PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY/ PROCEDURE
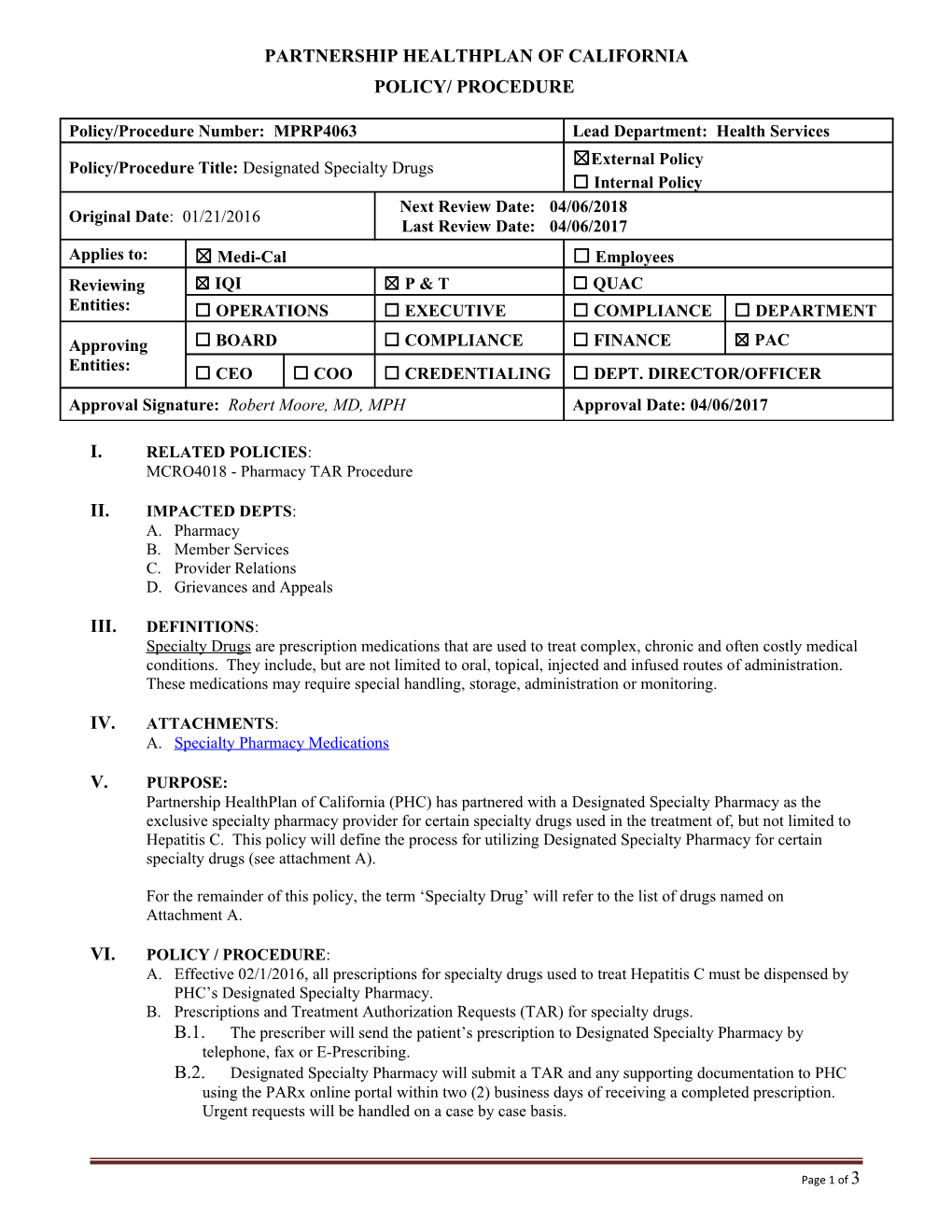
Policy/Procedure Number: MPRP4063 Lead Department: Health Services ☒External Policy Policy/Procedure Title: Designated Specialty Drugs ☐ Internal Policy Next Review Date: 04/06/2018 Original Date: 01/21/2016 Last Review Date: 04/06/2017 Applies to: ☒ Medi-Cal ☐ Employees Reviewing ☒ IQI ☒ P & T ☐ QUAC Entities: ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT
Approving ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC Entities: ☐ CEO ☐ COO ☐ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approval Signature: Robert Moore, MD, MPH Approval Date: 04/06/2017
I. RELATED POLICIES: MCRO4018 - Pharmacy TAR Procedure
II. IMPACTED DEPTS: A. Pharmacy B. Member Services C. Provider Relations D. Grievances and Appeals
III. DEFINITIONS: Specialty Drugs are prescription medications that are used to treat complex, chronic and often costly medical conditions. They include, but are not limited to oral, topical, injected and infused routes of administration. These medications may require special handling, storage, administration or monitoring.
