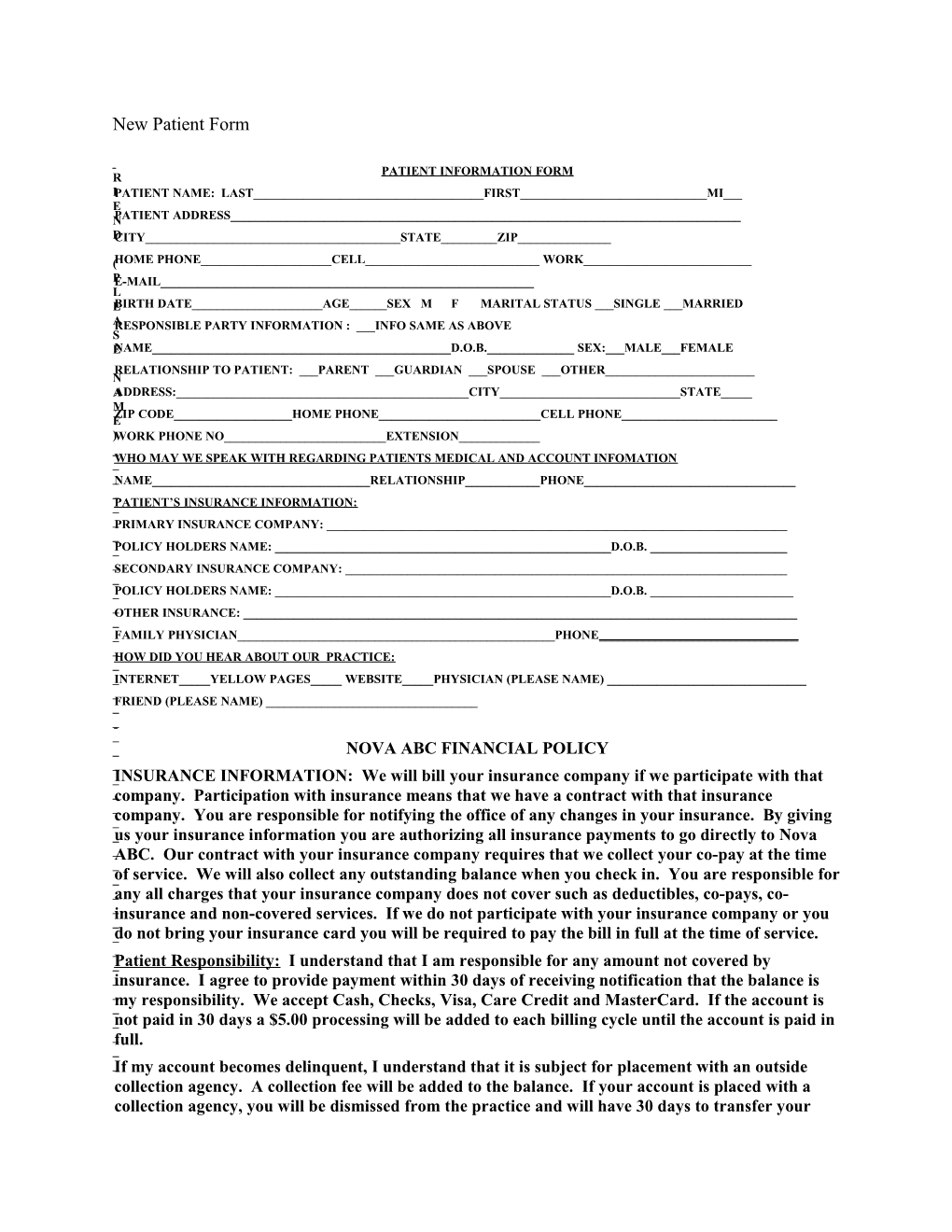
New Patient Form
PATIENT INFORMATION FORM R IPATIENT NAME: LAST______FIRST______MI___ E NPATIENT ADDRESS______DCITY______STATE______ZIP______
(HOME PHONE______CELL______WORK______PE-MAIL______L EBIRTH DATE______AGE______SEX M F MARITAL STATUS ___SINGLE ___MARRIED ARESPONSIBLE PARTY INFORMATION : ___INFO SAME AS ABOVE S ENAME______D.O.B.______SEX:___MALE___FEMALE RELATIONSHIP TO PATIENT: ___PARENT ___GUARDIAN ___SPOUSE ___OTHER______N AADDRESS:______CITY______STATE_____ M ZIP CODE______HOME PHONE______CELL PHONE______E )WORK PHONE NO______EXTENSION______WHO MAY WE SPEAK WITH REGARDING PATIENTS MEDICAL AND ACCOUNT INFOMATION _NAME______RELATIONSHIP______PHONE______PATIENT’S INSURANCE INFORMATION: _PRIMARY INSURANCE COMPANY: ______POLICY HOLDERS NAME: ______D.O.B. ______SECONDARY INSURANCE COMPANY: ______POLICY HOLDERS NAME: ______D.O.B. ______OTHER INSURANCE: ______FAMILY PHYSICIAN______PHONE______HOW DID YOU HEAR ABOUT OUR PRACTICE: _ _INTERNET_____YELLOW PAGES_____ WEBSITE_____PHYSICIAN (PLEASE NAME) ______FRIEND (PLEASE NAME) ______NOVA ABC FINANCIAL POLICY _ _INSURANCE INFORMATION: We will bill your insurance company if we participate with that _company. Participation with insurance means that we have a contract with that insurance _ _company. You are responsible for notifying the office of any changes in your insurance. By giving _us your insurance information you are authorizing all insurance payments to go directly to Nova _ABC. Our contract with your insurance company requires that we collect your co-pay at the time _ _of service. We will also collect any outstanding balance when you check in. You are responsible for _any all charges that your insurance company does not cover such as deductibles, co-pays, co- _ _insurance and non-covered services. If we do not participate with your insurance company or you _do not bring your insurance card you will be required to pay the bill in full at the time of service. _ _Patient Responsibility: I understand that I am responsible for any amount not covered by _insurance. I agree to provide payment within 30 days of receiving notification that the balance is _ _my