UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes
Help Notes for Paediatric Crohn’s Disease (Inpatients)
Patient Identification. Patients should be included if they have a primary discharge diagnosis of Crohn’s Disease that matches the ICD-Codes provided We know that there are often problems with miscoding so it will ultimately be the responsibility of the clinical lead at each site, or other designated IBD team members under their guidance, to decide whether the admission was primarily for Crohn’s Disease and if the case note details should therefore be audited. Only include admissions of >24 hours. Do not enter data for day cases such as for endoscopy or drug infusions.
We know that many sites choose to complete the details of each admission on the paper proforma prior to transferring the details onto the website. A general rule when completing the form is that where you see boxes as options for answers then you can choose multiple options for answers (i.e. all that apply). Circle options indicate that a single option must be chosen. Where you see a combination of boxes with a circle choosing the answer option next to a circle will mean that none of the answer options with a box next to them can therefore be chosen.
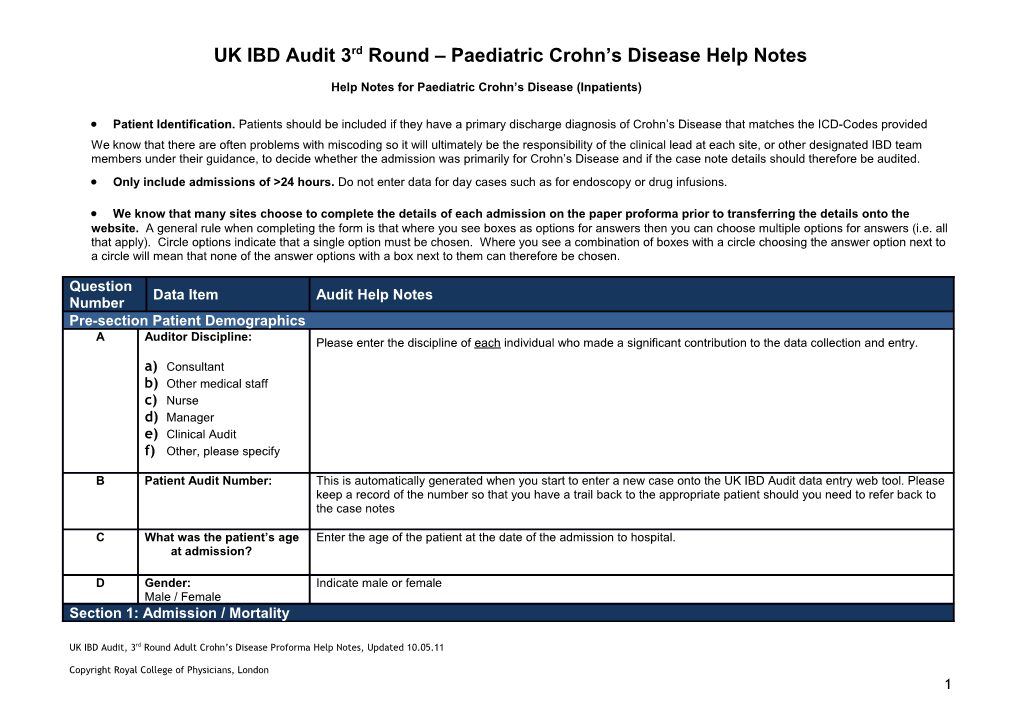
Question Data Item Audit Help Notes Number Pre-section Patient Demographics A Auditor Discipline: Please enter the discipline of each individual who made a significant contribution to the data collection and entry. a) Consultant b) Other medical staff c) Nurse d) Manager e) Clinical Audit f) Other, please specify
B Patient Audit Number: This is automatically generated when you start to enter a new case onto the UK IBD Audit data entry web tool. Please keep a record of the number so that you have a trail back to the appropriate patient should you need to refer back to the case notes
C What was the patient’s age Enter the age of the patient at the date of the admission to hospital. at admission?
