P.H.D. Thesis XXVIII Cicle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Table of Contents
A periodic pubblication from the Italian Trade Volume 12 Issue1 .it italian trade 1 Table of contents 22. CREDITS EDITORIALS 24. “Italy and Miami: a long lasting bond of friendship”: a message from Tomas Regalado, Mayor of the City of Miami 26. “The US Southeast, a thriving market for Italian companies”: a message from Gloria Bellelli, Consul General of Italy in Miami 28. “The United States of America, a strategic market for Italian food industry”: a message from Gian Domenico Auricchio, President of Assocamerestero 30. “25 years supporting Italy and its businesses”: a message from Gianluca Fontani, President of Italy-America Chamber of Commerce Southeast SPECIAL EDITORIAL CONTRIBUTIONS 32. “Andrea Bocelli, when simplicity makes you the greatest”, interview with Andrea Bocelli, Italian classical crossover tenor, recording artist, and singer-songwriter. 40. “Santo Versace, Style is the Man!”, interview with Santo Versace, President of Gianni Versace Spa 47. “Italians in Miami: a unique-of-its-kind community”, by Antonietta Di Pietro Italian Instructor in the Department of Modern Languages at Florida International University 53. “Italy and the US: a strong relationship” by Andrea Mancia e Simone Bressan, Journalists and Bloggers THE “MADE IN ITALY AMBASSADOR AWARD” WINNERS 58. “Buccellati, a matter of generations”, interview with Andrea Buccellati, President and Creative Director of Buccellati Spa 63. “The Made in Italy essence” interview with Dario Snaidero, CEO of Snaidero USA INTRODUCING “THE BEST OF ITALY GALA NIGHT” 69. “The Best of Italy Gala Night” Program THE PROTAGONISTS OF “THE BEST OF ITALY GALA NIGHT” 76. “Alfa Romeo, Return of a legend”, by Alfa Romeo 82. -

Goran BREGOVIC's KARMEN with a Happy End a Gypsy Opera Played
Goran BREGOVIC’s KARMEN with a Happy End A gypsy opera played and sung by Goran Bregovic and his Wedding and Funeral Band for KAMARAD production libretto & music: Goran Bregovic script co-writer and all the best ideas: Mirjana Bobic Mojsilovic orchestration: Nino Ademovic programming & sound: Dusan Vasic Slave Celevski Nikola Vukovic Sasa Jaksic - Zika Translations into Roma Ljuan Koka Translation into English Maria Rankov Recorded and mixed in KAMARAD Studios, Belgrade Mastering in METROPOLIS Studios, London * * * * CHARACTERS Vaska Jankovska: KLEOPATRA - A beautiful gypsy with a band-aid on her fore-arm who tells fortune in a tv show. Engages in a telephone seduction-game with BAKIA, passing herself off for Nena, a strip- tease girl. In the opera she plays the late Karmen. Bokan Stankovic: BAKIA - Street-sweeper, a trumpet player. In the opera he plays his own uncle, the late Fuad Kostic. Milos Mihajlovic: MILOS - Baritone player in Fuad’s orchestra. Dejan Manigodic: Deki - Tuba player in Fuad’s orchestra, he now circumcises Stojan Dimov: Stole - Sax player in Fuad’s orchestra Dalibor Lukic: trumpet player - In the opera he plays Captain EMILIO, leader of a police brass band. Alen Ademovic: Alen - Traditional drums payer in Fuad’s orchestra. In the opera he plays CEausesCu, the pimp Aleksandar Rajkovic: ACA - Baritone, gipsy street musicians Goran Bregovic: BREGA - Snare-drum player in Fuad’s orchestra, now receptionist in a hotel at the Central Station Ludmila Radkova-Trajkova: MICHAELA, Emilio’s fiance who plays accordion - In the opera she plays a worker from the Tobacco Factory, a prostitute Daniela Radkova-Aleksandrova: SINGER - in the opera she plays a worker from the Tobacco Factory, and a prostitute KLEOPATRA: Here I am. -