responsibility. We accept Cash, Checks, Visa, Care Credit and MasterCard. If the account is _not paid in 30 days a $5.00 processing will be added to each billing cycle until the account is paid in _full. _ _If my account becomes delinquent, I understand that it is subject for placement with an outside collection agency. A collection fee will be added to the balance. If your account is placed with a collection agency, you will be dismissed from the practice and will have 30 days to transfer your care to another physician ______Initial Returned Check Fee: A $35 processing fee will be charged for returned checks. That amount must be paid in cash or by credit card prior to making another appointment. ______Initial Treatment of Minors: Any minor (under age 18) who is treated at Nova ABC Weight Loss Center as a new patient must have a parent/legal guardian present with them; any established patient that is 16 or older can come to any follow up appointment without a parent/legal guardian as long as we have been given written consent by the parent/legal guardian to treat the patient for that date of service. Nova ABC Weight Loss Center requires a $60 deposit to reserve an initial appointment with the doctor. This charge will be applied to your first visit; or it is fully refundable as long as the office is given no less than 24 hours’ notice of cancelation. IF YOU ARE CALLING TO CANCEL AFTER HOURS. YOU CAN LEAVE A MESSAGE ON THE MACHINE BY DIALING 703-494-1020 AND PRESSING #8. THIS FEE MUST BE PAID PRIOR TO MAKING ANOTHER APPOINTMENT. ______Initial No Call/No Show Fee: There will be a $50 charge in the event that a patient makes and cancels the first appointment and then reschedules a second appointment and fails to keep that second appointment. In this event the 24 hour rule is waived. YOU MUST KEEP THE SECOND APPOINTMENT IN ORDER TO AVOID THE $50 CHARGE. THERE WILL BE NO EXCEPTIONS TO THIS RULE.
In Addition to the Above policy there is a $5 0 NO SHOW FEE for appointments that are canceled with less than 24 business hours’ notice. HABITUAL CANCELLATIONS AND NO SHOWS WILL RESULT IN TERMINATION FROM THE PRACTICE. I have read and understand the above and agree to these terms.
