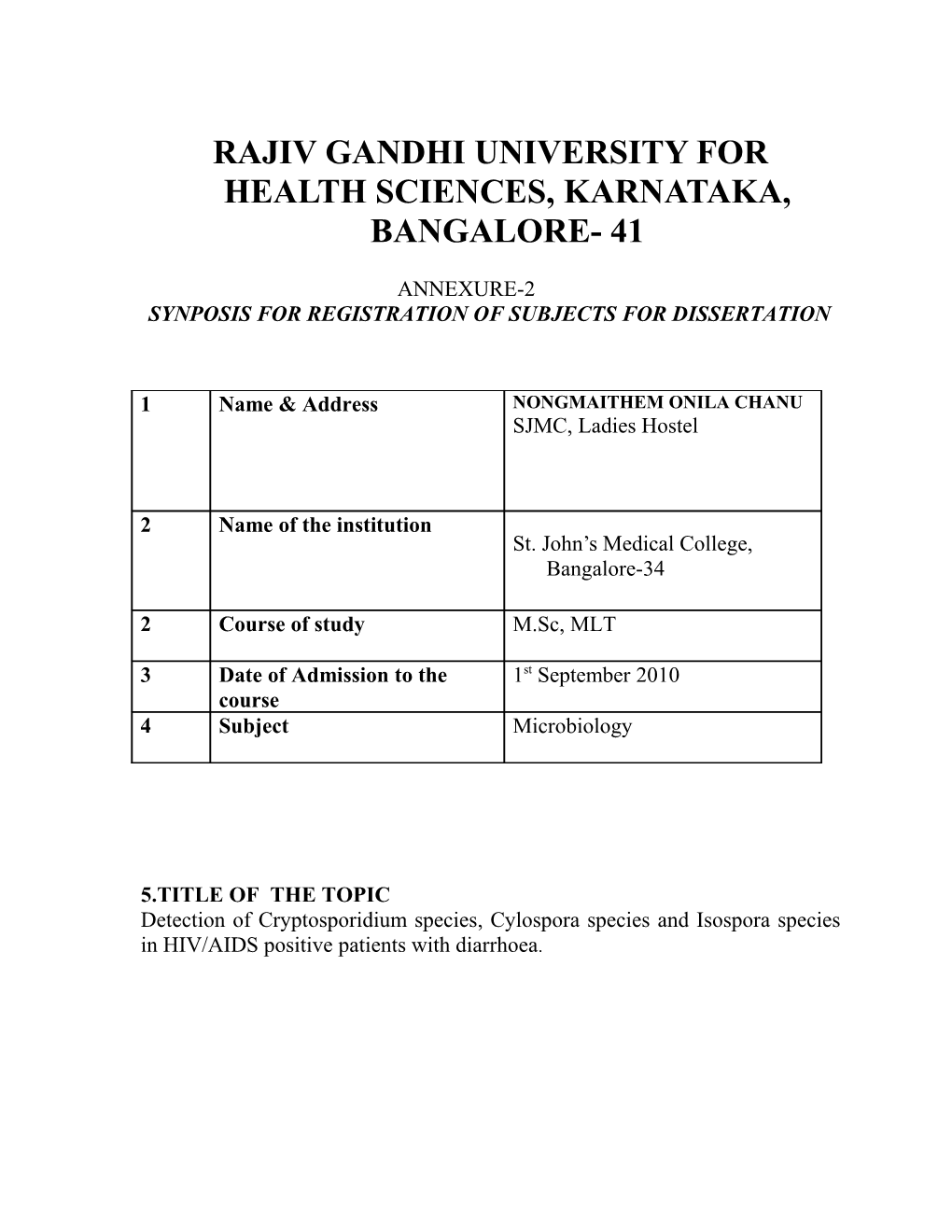
RAJIV GANDHI UNIVERSITY FOR HEALTH SCIENCES, KARNATAKA, BANGALORE- 41
ANNEXURE-2 SYNPOSIS FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1 Name & Address NONGMAITHEM ONILA CHANU SJMC, Ladies Hostel
2 Name of the institution St. John’s Medical College, Bangalore-34
2 Course of study M.Sc, MLT
3 Date of Admission to the 1st September 2010 course 4 Subject Microbiology
5.TITLE OF THE TOPIC Detection of Cryptosporidium species, Cylospora species and Isospora species in HIV/AIDS positive patients with diarrhoea. 6. BRIEF RESUME OF THE INTENDED WORK
6.1 Need For Study:
Gastrointestinal infections are very common in patients with HIV infection or AIDS. Diarrhoea is a common clinical presentation of these infections. Report indicate that diarrhoea occurs in 30-60% of AIDS Patients in developed countries and in about 90% of AIDS patients in developing countries like India.¹ Identification of the etiological agent of diarrhoea in AIDS patients is very important as it can help in timely institution of appropriate therapy and reduction of morbidity and mortality among these patients.There is need to obtain data regarding the association of parasites causing diarrhoea in HIV and AIDS patients attending St. John Medical College Hospital. St.John Medical College hospital is a 1700 bed facility. AIDS patients are admitted and managed during their illness. It is essential to provide prompt and adequate care during their illness.