D Gender: Indicate male or female Male / Female Section 1: Admission / Mortality
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 1 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number 1.1 Admission 1.1.1 What was the date of admission Please enter the date of admission to your hospital in the format: to this hospital? day (DD), month (MM) year (YYYY) DD/MM/YYYY
Only enter details of one admission per patient even if they were admitted more than once during the audit period, that being the admission closest to 1st September 2010.
Source: This will be found on electronic patient management systems and within medical and nursing notes 1.1.2 What was the primary reason a) Emergency admission for active CD: means acute admission from GP/A&E/other hospital for admission? b) Planned admission for active CD: patient seen as outpatient or by GP and admission arranged by hospital. c) Elective admission for surgery: surgery planned prior to the admission a) Emergency admission for d) New diagnosis of Crohn’s Disease active CD e) Transferred from another site for surgery b) Planned admission for active f) Transferred from another site for further medical management CD *If IBD was not the primary reason for admission please discard the patient’s notes, and move on to the c) Elective admission for surgery next applicable patient. d) New diagnosis of Crohn’s Disease If the primary reason for admission is option c) Elective admission for surgery, or e) transferred from e) Transferred from another site another site for surgery, then a number of subsequent questions in the dataset do not need to be answered. for surgery By section these are: f) Transferred from another site Section 1, questions 1.1.3 through to 1.1.7i for further medical Section 2, the entire section can be ignored management Section 3, ignore all questions in section 3 apart from 3.1.1 1.1.3 Which specialty was This can be difficult to clearly assess but we want to determine whose care the patient was under from the period 24 responsible for the patient's hours after the initial admission to hospital. care 24 hours after admission? a) Acute medicine Source: Which specialty the patient is under can be obtained from case note entries by specialist teams b) Paediatric gastroenterology (consultant, SpR, F1, F2 or other grade), from nursing notes or hospital transfer notes; it can also be inferred from c) Paediatric surgery transfer to a specialist ward. d) General paediatrics within a paediatric GI network e) Adult gastroenterology f) Colorectal surgery g) General paediatrics h) Other, please specify
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 2 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number
1.1.4 What date was the patient first Enter the date when the patient was first seen by a Consultant Paediatric Gastroenterologist during the admission. seen by a Consultant Paediatric ‘Seen by’ includes direct hand-written entries by consultants, typed letters or where noted by another member of the Gastroenterologist? team e.g. ‘patient reviewed by Dr…’
_ _ / _ _ / _ _ _ _ If the patient was not seen by a Consultant Paediatric Gastroenterologist during the admission enter ‘not seen’. Not seen Not required You have an additional option to indicate that review by a consultant paediatric gastroenterologist was not required, for instance if admitted under the direct care of a Consultant Paediatric Surgeon. To be able to tick ‘Not Required’ on the audit website you will need to select ‘Not Seen’ first, however we would like to confirm that if this is done the answer will be considered as ‘Not Required’ during data analysis.