______SIGNATURE DATE FIRST APPOINTMENT REQUIREMENTS PLEASE DO NOT WEAR ANY OILS, LOTIONS, OR CREAM THE DAY OF THE TEST LABWORK CMP, CBC, LIPID PANEL, FREE T4, URIC ACID, TSH, PHOS PREP FOR METABOLIC TEST: NO EXERCISE OF CAFFEINE THE DAY OF THE APPOINTMENT 4 HOUR FAST (NOTHING BUT WATER) PRIOR TO THE TEST
New Patient Privacy Forms
Northern Virginia Area Bariatric Consultants Privacy Practices This notice describes the way in which medical and personal information pertaining to you may be used and disclosed. It also, explains how you can access your health information. Please review it carefully and sign the attached acknowledgement receipt at the bottom of this notice and return it to the receptionist. At Northern Virginia Area Bariatric Consultants the staff is committed to the protection of your private health information. Within our office access to your information is limited to those employees who need access in order to perform their jobs. Northern Virginia Area Bariatric Consultants may use and disclose protected health information in order to facilitate treatment, collect payments and for internal healthcare operations. Examples of these include, but are not limited to referral to other healthcare providers, life insurance physicals, and home healthcare agencies. Payment examples include your health insurance provider for claims and coordination of benefits, workman's compensation or similar programs: Collections agencies, etc. Healthcare operations include auditing of records and internal quality control. Northern Virginia Area Bariatric Consultants is required by law to use and/or disclose protected health information without the patients' written consent or authorization in certain circumstances. These include reporting a crime, responding to a subpoena, warrant or court order; public health officials concerned with controlling disease, disability and injury. Northern Virginia Area Bariatric Consultants may use or disclose protected health information to your personal representative whom you have authorized to act on your behalf in making decisions related to your health care. NOVA ABC Weight Loss Clinic will contact patients at phone numbers provided to us by the patient in order to give appointment reminders or other information regarding treatment and/or tests results. NOVA ABC Weight Loss Clinic will not use or disclose a patients protected health information as is described in this notice without the individual's written authorization. This authorization may be revoked at any time in writing. Exceptions are those described above as required by law.
NOVA ABC Weight Loss Clinic will abide by this notice which is currently in effect as of April 14, 2003, at the time of disclosure. We reserve the right to revise the terms of this notice and make new provisions effective for all protected health information we maintain. NOVA ABC Weight Loss Clinic will keep a posted copy of our current privacy practices in our lobby area. Copies of this notice may also be obtained at any time in our office. Any person/patient, who believes their privacy rights have been violated, may register a complaint with our office manager at 703-494-1020; and to the Secretary of Health of Human Services. It is our office policy that no retaliatory action will be made against any individual who submits a complaint of non-compliance of the privacy standards You have the legal right to inspect copies of your protected health information. This requires a written, signed and dated request. (as allowed by State law, reasonable copy fees may apply) If you believe your health information is inaccurate or incomplete, you may request to amend your information. In the event that we deny your request, we will inform you of our reasons for such a denial in writing. You have the legal right to request restrictions on certain uses of your protected health information as provided by 45CFR 154.522(a). By law we are not required to comply with a requested restriction.