Author Index
JACC February 1994:487A-522A 487A Author Index Aarhus. Lawrence L. 868-127. 94A. 743-4. 173A. Akasaka. Takashi 912-46. 248A. 909-55. 241A. Amlie. Jan Peder 863-87. 83A 746-5. 177A. 903-95. 213A. 784-4. 339A. 957-14.410A. 957-15. 410A. 828-1 .468A Ammon. Susan 937-82. 331A 784-6. 339A Akashi. Katsuya 707-3. 14A Amodaj. Nenad 990-1. 3A Aarons. Diana 899-70. 204A Akhtar. Masood 509. Ix. 222. xvii. 913-113. 249A. Anagnos. Peter C. 894-11 • 193A Aass. Halfdan 863-87. 83A 766-3.276A. 947-77. 367A, 947-78. 367A. Anastasakis. Aris 725-6. UIA Abascal. Vivian M. 894-17. 194A 961-108.421A Anayiotos. Andreas S. 824-5. 463A Abbas. Syed A. 732-5. 121A Akosah. Kwame O. 868-121 • 92A. 877-9. 141A Anderson. H. Vernon 875-38 • 137A. 875-39. 137A. Abbo. Katherine M. 772-5 • 286A Aksu!, Seydi V. 884-74 .lS7A. 915-51. 2SSA 906-32.234A Abbott. Joseph A. 943-14. 361A Akutsu. Naoko 840-35. 20A Anderson. Jeffrey L. 323. xxvii. 844-99. 28A. 747-3 Abdalla, Ismaile S. H. 863-51 • 83A. 882-88. Alam, Mohsin 894-53. 19SA • 178A. 901-49. 209A. 948-93. 372A. 838-4 154A Albano. Maureen P. 958-54. 412A .483A Abdelmeguid. Alaa E. 939-38. 3S1A Alberghini. Tod V. 701-3. SA. 798-6. 396A Anderson. Jill 706-5. 13A. 726-1 .IUA Abdel-Wareth. Laila O. 929-36. 316A Albers. John J. 871-103. HIOA. 739-1 • 131A Anderson. Keaven 714-4. 6OA. 722-5. -

View Our 2014 Annual Report
hephzibah annual report children’s association 2013-2014 “ ...places to play in and pray in where nature may heal and cheer and give strength to the body and soul alike.” EvERYbODY NEEDS bEAUTY — J ohn Muir , naturalist and author (1838-1914) Dear Friend of Hephzibah, “THERE IS SOMETHING INFINITELY HEALING IN THE REPEATED REFRAIN OF these broken family bonds, Hephzibah founded 49 NATURE — the assurance that dawn comes after night, and spring after winter.” an annual sibling camp that reunites brothers Number of neglected and These words were written half a century ago by naturalist Rachel Carson. Yet and sisters living in different group, foster or abused children who found they still resonate today, perhaps because so many of us are suffering from a “nature adoptive homes. In FY14, 56 children reunited a safe haven in our deficit.” Urbanization, the rise of technology and a fear of “stranger danger” have all with their siblings at this rustic overnight camp diagnostic treatment center conspired to drive us indoors and away from the natural world. in northern Illinois and created shared memories and residence Just breathing in the oxygen created by plants and trees or watching a butterfly that will last a lifetime. alight on a flower makes us feel more optimistic, alert and alive. Studies show that Meanwhile, teens from our Foster care program were having a different a connection with nature promotes physical and mental well-being — and makes us kind of camp experience at camp old navy. This partnership between Gap, Inc. kinder and more caring as our values shift from a focus on personal gain to a deeper and local youth organizations brings disadvantaged teens into Old Navy stores connection with the world around us. -

Ferruccio Lamborghini