Source: From medical, nursing or therapy records
1.1.5 What date was the patient first Enter the date when the patient was first seen by a Consultant Paediatric Surgeon during the admission. seen by a Consultant Paediatric ‘Seen by’ includes direct hand-written entries by consultants, typed letters or where noted by another member of the Surgeon? team e.g. ‘patient reviewed by Mr / Miss…’
_ _ / _ _ / _ _ _ _ If the patient was not seen by a Consultant Paediatric Surgeon during the admission select ‘not seen’. Not seen Not required You have an additional option to indicate that review by a Consultant Paediatric Surgeon was not required, for instance if admitted under the direct care of a Consultant Paediatric Gastroenterologist. To be able to tick ‘Not Required’ on the audit website you will first need to tick ‘Not Seen’, however we would like to confirm that if this is done the answer will be considered as ‘Not Required’ during data analysis 1.1.6 Was the patient seen by a This refers to being seen by a Paediatric IBD Specialist Nurse at any time during the admission. This does not Paediatric IBD Nurse Specialist include being seen by a stoma nurse only. during the admission? Yes No Source: entry in the continuing care case notes, direct entry in nursing notes or entry in notes commenting that patient seen by IBD Nurse/GI Nurse 1.1.7 Was the patient transferred to a Answer ‘yes’ to this question if the patient was transferred to a specialist paediatric gastroenterology ward at any specialist paediatric time during their admission gastroenterology ward? A specialist paediatric gastroenterology ward is defined for this audit as one where paediatric gastroenterology Yes patients (including liver disease) are routinely allocated and that have specialist medical, nursing and allied health No professional staff. It can be a medical, surgical or joint specialist ward
Source: From medical, surgical, nursing or therapy records or hospital patient administration records
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 3 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number
1.1.7i If yes to Q 1.1.7, which type of If you answered Yes to Q1.1.7 you should indicate which type of specialist paediatric gastroenterology ward the ward? patient was transferred to from the following options:
a) Medical a) Medical: A ward in the hospital which predominantly deals with medical paediatric b) Joint Medical / Surgical gastroenterology b) Joint Medical / Surgical: A joint medical and surgical paediatric gastroenterology ward c) Surgical c) Surgical: A ward in the hospital which predominantly deals with surgical paediatric gastroenterology
Source: From medical, surgical, nursing or therapy records or hospital patient administration records
1.2 Comorbidity
1.2.1 Did the patient have any There only needs to be a mention of these in clerking notes or previous letters, rather than extensive supporting significant comorbid diseases? information, to include as comorbidity. You can choose more than one option. (select all that apply) If you choose ‘other’ please be sure to give further details. Only include ‘other’ if it is a significant comorbidity such a) Respiratory as non-cured cancer (except BCC). b) Stroke c) Liver Disease d) None Source: Clerking notes / Patient Letters e) Other, please specify
1.3 Discharge / Mortality
1.3.1 Did the patient die during Indicate whether the patient died during the admission admission? If no, you must still answer Q1.3.1iii below Yes No
1.3.1i If yes, Date of death? Please enter the date of death in the format: day (DD), month (MM) year (YYYY) = DD/MM/YYYY
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 4 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number _ _ / _ _ / _ _ _ _
1.3.1ii If yes, please write the primary If a post mortem was performed state the primary cause of death indicated on the post mortem report. cause of death in the space below If there was no post mortem state the primary cause of death entered on the death certificate counter foil in the (appears as Q1.3.1iii on the web notes. tool) If neither of the above are available then you can use the last primary diagnosis stated in case notes recorded prior to, or after death.
Source: patient case notes, death certificate, post mortem report 1.3.1iii If no to 1.3.1, Date of Discharge If you answered No to Q 1.3.1 then you must enter the date of discharge from your hospital in the format: day (DD), month (MM) year (YYYY) DD/MM/YYYY _ _ / _ _ / _ _ _ _ Source: This will be found on PAS medical or nursing notes 1.3.1iv Was the patient: Please indicate the destination that the patient was discharged to a) Discharged home b) Transferred to another site for surgery c) Transferred to another site for Source: patient case notes, PAS system further medical management 1.4 Medication on Admission 1.4.1 What treatment was the patient Include only oral drugs and drugs which are used directly for the treatment of Crohn’s Disease: taking for Crohn’s Disease on admission? (select all that apply) a) 5-ASA drugs: includes drugs such as Salazopyrine, Balsalazide, Pentasa, Asacol, Olsalazine, Salofalk. Only