IV. ATTACHMENTS: A. Specialty Pharmacy Medications
V. PURPOSE: Partnership HealthPlan of California (PHC) has partnered with a Designated Specialty Pharmacy as the exclusive specialty pharmacy provider for certain specialty drugs used in the treatment of, but not limited to Hepatitis C. This policy will define the process for utilizing Designated Specialty Pharmacy for certain specialty drugs (see attachment A).
For the remainder of this policy, the term ‘Specialty Drug’ will refer to the list of drugs named on Attachment A.
VI. POLICY / PROCEDURE: A. Effective 02/1/2016, all prescriptions for specialty drugs used to treat Hepatitis C must be dispensed by PHC’s Designated Specialty Pharmacy. B. Prescriptions and Treatment Authorization Requests (TAR) for specialty drugs. B.1. The prescriber will send the patient’s prescription to Designated Specialty Pharmacy by telephone, fax or E-Prescribing. B.2. Designated Specialty Pharmacy will submit a TAR and any supporting documentation to PHC using the PARx online portal within two (2) business days of receiving a completed prescription. Urgent requests will be handled on a case by case basis.
Page 1 of 3 Policy/Procedure Number: MPRP4063 Lead Department: Health Services Policy/Procedure Title: Designated Specialty Drugs ☒ External Policy ☐ Internal Policy Original Date: 01/21/2016 Next Review Date: 04/06/2018 Last Review Date: 04/06/2017 Applies to: ☒ Medi-Cal ☐ Employees B.3. TARs requiring additional documentation prior to submission: B.3.a. Designated Specialty Pharmacy will make three (3) attempts to contact the prescriber within one (1) week. If additional documentation is not provided, Designated Specialty Pharmacy will submit the TAR to PHC. B.3.b. PHC will make a determination based on the information submitted with the TAR and/or attempt to contact the prescriber for the additional documentation. B.4. Determination and provider notification by telephone or other telecommunication device of PHC determination will be made within twenty-four (24) hours of receiving a completed TAR. B.5. Determination and provider notification of PHC determinations for urgent TARs will be made within twenty-four (24) hours from the date and time the TAR is received. The Plan will make every effort to provide determination and both provider and member notification for urgent TARs, if the TAR is received by 3:00 PM on a Plan business day. All TARs received by PHC designated as urgent by the submitting provider are subject to review to determine if the TAR should be processed as urgent. B.6. Determination and member notification of PHC determinations, which includes the reason for the denial, modification or deferral to the requesting provider and information about the appeals process, is made within twenty-four (24) hours of the following TAR actions: B.6.a. A denied TAR that lacks medical justification for the intended use of the drug. B.6.b. A denied TAR in which insufficient information was submitted on the TAR. B.6.c. A denied TAR in which additional requested information was not received by PHC within 14 calendar days of the initial TAR. B.6.d. A denied TAR in which the requested drug is a Carve-out drug (member notification is administrative and not a determination of medical necessity). B.6.e. A denied TAR in which the member has other primary insurance (member notification is administrative and not a determination of medical necessity). B.6.f. A modified TAR B.6.g. A deferred TAR C. Designated Specialty Pharmacy will not be exclusive for adjunctive therapy medications, but can fill adjunctive therapy medications as a convenience to the member. D. If Designated Specialty Pharmacy is unable to dispense a specialty drug due to an emergency, the alternate Designated Specialty Pharmacy or other alternative pharmacy may dispense the specialty drug with prior approval by PHC.
VII. REFERENCES: N/A
VIII. DISTRIBUTION: A. PHC Provider Manual, B. PHC Department Directors
IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Associate Director, Pharmacy Operations
Page 2 of 3 Policy/Procedure Number: MPRP4063 Lead Department: Health Services Policy/Procedure Title: Designated Specialty Drugs ☒ External Policy ☐ Internal Policy Original Date: 01/21/2016 Next Review Date: 04/06/2018 Last Review Date: 04/06/2017 Applies to: ☒ Medi-Cal ☐ Employees X. REVISION DATES: 01/12/17; 04/06/17
PREVIOUSLY APPLIED TO: Healthy Kids 01/21/2016 to 12:01/2016 (Healthy Kids program ended 12/01/2016)
XI. POLICY DISCLAIMER: A. In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: A.1. Consistent with sound clinical principles and processes; A.2. Evaluated and updated at least annually; A.3. If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request. B. The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC.
Page 3 of 3