Warfarin are anticoagulant. The immune system can produce antibodies against coagulation factors. Excess Fibrinolysis and anticoagulant facto production is rare except when induced by drugs (tissue plasminogen activator – tPA and heparin). 5 & 6. Describe the manifestations for venous thrombosis and list risk factors. Thrombosis – increase in coagulation factors and platelets. Venous thrombosis may obstruct blood flow or embolise to the lungs. 3 factors contribute to thrombosis: 1) Blood deficiency in anticoagulant (antithrombin, protein C). increase of coagulants (Factor VIII, II, V Leiden) 2) Vessel wall proteins used for coagulation are on endothelial walks which may be affected by inflammation. 3) Flow reduced flow rate due to surgery, long flight, pregnancy. Risk of thrombosis increases with age.
7. Give a rough estimate of its prevalence. In general population = 1/1000 (over 60) = 1/10 000 (under 60) They can embolise (migrate) to lungs and form pulmonary embolism
8. Treatment of bleeding disorders and thrombosis.
Bleeding disorders: Factor replacement therapy Drugs that can inhibit Fibrinolysis such as tranexamic acid. Desmopressin acetate – releases bodies store of coagulants
Thrombosis Warfarin inhibits vitamin K and so lowers procoagulant factors. Heparin increases coagulant activity Thrombolysis (clotbusters) tPA.