record oral 5-ASA a) 5-ASA b) Azathioprine b) Azathioprine c) Mercaptopurine d) Methotrexate c) Mercaptopurine e) Antibiotics: Only include those used to treat Crohn’s Disease e.g. Ciprofloxacin or Metronidazole d) Methotrexate f) Corticosteroids: Prednisolone or Budesonide. Only record oral steroids e) Antibiotics g) Dietary therapy-exclusive enteral liquid therapy: f) Corticosteriods h) Dietary therapy–supplemental enteral liquid therapy: g) Dietary Therapy – exclusive h) Anti–TNF: Infliximab or Adalimumab. Include if currently on Adalimumab. Include if having regular Infliximab enteral liquid therapy infusions (8 weekly or less) or if had Infliximab within the previous 8 weeks. Include if on Thalidomide for treatment of Crohn’s Disease
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 5 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number h) Dietary Therapy – j) Other: (eg trial medication) Do not include treatment not specifically for Crohn’s; disease, e.g. treatment for supplemental enteral liquid osteoporosis, vitamin B12, folic acid. Please indicate details of the ‘Other’ treatment in the space provided. therapy i) Anti-TNF-α Source: From medical, nursing or therapy records j) None k) Other (e.g. trial medicine) 1.4.2 In the 12 months prior to this When looking to answer ‘Yes’ or ‘No’ include any dose of corticosteroids (Prednisolone or Budesonide) taken admission was the patient continuously for more than 3 months for Crohn’s Disease (and not any other indication) during the 12 months prior taking Steroids (at any time) for to the date of this admission >3 months? Source: Medical or nursing notes; Clinic letters 1.4.2i If yes, was an appropriate dose Please answer Yes or No reduction planned? Yes / No Source: Medical or nursing notes; Clinic letters 1.4.2ii If yes, was bone protection Bone protection agents such as calcium, calcium with vitamin D, Bisphosphonates (alendronate, risendronate, used? disodium etindronate) Yes / No Source: Medical or nursing notes, Clinic letters 1.4.2iii Was a DEXA scan done? Bone densitometry may be measured by DEXA scan or heel ultrasound. Yes No Source: Medical or nursing notes, clinic letters or radiology or nuclear medicine results section 1.4.2iv Was a course of exclusive enteral nutrition administered in the past 12 months? Yes / No 1.5 Smoking Status (only to be completed for children aged 12 and over) 1.5.1 What was the smoking status Current smoker - if the patient is either a) currently smoking or b) has given up within the last 3 months of the patient? Lifelong non-smoker/ex-smoker - if stopped smoking >3 months ago or never smoked a) Current smoker Not documented - if no documentation of smoking status on this admission b) Lifelong non-smoker / ex smoker Source: Medical or nursing notes c) Not documented 1.6 Patient History 1.6.1 Did the patient have a pre- If the primary reason for admission was indicated as c) Elective admission for surgery in Q 1.1.2 then you do not
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 6 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number admission diagnosis of Crohn’s need to answer this question. Disease? If patient had previous diagnosis of Crohn’s Disease based on endoscopic, histological or radiological evidence and/or began any active treatment for CD (at any time) then class as a pre-admission diagnosis of Crohn’s Disease. Yes No If the patient had been referred by GP (or others) with a possible diagnosis of CD but diagnosis had not been made then class as ‘no pre-admission diagnosis of CD’
Source: Medical, nursing or therapy records. An established diagnosis of Crohn’s Disease will most often be recorded in the initial clerking. However you may need to search previous clinic letters 1.6.2 What was the extent of the a) Terminal ileum (L1) disease? b) Colonic (L2) – Evidence of colonic disease by endoscopy or radiology with no evidence of small bowel disease. (select all that apply) c) Ileo-colonic (L3) – Both small bowel and colonic disease d) Perianal Disease – No evidence of small bowel or colonic disease but with Crohn’s fissures / fistulas / perianal a) Terminal ileum (L1) abscesses b) Colonic (L2) e) Oral f) Upper GI (L4) c) Ileo-colonic (L3) g) Not known – Only tick this if there is no clearly identifiable extent of disease. d) Perianal e) Oral Do not include: Gastro-duodenal Crohn’s or Oral Crohn’s patients f) Upper GI (L4) g) Not known Source: From medical, nursing or therapy records or IBD database 1.6.3 Has the patient had previous Answer ‘Yes’ or ‘No’ admissions to your hospital with Crohn’s Disease in the two years prior to this admission? Yes No Source: From medical, nursing or therapy records or hospital patient administration records. 1.6.3i If yes, how many times in the 2 Count all admissions with the primary diagnosis as Crohn’s Disease in the 2 years prior to the audited admission. years prior to this admission? This includes both surgical and medical admissions. Do not include day case/overnight admissions for drug infusions / transfusions / endoscopy. Do not include admission to other hospitals.