Editorial In 1981, I started up my new Tonino Lamborghini Style and Accessories company. At the time I was assisting my father in the family group, but I felt the need to do something exclusively of my own, different from the world of engines. I have always been interested in design and accessories. I really liked brands like Gucci and Hermès and I was inspired by them to create an activity with signature branded products. Just as Gucci was inspired by the equestrian world with iconic elements such as a bracket or a bite, I took inspiration from the bearing, the piston, the springs, the suspensions. I’ve always loved products linked to mechanics and engineering. Thus, it was obvious for me that the first accessory that I realized was a watch. And this is the reason why in each product I create a special detail legend of a brand recognized throughout the globe as a beacon of luxury, exclusivity and Italian flair: these are the values of my brand. I hope my clientele understands my personal vision behind all my branded products: to spread the passion and spirit of Italy with unique and distinctive products, inspired by Italian industrial design and the Lamborghini family mechanical heritage. TESORI LATINI is made of liquid metal and kevlar carbon fiber with back cover in Italian leather with double gold stitching line. • 20 Mpx rear camera with F/1.8 and ultrafast autofocus • 5.5’’ 2K-WKHD Amoled display • Dual Hi-Fi audio flagship chipsets with Dolby Audio System, 3D surround sound quality • Qualcomm Snapdragon 820 processor • 4GB RAM -
The Imagery of Interior Spaces
the imagery of interior spaces Before you start to read this book, take this moment to think about making a donation to punctum books, an independent non-profit press, @ https://punctumbooks.com/support/ If you’re reading the e-book, you can click on the image below to go directly to our donations site. Any amount, no matter the size, is appreciated and will help us to keep our ship of fools afloat. Contri- butions from dedicated readers will also help us to keep our commons open and to cultivate new work that can’t find a welcoming port elsewhere. Our ad- venture is not possible without your support. Vive la Open Access. Fig. 1. Hieronymus Bosch, Ship of Fools (1490–1500) the imagery of interior spaces. Copyright © 2019 by the editors and au- thors. This work carries a Creative Commons BY-NC-SA 4.0 International li- cense, which means that you are free to copy and redistribute the material in any medium or format, and you may also remix, transform and build upon the material, as long as you clearly attribute the work to the authors (but not in a way that suggests the authors or punctum books endorses you and your work), you do not use this work for commercial gain in any form whatsoever, and that for any remixing and transformation, you distribute your rebuild under the same license. http://creativecommons.org/licenses/by-nc-sa/4.0/ First published in 2019 by punctum books, Earth, Milky Way. https://punctumbooks.com ISBN-13: 978-1-950192-19-9 (print) ISBN-13: 978-1-950192-20-5 (ePDF) doi: 10.21983/P3.0248.1.00 lccn: 2019937173 Library of Congress Cataloging Data is available from the Library of Congress Book design: Vincent W.J. -

Staff Details 1 Head of the Institution Name: ANTONIETTA ROZZI Designation: PRESIDENT Office Phone:0039 ( 0)187 971385 Mobile No