Acknowledgement of Privacy Practices: I have received a notice of privacy practices, outlining my rights regarding my protected health information and the specific ways in which my private health information may be used and disclosed as allowed under state and federal law. Patient or legal Representative______Date______Relationship of above if not signed by patient______In the event patient refused to sign______
WEIGHT LOSS CONSENT FORM I______authorize Dr William C. McCarthy and his staff at Northern Virginia Area Bariatric Consultants to help me in my weight reduction efforts. I understand that my program may consist of a balanced diet, a regular exercise program, instruction in behavior modification techniques, and may involve the use of appetite suppressant medications. Other treatment options may include a very low calorie diet, or a protein supplemented diet. I further understand that if appetite suppressants are used, they may be used for durations exceeding those recommended in the medication package insert It has been explained to me that these medications have been used safely and successfully in private medical practices as well as in academic centers for periods exceeding those recommended in the product literature. I understand that any medical treatment may involve risks as well as the proposed benefits. I also understand that there are certain health risks associated with remaining overweight or obese. Risks of this program may include, but are not limited to, nervousness, sleeplessness, headaches, dry mouth, gastrointestinal disturbances, weakness, tiredness, psychological problems, high blood pressure, rapid heartbeat and heart irregularities. These and other possible risks could, on occasion be serious or even fatal. Risks associated with remaining overweight are tendencies to high blood pressure, diabetes, heart attack and heart disease, arthritis of the joints including hips, knees, feet and back, sleep apnea, and sudden death. I understand that these risks may be modest if I am no significantly overweight, but will increase with additional weight gain. I understand that much of the success of the program will depend on my efforts and that there are no guarantees or assurances that the program will be successful. I also understand that obesity may be a chronic, life-long condition that may require changes in eating habits and permanent changes in behavior to be treated successfully. I have read and fully understand this consent form and I realize I should not sign this form if all items have not been explained to me. My questions have been answered to my complete satisfaction. I have been urged and have been given all the time I need to read and understand this form. If you have any questions regarding the risks or hazards of the proposed treatment, or any questions whatsoever concern the proposed treatment or other possible treatments, ask your doctor now before signing this consent form. Date______Time______Witness______Patient______
Weight-Loss Consumer Bill of Rights WARNING: Rapid weight loss may cause serious health problems. Rapid weight loss is weight loss of more than 1 1/2 pounds to 2 pounds per week or weight loss of more than 1 percent of body weight per week after the second week of participation in a weight loss program. Consult your personal physician before starting any weight loss program. Only permanent lifestyle changes such as making healthful food choices and increasing physical activity, promote long-term weight loss. Qualifications of this provider are available upon request. You have the right to ask questions about the potential health risks of the program and its nutritional content, psychological support, and educational components; receive an itemized statement of the actual or estimated price of the weight loss program, including extra products, services, supplements, examinations and laboratory tests; know the actual or estimated duration of the program. I have read the above: Patient's Signature______Date______Release of Medical Records I give permission for my medical records (blood work, chart, EKG) to be release to (this applies to a family member)
Name______Signature______Date______
BEFORE" AND "AFTER" PHOTOS I______, give my permission for NOVA ABC to take my "before" and "after" photographs. (photographs will not be used for advertising without patient permission) Signature______PATIENT INFORMED CONSENT FOR APPETITE SUPPRESSANTS I. Procedure and Alternatives: 1. I______(patient or patient's guardian) authorize Dr. William C. McCarthy to assist me in my weight reduction efforts. I understand my treatment may involve, but not be limited to, the use of appetite suppressants for more than 12 weeks and when indicated in higher doses than the dose indicated in the appetite suppressant labeling. 2. I have read and understand my doctor's statements that follow: "Medications, including the appetite suppressants, have labeling worked out between the makers of the medication and the Food and Drug Administration. This labeling contains, among other things, suggestions for using the medication. The appetite suppressant labeling suggestions are generally based on the shorter term studies (up to 12 weeks) using the dosages indicated in the labeling. "As a bariatric physician, I have found the appetite suppressants helpful for periods far in excess of 12 weeks, and at times in larger doses than those suggested in the labeling. As a physician, I am not required to use the medication as the labeling suggests, but I do use the labeling as a source of information along with my own experience, the experience of my colleagues, recent longer term studies and recommendations of university based investigators. Based on these, I have chosen, when indicated, to use the appetite suppressants for longer periods of time and at times, in increased doses." "Such usage has not been as systematically studied as that suggested in the labeling and it is possible, as with most other medications, that there could be serious side effects (as noted below)." "As a bariatric physician, I believe the probability of such side effects is outweighed by the benefit of the appetite suppressant use for longer periods of time and when indicated in increased doses. However, you must decide if you are willing to accept the risks of the side effects, even if they might be serious, for the possible help the appetite suppressants use in this manner may give." 3. I understand it is my responsibility to follow the instructions carefully and to report to the doctor treating me for my weight any significant medical problems that I think may be related to my weight control program as soon as reasonably possible. 4. I understand the purpose of this treatment is to assist me in my desire to decrease my body weight and to maintain this weight loss. I understand my continuing to receive the appetite suppressant will be dependent on my progress in weight reduction and weight maintenance.