6.2 REVIEW OF LITERATURE
Cryptosporidium:
Cryptosporidium is an intestinal coccidian parasite which causes infection of the small intestine. Once thought to be non-pathogenic this coccidian has been recently recognized as an important cause of diarrhoea in immunocompromised patient ³ Although cryptosporidium can be acquired at any time during the course of HIV infection, major mortality and morbidity occur almost exclusively in patient with CD4 counts below 180cells/cumm. Above this level generally spontaneous recovery occur. Infection in immunocompetent persons is usually self limited, but in person with HIV, cryptosporidiosis often results in debilitating and life-threating chronic illness.³ Cryptosporidium is a substantial threat to HIV infected individuals, who have a life-time risk of infection in around 10 percent.5
Life Cycle: Cryptosporidium completes its life cycle through the stages of asexual generation(schizogony) and sexual generation (gametogony) in a single host. All these stages of the parasites are truly intracellular and are being surrounded by a host cell membrane, which is extra-cytoplasmic.³ Man acquires infection on ingestion of food or drink contaminated with the faces, containing sporulated thick-walled oocysts of cryptosporidium.³ On ingestion, the sporozoites are released from oocysts in the small intestine. The sporozoites are slender,crescent–shaped and measure 1.5µm to 1.75µm in diameter. They invade the enterocytes in which they parasitise.
Asexual generation(schizogony):
Inside the enterocytes, the sporozoite subsequently differentiate into intracellular trophozoites. Trophozoites are the intracellular transitional form of the parasites. They are round or oval and transitional form of the parasites. They are round or oval and measure 2µm to 2.5µm in diameter. Each trophozoite consists of a large nucleus with or without a conspicuous nucleolous. These trophozoites multiply asexually by nuclear division to produce two types of meronts, type I and type II (asexual generation or schizogony). These meronts are crescent shaped and measure 1µm to 5µm in diameter showing rounded anterior and posterior ends . These type II meronts in turn produce four merozoites each, which are known as type II merozoites.
Sexual generation(gametogony):
Some of the type II merozoites invade new host cells and intiate sexual replication (sexual generation or gametogony). Inside the host cells, they differentiate either into female (macrogamont)or male(microgametocyte) forms. Each microgametocyte produces 16 sperm-like microgamets, which fertilise the macrogamont resulting in the formation of oocysts(zygote). Four sporozoites are formed inside each sporulating oocysts insitu. The sporulating oocysts are of two types, thin or thick walled. The thin-walled oocysts release the sporozoites inside the lumen of the intestine and causes auto-infection in the same host by repating the cycle of schizogony and gametogony. The thick-walled oocysts excreted in the faces are infective to other human hosts. The cysts under favourable condition remain viable and infectious relatively for a long time. These cysts, when taken up by other susceptible human hosts, cause incection and the cycle are repeated.
Cyclospora:
Cyclospora is also a coccidian parasite causes infection of the gastrointestinal tract of both the immunocompetent and immunocompromised host. The onset and course of diarrhoea vary depending on AIDS patients, diarrhoea lasts for several days to 2 weeks. It shows a waxing and waning course. The infection is self-limiting.3 The disease associated with cyclospora cayetanenses usually manifests with watery diarrhoea,vomiting and abdominal pain in immunocompromised patient for a longer duration.6,7 In AIDS patients, onset of diarrhoea is more insidious. The diarrhoea is watery and profuse and is prolonged cases can cause dehydration and loss of weight . Diarrhoea becomes chronic and oocysts are excreted in faces for an indefinite period.