Staff Details Give details of key Managerial Personnel, all Auditors & Technical / Teaching Experts at the Main Office as well as Branch Office locations. 1 Head of the Institution Name: ANTONIETTA ROZZI Designation: PRESIDENT Office Phone:0039 ( 0)187 971385 Mobile No.:0039 3396208821 Email ID:[email protected] 2 Teaching / technical staff details Name Educational Experien Designati Year of Offic Mobil Emai Natur Qualificatio ce on experienc e e l ID e of n e Phon emplo 2.1 ANTONI Yoga Senior Loong teaching e Anto yment ETTA teacher experien sana, 42 years 0039 niett ROZZI ce in pranayam +39 339 aroz teaching a, mantra, 0187 62088 zi3 yoga and yantra, 9713 21 @g pedagog yoga in 85 mail. All y education. com Free lance teach Yoga Senior asana ers or 2.2 EROS teacher Scientist meditatio volou SELVAN in n 43 years Tel. 0039 omer nteers IZZA oceanogr relax 0187 335 os@t aph technique 6035 84488 in.it research s 54 – 49 and yoga scientific Fax: teachers aspects of 0187 yoga 6259 61 ROSA GIUFFR 2.3 E Pranayam gires Nursery a 20 +39 0039 y@h yoga teacher teachers 0415 33887 otma and yoga 9027 73176 il.co teachers 76 m Doralice Lucchina Asana/Me doral High ditation 20 ice@ 2.4 Yoga school fast teacher teacher web and yoga net.it teacher Yoga Porzia teacher Maria porzi 2.5 Favle lawyer Pranayam +30 afav diploma a 12 +39 32030 @g and yoga Oncologic 0774 18746 mail. teacher al yoga 5715 com teacher 23 Yoga Laura La teacher +39 laula Rosa Pranayam 34740 ro@ 2.6 Pedagogi a 9 73729 yaho st o.it and yoga teacher University +30 Giuliano teacher 34780 giuli Boccali Indian 67946 ano. -

Print Key St No. Pre Street Name St Dir Primary Owner Land Av Total Av PC
print_key St No. pre street name st dir primary_owner land_av total_av PC roll 39.00-2-11 200-300 Aaron Ln Wright, William W 277500 403400 411 1 51.16-3-14 1 Ableman Ave Leizer, Darrin J 46000 230000 210 1 51.16-3-36 2 Ableman Ave Jack, Richard J 74000 370000 210 1 51.16-3-15 3 Ableman Ave Chen, Xue Yong 56000 282000 210 1 51.16-3-35 4 Ableman Ave Stefani, John Nicholas 70000 349000 210 1 51.16-3-16 5 Ableman Ave Wall, Richard R 55000 276000 210 1 51.16-3-34 6 Ableman Ave Pietrosanto, Santina 67000 333000 210 1 51.16-3-17 7 Ableman Ave Hausman, Diane M 46000 228000 210 1 51.16-3-33 8 Ableman Ave Knapp, Sara D 45000 227000 210 1 51.16-3-18 9 Ableman Ave Vonhof, Mary Louise 51000 253000 210 1 51.16-3-32 10 Ableman Ave Duffy, Joseph Patrick 46000 228000 210 1 51.16-3-19 11 Ableman Ave Mora, Jose M III 47000 233000 210 1 51.16-3-31 12 Ableman Ave White, Beatrice A 43000 215000 210 1 51.16-3-30 14 Ableman Ave Crowder, Robert C 54000 271000 210 1 51.16-3-20 15 Ableman Ave Slutskiy, Gregory 52000 260000 210 1 51.16-3-29 16 Ableman Ave Besson, Andrew 57000 283000 210 1 51.16-3-21 17 Ableman Ave Hysenllari, Alida 46000 238000 210 1 51.16-3-28 18 Ableman Ave McDonnell, John W 51000 257000 210 1 51.16-3-22 19 Ableman Ave Leddick, Marjorie 44000 221000 210 1 51.16-3-27 20 Ableman Ave Romano, Linda A 51000 257000 210 1 51.16-3-23 21 Ableman Ave Fraterrigo, Philip A 68000 341000 210 1 51.16-3-26 22 Ableman Ave Thomas, Lee O 46000 230000 210 1 51.16-3-24 23 Ableman Ave Fish, Peter J 67000 335000 210 1 51.16-3-25 24 Ableman Ave Scotti, Peter S 46000 -
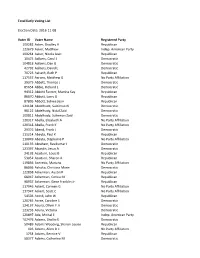
Total Early Voting List Election Date