5. I understand there are other ways and programs that can assist me in my desire to decrease my body weight and to maintain this weight loss. In particular, a balanced calorie counting program or and exchange eating program without the use of the appetite suppressant would likely prove successful if followed, even though I would probably be hungrier without the appetite suppressants. II. Risks of Proposed Treatment I understand this authorization is given with the knowledge that the use of the appetite suppressants for more than 12 weeks and in higher doses than the dose indicated in the labeling involves some risks and hazards. The more common include nervousness, sleeplessness, headaches, dry mouth, weakness, tiredness, psychological problems, medication allergies, high blood pressure, rapid heartbeat and heart irregularities. Less common, but more serious, risks are primary pulmonary hypertension and valvular heart disease. These and other possible risks could, on occasion, be serious or fatal. III. Risks Associated with Being Overweight or Obese: I am aware that there are certain risks associated with remaining overweight or obese. Among them are tendencies to high blood pressure, to diabetes, to heart attack and heart disease, and to arthritis of the joints, hips, knees and feet. I understand these risks may be modest if I am not very much overweight but that these risks can go up significantly the more overweight I am. IV. No Guarantees: I understand that much of the success of the program will depend on my efforts and that there are no guarantees or assurances that the program will be successful. I also, understand that I will have to continue watching my weight all of my life if I am to be successful. Patient's Consent: I have read and fully understand this consent form and I realize I should not sign this form if all items have not been explained, or any questions I have concerning them have not been answered to my complete satisfaction. I have been urged to take all the time I need in reading and understanding this form and in talking with my doctor regarding risks associated with the proposed treatment and regarding other treatments not involving the appetite suppressants.
IF YOU HAVE ANY QUESTIONS AS TO THE RISKS OR HAZARDS OF THE PROPOSED TREATMENT, OR ANY QUESTIONS WHATSOEVER CONCERNING THE PROPOSED TREATMENT OR OTHER POSSIBLE TREATMENTS, ASK YOUR DOCTOR NOW BEFORE SIGNING THIS CONSENT FORM. DATE______TIME______PATIENT______WITNESS______(can be signed by legal guardian if patient is a minor)
VI. PHYSICIAN DECLARATION: I have explained the contents of this document to the patient and have answered all the patient's related questions, and to the best of my knowledge, I feel the patient has been adequately informed concerning the benefits and risks associated with the use of the appetite suppressants, the benefits and risks associated with alternative therapies and the risks of continuing in an overweight state. After being adequately informed, the patient has consented to therapy involving the appetite suppressants in the manner indicated above. Physician's Signature______
NOVA ABC Hours of Operation and Cancellation Policy We make every effort to make sure your visits are pleasant and efficient for you. Please make every effort to arrive at your appointment on time. If you are unable to make your scheduled time just call and notify our office. (AFTER HOURS YOU CAN LEAVE A MESSAGE ON OUR PHONE) Or email us at [email protected] Our patient hours are as follow: Monday 12:30 pm -7 pm Tuesday 12:30 pm -7 pm Wednesday 6:30 am -11:30 am Thursday 6:30 am -1 pm Friday 6:30 am-10 am Phone hours are available to make appointments between 9 am - 4 pm Monday-Tuesday, 9 am - 2 pm Wednesday-Thursday and Fridays between 6:30am - 12 pm (these hours are subject to change depending on staff availability) If you need to miss an appointment please call 24 hours in advance to cancel in order to avoid a $50.00 no-show fee. Again you can call after hours and leave a message on our answering machine. Our phone number is 703-494-1020 and press #8 to leave a message. I ACKNOWLEDGE THE ABOVE MENTIONED NO-SHOW POLICY AND UNDERSTAND I WILL BE CHARGED $50.00 FOR FAILURE TO GIVE 24 HOURS NOTICE TO THE OFFICE OF CANCELLATION.