Life Cycle: Human acquire infection by ingestion of water or vegetables contaminated with sporulating oocysts. In the intestine the oocysts release sporozoites, which invade enterocytes. The sporozoites, develop into unsporulated oocysts, which are excreted in faeces. The oocysts undergo sporulation outide the host before becoming infective. Other stages in the life cycle of cyclospora are not known.
Isospora:
Isospora is a coccidian parasite of the human beings, which causes infection of the gastrointestinal tract. It is an AIDS defining illness responsible for diarrhoea followed by disseminated extra-intestinal disease such as acalculous cholecystitis.
Life Cycle:
Humans acquire infection by drinking water or taking food contaminated with mature oocysts. The oocysts excyst in the small intestine and release their sporozoites. These sporozoites invade the enterocytes not the peroximal jejunum and distal duodenum and remain intracellular, inside the enterocytes, the parasites undergo asexual multiplication(shizogony) to produce merozoites be that invade new uninfected cells.
Shortly thereafter, some of these trophozoites undergoes sexual cycle(sporogony) and produce unsporulating oocysts, each containing a single sporoblast. These unsporualating oocysts are excreted in the faces and further development takes place outside the cyst.
In environmental conditions, these oocysts sporulate and mature into sporulating oocysts with two sporocysts, each containing four sporozoites. These mature cysts are the infective form of the parasite. They are resistance and are viable in the environment for months.
6.3 OBJECTIVE OF THE STUDY
1. To detect cryptosporidium species, cylospora species, Isospora species, in stool samples using modified acid fast stain in HIV/AIDS patients with diarrhoea.
2. To detect cryptosporidium species, cylospora species by rapid saffranin staining.
7. MATERIAL AND METHODS
7.1. Source of data:
Diarrhoea stool samples from the HIV patients attending St. John Medical College, Hospital from January 2011 to December 2011.
7.2. Inclusion criteria: Stool samples from HIV/AIDS patients with diarrhea attending St.John Medical College, Hospital.
7.3. Exclusion criteria: Cases of diarrhoea not associated with AIDS/HIV positive patients. Formed stools submitted from patients with AIDS/HIV. Number of isolates: 50 patient sample
7.4 Method of collection of data: Diarrhoea stool samples will be collected in a clean wide mouthed containers with tight fitting lids. All specimen will be collected prior to radiological studies using barium or the administration of bismuth, mineral oil and antidiarrhoeal medication that may interfere with the detection and identification of intestinal parasites.4
1. Macroscopic examination: The stool samples are examined for a) colour b) consistency(liquid,semi solid or formed) c) presence of muocus d) presence of visible blood .
2. Saline mount4: Method: a) Place 1 drop of 0.85% Nacl on a clean, dry 2x3 inch microscope slide. b) With an applicator stick, transfer a small amount of about 2mg of facial sample and emulsify in the saline drop. c) Place a 22x22mm coverslip over the suspension. d) Using the low power objective(10x), systematically scan the entire surface area of the coverslip for parasites. e) The high dry objective (40x) should be used for investigation of suspicious objects.
3. Iodine mount4: Method: a) Place 1 drop of Lugols iodine on a clean, dry slide. b) With an applicator stick, transfer a small amount of faecal sample and emulsify in the solution. c) A 22mm coverslip is place on the suspension. d) Using the low power objective(10x), systematically scan the entire surface area of the coverslip for parasites. e) The high dry objective (40x) should be used for investigation of suspicious objects.
4. Modified acid fast staining 4: Method: a) 1-2 drops of specimen is smeared on a slide and allowed to dry. b) Fix the smear with absolute methanol for 1 minute. c) Flood the slide with carbol fuchsin for 5-8 mins and the rinse thoroughly with water. d) Decolourise the slide with 1% HCl in ethanol until no more color runs the slide and rinsed with water and drain. e) Counterstain with 0.4% malachite green for 1 min, and rinse with water and allow to air dry. f) Examine under low or high power objective.
5. Rapid Saffranin staining4: Method: a) Faeces is smeared on a glass slide and allow to air dry at room temperature. b) The slide is then passed briefly by passing through the Bunsen burner flame. c) Fix the smear for 3-5 minutes with 2% Hcl in methanol and wash the smear with tap water. d) Stain the smear with 1% aquous saffranin for 1 minute with heating until steam appears. The slide is then rinsed with tap water. e) Counterstain with 1% methylene blue for 30 seconds.