Total Early Voting List Election Date: 2016-11-08 Voter ID Voter Name Registered Party 109282 Aaker, Bradley H Republican 123679 Aaker, Matthew Indep. American Party 109264 Aaker, Nicola Jean Republican 10475 Aalbers, Carol J Democratic 104818 Aalbers, Dan G Democratic 42792 Aalbers, David L Democratic 70723 Aalseth, Ruth P Republican 117557 Aarons, Matthew G No Party Affiliation 29375 Abbett, Thomas J Democratic 85654 Abbie, Richard L Democratic 94312 Abbott Farmer, Marsha Kay Republican 86670 Abbott, Larry G Republican 87805 Abbott, Sidnee Jean Republican 121104 Abdelhade, Suleiman N Democratic 98122 Abdelhady, Nidal Zaid Democratic 100811 Abdelhady, Sulieman Zaid Democratic 120317 Abella, Elizabeth A No Party Affiliation 120318 Abella, Frank K No Party Affiliation 29376 Abend, Frank J Democratic 111214 Abeyta, Paul K Republican 110049 Abeyta, Stephanie P No Party Affiliation 110135 Abraham, Ravikumar I Democratic 123397 Abundis, Jesus A Democratic 24192 Acaiturri, Louis B Republican 53052 Acaiturri, Sharon A Republican 119856 Acevedo, Mariana No Party Affiliation 86036 Achoka, Christina Marie Democratic 122858 Ackerman, Austin R Republican 68947 Ackerman, Corina M Republican 98937 Ackerman, Gene Franklin Jr Republican 117946 Ackert, Carmen G No Party Affiliation 117947 Ackert, Scott C No Party Affiliation 54503 Acord, John W Republican 120765 Acree, Caroline S Democratic 124137 Acuna, Oliver F Jr Democratic 123233 Acuna, Victoria Democratic 120897 Ada, Michal E Indep. American Party 102476 Adamo, Shellie E Democratic 50489 Adams Wooding, Sharon Louise Republican 426 Adams, Allen D Ii No Party Affiliation 1754 Adams, Bernice V Republican 58377 Adams, Catherine M Democratic 28234 Adams, Cheryl A Republican 28235 Adams, David L Republican 427 Adams, Irma M Indep. -

Carcuro Daniele Castaldo Raffaella Cirigliano
Elenco Regionale delle Fattorie Didattiche N° N° ordine posizione Cognome e Nome Denominazione Azienda Comune Località 1 1 Carcuro Daniele Omonima Genzano di Lucania Loc. Masseria Cafiero 2 2 Castaldo Raffaella Az. Ag. Sant'Agata Melfi C.da Toppo Sant'Agata 3 3 Cirigliano Antonella Il Piccolo Mulino San Severino Lucano C.da Villaneto 4 4 Doino Sandro Tonino La Taverna del Pastore Bella C.da Toppa Castelluccio 5 5 Fonti Elena Carrera della Regina Banzi C.da Cerasola 6 6 Ianniello Emiliano BioAgrisalute Cancellara C.da Carpine 7 7 Imbriani Rocco Il Tratturo Regio Melfi C.da Casonetto 8 8 Lauria Maria Omonima Paterno Loc. Carpineta 9 9 Leggieri Francesca Il Querceto Marsicovetere Loc. Barricelle 10 10 Mancone Mauro Carpe Diem Venosa C.da Boreano ,56 11 11 Miele Maria Concetta Valle Ofanto Rapone C.da Ofanto 12 12 Placella Domenico Antonio Grotta dell'Eremita Castelmezzano C.da Calcescia,1 13 13 Rondinella Franco Apicoltura Rondinella Ripacandida Via Ciriello, 34 14 14 Stellato Maria Az. Zoot. Casearia Chiaromonte C.da Battifarano 15 15 Tufaro Enzo Omonima Terranova del Pollino Loc. Virgallita 16 16 Vignola Maria Antonietta Agriturismo Vignola Marsico Nuovo C.da Capo d'acqua 17 17 Cardinale Domenico Antonio Le Matinelle Matera C.da Le Matinelle 18 18 Dibernardi Pasquale Il Terrazzo sul Sinni Rotondella C.da Caramola 19 19 La Luce Michele Omonima Ginestra C.da Serra del Tesoro 20 20 Leone Rosa Maria Carmela Antica Fattoria Scanzano Jonico Loc. III Cavone 21 22 Pietrapertosa Faustina Soc. Agric. Monteflor sas Genzano di L. Loc. Monteformisiello 22 23 Pucciariello Umberto Omonima Satriano di Lucania C.da Serra 23 24 Saraceno Domenico Masserie Saraceno di D. -

Fifteen Years of Clinical Experience with Hydroxyapatite Coatings in Joint Arthroplasty Springer-Verlag France S.A.R.L Jean-Alain Epinette, MD Michael T