Source: From medical, nursing or therapy records or hospital patient administration records. Section 2: Assessing the Severity of Crohn’s Disease (with reference to your answer to Q1.1.2, if the patient was either admitted electively for surgery, or transferred from another site for surgery ignore all of section 2) 2.1 Initial assessment during first full day following admission 2.1.1 Number of liquid stools per Record the number of liquid / semi-formed stools indicated in the handwritten case notes or clinic letter to GP. Include day: all bowel movements regardless of whether only blood or mucus or faecal. Sometimes it can be difficult to find a
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 7 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number _ _ precise measure. If it is documented as ‘8-10X a day’, answer with the highest number recorded. Not documented Not required Source: Medical or nursing notes and typed letters 2.1.2 General well being: This data item is subjective and can be difficult to decide. There is no pre-defined definition of severity. The scoring system relates to the modified Harvey Bradshaw index to patient’s description of general well being. If general well- Well being is recorded then define as follows: “Well” = well; “Below par” = mild symptoms; “Poor” = moderate symptoms; Mild symptoms “terrible” = severe symptoms. Moderate symptoms Severe symptoms If general well-being is not recorded and/or you can’t make value judgement from the clinical details from that clinic Not documented visit, enter “Not Documented”.
Source: Medical or nursing notes and typed letters. 2.1.3 Abdominal Pain: If there is no documented abdominal pain put “Not documented” rather than “None”. If the severity is not specifically recorded, but abdominal pain is mentioned, you will have to make a judgment on None severity. If you can not make a judgement on the available data in the case notes, put “Not documented”. Present Not documented Source: Medical or nursing notes and typed letters. 2.1.4 Abdominal Mass Dubious = thickened small bowel or colonic loops but not recorded as definite mass. None Present Source: Medical or nursing notes and typed letters. Not documented 2.1.5 Did the patient report any of the following All listed options require one of the following responses: complications? Yes / No / Not documented Mouth ulcers Arthralagia Pyoderma Gangrenosum Anal fissure Fistula Erythema Nodusm Abscess Iritis Other, please Specify Source: Medical or nursing notes and typed letters 2.1.6 What were the admission Record results of blood tests either done at this clinic visit or in the 4 weeks before or after this clinic visit. If multiple results for the following blood tests done in this time then document those done nearest to this clinic visit
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 8 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number tests? 2.16i CRP mg/L The initial results for CRP on admission must be between 0 and 800 _ _ _ Not documented 2.16ii HB g/dL The initial result for Hb on admission must be between 2.0 and 20.0 _ _ _ Not documented 2.16iii Albumin g/L The initial result for Albumin on admission must be between 5 and 50 _ _ Not documented Source: Laboratory results section of case notes most likely source. Other sources may be hand written case notes, clinic letters. If none found then check computerised laboratory results service in your organisation (if one exists) 2.2 Exclusion of Infection (in patients with diarrhoea as a presenting symptom) 2.2.1 Was a stool sample sent for Record as ‘Yes’ if a stool sample was sent for standard stool culture if the patient had diarrhoea (i.e. was producing Standard Stool Culture? loose or semi-formed stools) Do not include for any subsequent episodes of diarrhoea following admission Yes / No /NA Source: Best source will be microbiology report which should have the date sample received. Also review PAS/computer records and medical, nursing or therapy records 2.2.1i Date sent? Record the date that stool culture was sent. If the patient had a stool sample sent within 7 days prior to admission this can included in this section. _ _ / _ _ / _ _ _ _ Source: Best source will be microbiology report which should have the date sample received. Also review PAS/computer records and medical, nursing or therapy records 2.2.1ii Was it positive? Answer ‘Yes’ or ‘No’
Yes / No Source: Best source will be microbiology report, PAS / computer records or medical, nursing or therapy records 2.2.1iii Date of positive sample DD / MM / YYYY
2.2.2 Was a stool sample sent for If the patient had diarrhoea (i.e. was producing loose or semi-formed stools) then record if and when the stool sample CDT? was sent. Do not include for any subsequent episodes of diarrhoea following admission. Record the date that the stool sample was sent. If the patient had a stool sample sent within 7 days prior to Yes / No / NA admission this can included in this section.