6.Concentration technique:
Stool are concentrated by formalin-ether( Formalin-ethyl Acetate) to improve the recovery of facial specimens.4 METHODS8 a. Trasfer ¼ to ½ teaspoon of fresh stool into 10ml of 5% to 10% formalin in a 15ml shell vial, unwaxed paper cup, or 16x125mm tube( container may vary depending on individual preferences) and comminute thoroughly. Let stand for 30 minute for adequate fixation. b. Filter this material( Funnel or pointed paper cup with end cut off) thoroughly two layer of guaze into a 15 ml centrifuge tube. c. Add physiologic saline or 5% or 10% formalin to within ½ inch (1.5cm) of the top and centrifuge for 10 minutes at 500xg. d. Decant,resuspend the sediment (should have 0.5 to 1 ml sediment) in saline to within 1/2 inch (1.5cm) of the top, and centrifuge again for 10 minutes at 500xg. This second wash may be eliminated if the supernatant fluid after the first wash in light tan or clear. e. Decant and resuspend the sediment in 5% or 10% formalin. If the amount of sediment left in the bottom of the tube is very small, do not add ethyl acetate in step 6; merely add the formalin , then spin decant, and examine the remaining sediment . f. Add approximately 3ml of ethyl acetate, stopper and shake vigorously for 30 seconds. Hold the tube so that the stopper is directed away from our face, remove stopper carefully to prevent spraying of material caused by pressure within the tube. g. Centrifuge for 10 minutes at 500xg . Four layers should result, a small amount of sediment in the bottom of the tube, containing the parasites; a layer of formation; a plug of faecal debris on top of the formalin layer; and a layer of ether substitute at the top.
h. Free the plug of debris by rinsing with an applicator stick, and decant all the fluid. After proper decating, a drop or two of fluid remaining on the side of the tube will drain down to the sediment. Mix the fluid with the sediment and prepare a wet mount for examination.
7.5 Does the study require any investigations or investigations to be conducted on patients or other humans or animals? If so, please describe briefly
- No 7.6) Has ethical clearance been obtained from your in case of 7.5 - Not applicable.
Statistical analysis . This is a descriptive study. 8 . LIST OF REFERENCES:
1. Kulkarni S.V, Kairon R, Sane S.S, Padmawar P.S, Kale V.A, Thakar M.R and Risbad A.R; Oppotunistic parasitic infection in HIV/AIDS patients presenting with diarrhoea by the level of immunosuppression. Indian J Med Res 130,July 2009,pp63-66
2. Satheesh Kumar.S, Ananthan S. and Saravanan P; Role of coccidian parasites in causatation of diarrhoea in HIV infected patients in Chennai. Indian J Med Res 116,September 2002,pp 85-89
3. Dr. Subhash Chandra parija, Textbook of Medical Parasitology, Protozoolgy and Helminthology .3rd edi. 2009,pp-156-69
4. Juidith S.Hedam, Frances W. Ingersoll; Processing specimen for recovery of parasites, Essentials of Human Parasitology, COPYRIGHT@2002 by Delmar, a division of Thomson Learning .Inc
5. Farthing MJ.Clinical aspects of human cryptosporidiosis.Contrib Microbiol 2000;6:50-74
6. Pape JW. Verdier RI, Boncy M, Boncy J, Johnson WD Jr.Cyclospora infection in adults infected with HIV.Clinical manifestations , treatment and propholaxis. Ann Intern Med 1994;121:654-7
7. Sifuentes-Osnornio J, Porras-Cortes G. Bendall RP, Morales-Villarreal F, Reyes- Teran G, Ruiz, Palacoios GM. Cyclospora cayetanensis infection in patients with and without AIDS: biliary disease as another clinical manifestation. Clin Infect Dis 1995;21:1092-7
8. Forbes BA, Sahm DF, Weissfeld AS. Bailey and Scott’s diagnostic microbiology.11th ed. St. Louis: Mosby;2002.
15)Signature of the candidate
16)NAME AND DESIGNATION OF (IN BLOCK LETTERS)
17)Guide : Dr.N.S.SRIKANTH PROFESSOR OF MICROBIOLOGY SJMC, BANGALORE- 560034
17.1)Signature :
Remarks of guide :
17.2)Co- Guide(if any ) :
17.3)Signature :
17.4)Head of Department : Dr.MURALIDHARAN S. MD
17.5)Signature :
17.6)Remarks of the Chairman And Principal :
17.7)Signature