Fifteen Years of Clinical Experience with Hydroxyapatite Coatings in Joint Arthroplasty Springer-Verlag France S.A.R.L Jean-Alain Epinette, MD Michael T. Manley, PhD Fifteen Years of Clinical Experience with Hydroxyapatite Coatings in Joint Arthroplasty Preface by Rudolph G.T. Geesink, MD, PhD Springer Jean-Alain Epinette, MD Clinique Medico-Chirurgicale 200, rue d'Auvergne 62700 Bruay-Labuissiere France Michael T. Manley, PhD 12-A Chestnut Street Ridgewood, NJ 07450 USA ISBN 978-2-287-00508-4 ISBN 978-2-8178-0851-2 (eBook) DOI 10.1007/978-2-8178-0851-2 © Springer-Verlag France 2004 Originally published by Springer Paris Berlin Heidelberg New York in 2004 Apart from any fair dealing for the purposes of the research or private study, or criticism or review, as permitted under the Copyright, Designs and Patents Act 1998, this publication may only be reproduced, stored or transmitted, in any form or by any means, with the prior permission in writing of the publishers, or in the case of reprographic reproduction in accordance with the terms of licenses issued by the copyright. Enquiry concerning reproduction outside those terms should be sent to the publishers. The use of registered names, trademarks, etc, in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant laws and regulations and therefore free for general use. Product liability: the publisher can give no guarantee for information about drug dosage and application thereof contained in this book. In evety individual case, the user must check its accuracy by consulting other pharmaceuticalliterature. -

Dead Silent: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018 Robin Pickering-Iazzi University of Wisconsin-Milwaukee, [email protected]
University of Wisconsin Milwaukee UWM Digital Commons French, Italian and Comparative Literature Faculty French, Italian and Comparative Literature Books Department 2019 Dead Silent: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018 Robin Pickering-Iazzi University of Wisconsin-Milwaukee, [email protected] Follow this and additional works at: https://dc.uwm.edu/freita_facbooks Part of the Criminology and Criminal Justice Commons, Italian Language and Literature Commons, and the Women's Studies Commons Recommended Citation Pickering-Iazzi, Robin, "Dead Silent: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018" (2019). French, Italian and Comparative Literature Faculty Books. 2. https://dc.uwm.edu/freita_facbooks/2 This Book is brought to you for free and open access by UWM Digital Commons. It has been accepted for inclusion in French, Italian and Comparative Literature Faculty Books by an authorized administrator of UWM Digital Commons. For more information, please contact [email protected]. DEAD SILENT: Life Stories of Girls and Women Killed by the Italian Mafias, 1878-2018 Robin Pickering-Iazzi Robin Pickering-Iazzi is Professor of Italian and Comparative Literature in the Department of French, Italian, and Comparative Literature at the University of Wisconsin-Milwaukee. She is the author of The Mafia in Italian Lives and Literature: Life Sentences and Their Geographies, published in Italian as Le geografie della mafia nella vita e nella letteratura dell’Italia contemporanea, and editor of the acclaimed volumes The Italian Antimafia, New Media, and the Culture of Legality and Mafia and Outlaw Stories in Italian Life and Literature. She is currently working on a book that examines representations of feminicide in Italian literature, film, and media.