______NAME DATE
New Patient History Forms
NOVA ABC Medical History Form Name: ______Age: ______Sex: M F (circle one) Family Physician: ______Phone: ______Present Status: 1. Are you in good health at the present time to the best of your knowledge? Y N 2. Are you under a doctor’s care at the present time? Y N If yes, for what? ______3. Are you taking any medications at the present time? Y N What: ______Dosage: ______What: ______Dosage: ______4. Any allergies to any medications? Y N What: ______5. History of high blood pressure? Y N 6. History of pre-diabetes or diabetes? Y N At what age? ______7. History of heart attack or chest pain? Y N 8. History of swelling feet? Y N 9. History of frequent headaches? Y N Migraines? Y___ N ___ Medications for headaches: ______10. History of sleep apnea? Y___ N___ Have you ever had a sleep study? Y N Result of Sleep Study:
Do you snore? Y___ N___ Have you been told you quit breathing while sleeping? Y___ N___ Do you fall asleep while driving, riding in a car >30 min, reading, or watching TV? Describe ______11. History of constipation (difficulty in bowel movement)? Y N 12. History of glaucoma? Y N 13. Gynecologic history: Pregnancies: Number: ______Dates: ______Is there any chance of pregnancy now? Y___ N___ Natural delivery or C-Section (specify): ______Complications of pregnancy (e. g. gestational diabetes, preeclampsia, eclampsia, etc.) Describe: ______Menstrual: Onset Age: _____ Regular: Y___ N___ If periods are not regular (not regular, excessively heavy, etc.), please describe______
______Have you ever been diagnosed with polycystic ovary syndrome? Y___ N___ Pain associated: Y___ N___ Last menstrual period: ______Hormone Replacement Therapy: Y N What: ______Birth Control Pills: Y N Type: ______Last Checkup:______
14. Serious Injuries: Y N Specify: ______15. Any surgery: Y N Specify: ______Date: ______Specify: ______Date: ______16. Family History: Age Health Disease Cause of Death Overweight? Father: ______Mother: ______Brothers: ______Sisters: ______
Has any blood relative ever had any of the following: Glaucoma: Y N Who: ______Asthma: Y N Who: ______Epilepsy: Y N Who: ______High Blood Pressure Y N Who: ______Kidney disease: Y N Who: ______Diabetes: Y N Who: ______Tuberculosis: Y N Who: ______Psychiatric Disorder Y N Who: ______Heart disease/stroke Y N Who: ______
Past Medical History: (circle all that apply) Polio Measles Tonsillitis Jaundice Mumps Pleurisy Kidneys Scarlet Fever Liver Disease Lung Disease Whopping Cough Chicken Pox Rheumatic Fever Bleeding Disorder Nervous breakdown Ulcers Gout Thyroid Disease Anemia Heart Valve Disorder Heart Disease Tuberculosis Gallbladder Disorder Psychiatric Illness Drug Abuse Eating Disorder Alcohol Abuse Pneumonia Malaria Typhoid Fever Cholera Cancer Blood transfusion Arthritis Osteoporosis Other: ______
Nutrition Evaluation: 1. Present weight: Height (no shoes): Desired weight: 2. In what time frame would you like to be at your desired weight? ______3. Birth Weight: Weight at 20 years of age: Weight one year ago: 4. What is the main reason for your decision to lose weight? ______5. When did you begin gaining excess weight? (Give reasons, if known); ______6. What has been your maximum lifetime weight (non-pregnant) and when? ______7. Previous diets you have followed: Give dates and results of your weight loss: ______8. Is your spouse, fiancé or partner overweight? Y N By how much is he or she overweight? 9. How often do you eat out? 10. What restaurants do you frequent? 11. How often do you eat fast foods? 12. Who plans meals? Cooks? Shops? 13. Do you use a shopping list? Y N 14. What time of the day and what day do you shop for groceries? 15. Food Allergies (list):
16. Food dislikes (list):
17. Foods you crave: 18. Any specific time of the day or month do you crave food? 19. Do you drink coffee or tea? Y N How much daily? 20. Do you drink soft drinks? Y N How many daily? Diet or regular? 21. Do you drink alcohol? Y N How much?
22. Do you use a sugar substitute? Y N 23. Do you awaken hungry during the night? Y N What do you eat? Have you ever found evidence of night time eating without your knowledge? ______24. What are your worst food habits? Do you binge eat? Y___ N ___ How often? ______25. Have you ever induced vomiting or taken laxatives or diuretics for weight loss? Have you ever been diagnosed with bulimia? Y____ N___ Have you ever been diagnosed with Anorexia Nervosa? Y___ N___ 26. Snack Habits: What? When? How Much? 27. When you are under a stressful situation at work or family related, do you tend to reach more? Explain:
28. Do you think are currently undergoing a stressful situation or an emotional upset? Explain:
29. Smoking habits: (answer only one) ____ You have never smoked cigarettes, cigars or a pipe ____ You quit smoking ______years ago and have not smoked since______You have quit smoking cigarettes at least one year ago and now smoke cigars or a pipe without inhaling smoke ____ You smoke 20 cigarettes per day (1 pack) ____ You smoke 30 cigarettes per day (1 1/2 pack) ____ You smoke 40 cigarettes per day (2 packs) 30. Typical Breakfast Typical Lunch Typical Dinner Time eaten: ______Time eaten:______Time eaten:______Where: ______With whom: ______31. Describe your usual energy level: 32. Activity Level: (answer only one) ____ Inactive not regular physical activity with a sit-down job. ____ Light activity no organized physical activity during leisure time. ____ Moderate activity-occasionally involved in activities such as weekend golf, tennis, jogging, swimming or cycling. ____ Heavy activity consistent lifting, stair climbing heavy construction, etc. or regular ____ Vigorous activity participation in extensive physical exercises for at least 60 minutes per Session 4 times per week. 33. Behavior style: (answer only one) ____ You are always calm and easy going. ____ You are usually calm and easy going. ____ You are sometimes calm with frequent impatience. ____ You are seldom calm and persistently driving for advancement. ____ You are hard-driving and can never relax. Current Symptoms (please circle if present) General: Appetite Increase Appetite Decrease Chills Fatigue Fever Sweats Eyes Last check up (Date or how long ago)______Blurred vision Double vision Cataracts Eye pain Redness Glaucoma Y N Recent change in vision Y N Ears Decreased hearing Pain Ringing/Use of hearing device Y N Nose Allergies Congestion Obstruction Y N Throat Enlarged tonsils Snoring Sore throat trouble swallowing Y N Cardiovascular Chest pain or pressure, fainting or black out spells / Heart murmur Palpitations(racing heart or skipped beats) Shortness of breath Trouble lying flat Swelling in legs or feet Respiratory (Lungs) Congestion Cough Rattling or wheezing Stomach and gastrointestinal Last colonoscopy (year) ______Bloody stools Cramps Constipation Diarrhea Heartburn or reflux Nausea Pain Vomiting Muscles, joints, and bones Arthritis Back pain Joint pain or stiffness (where)______Morning stiffness Muscle pain Muscle weakness
Skin Acne Dry or scaly Itching Lump, nodule, or mole (where)______Nail changes Rash (where)______Breast Last mammogram______Discharge Lump Pain Rash or redness Neurologic Forgetfulness Numbness Weakness Psychiatric Anxiety Crying spells Depression Insomnia Panic attacks Rage or temper problems Suicidal feelings Hormones (Circle all that applies) Excessive hunger Excessive thirst Decreased libido Hoarseness Recent hair growth Hormones (Female) Last female exam ______Change in periods Y N Blood and circulation Clotting problems Easy bruising Allergy and immune Frequent infection Seasonal allergies Please describe your general health goals and improvements you with to make:
What kind of dietary approach do you feel is best for you? (Circle one, feel free to leave blank, we’ll go over this): ALL FOOD, PARTIAL MEAL REPLACEMENT (USE A MEAL REPLACEMENT FOR ONE OR MEALS DAILY, OR TOTAL MEAL REPLACEMENT (Very low calorie protein Sparing fast for quicker weight loss). Do you feel you will need medication for appetite suppression?
Do you want vitamin B12 shots? (These are not given routinely, but many patients request them) Y N This information will assist us in assessing your particular problem areas and establishing your Medical management.
Thank you for your time and patience in completing this form.
2014 NEW PATIENT FORM.docx