Source: Best source will be microbiology report which should have the date sample received. Also review PAS/computer records and medical, nursing or therapy records 2.2.2i Date sent DD / MM / YYYY
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 9 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number 2.2.2ii Was it positive?
Yes / No Source: Microbiology report / PAS / computer records / medical, nursing or therapy records 2.2.2iii Date of positive sample DD / MM / YYYY
Source: Microbiology report / PAS / computer records / medical, nursing or therapy records
2.3 Weight assessment and dietetic support during admission 2.3.1i Was the patient’s weight Record if the patient’s weight was recorded at any time during admission. Weight may be recorded in the medical measured during notes, nursing notes, observation chart or in separate dietetic notes. Body Mass Index is weight (Kg) divided by admission? height2 (meters). Yes / No Source: Dietetic/Medical/Nursing/Therapy notes. If you are not sure where the dietician enters information in the case a) Was BMI measured? report contact your dietetic department. In some hospitals the dietetic records are kept separately from the rest of the Yes / No notes 2.3.1ii Was the patient’s height measured during admission? Yes / No Source: Dietetic/Medical/Nursing/Therapy notes 2.3.2 Did a dietician see the Did a dietician visit the patient at any time during admission? patient? Yes / No Source: Dietetic/Medical/Nursing/Therapy notes 2.3.3 Was dietary treatment Any dietary advice or dietary supplements given to the patient. This includes general advice on a diet high in calories, initiated? advice on dietary supplements, specific Crohn’s specific dietary therapy to treat active disease or TPN. Yes / No Source: Dietetic/Medical/Nursing/Therapy notes 2.3.3i Was exclusive liquid Discuss with Dietetics Department if unsure enteral nutrition therapy prescribed? Yes / No Source: Dietetic/Medical/Nursing/Therapy notes 2.3.3ii Was supplemental liquid Discuss with Dietetics Department if unsure enteral nutrition therapy prescribed? Yes / No Source: Dietetic/Medical/Nursing/Therapy notes 2.3.4 Was parenteral nutrition Includes central or peripheral parenteral nutrition given at any point during admission including after surgery. given? Yes / No Source: Dietetic/Medical/Nursing/Therapy notes
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 10 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number Section 3: Medical Interventions (with reference to your answer to Q1.1.2, if the patient was admitted electively for surgery or transferred from another site for surgery ignore sections 3.2 and 3.3 (other than Q3.3.2) and 3.4 3.1 Use of anti-thrombotic therapy 3.1.1 Did the patient have a thrombotic episode during this admission?
Yes / No Source: medical, nursing or therapy records 3.1.2 Was the patient given Any dose of Heparin and can either be fractionated or unfractionated Heparin. prophylactic Heparin?
Yes / No Source: Drug chart, medical, nursing or therapy records 3.2 Steroid Therapy 3.2.1 Were corticosteroids i. Indicate “yes” if IV steroids were used at any time except if given after surgery. Any intravenous corticosteroid administered during this preparation that was used to treat Crohns should be included. admission? ii. Oral steroids: any orally administered corticosteroid that was used to treat Crohns should be included Yes / No iii. No……Indicate here if either a) no steroids were used or b) no IV or oral steroids were used i.e. steroid enemas or 3.2.1i If yes, which were initially suppositories. prescribed a) IV corticosteroids b) Oral corticosteroids Source: Drug charts, medical, nursing or therapy records, hospital patient administration records 3.2.2 Which of the following Only include either oral corticosteroids (Prednisolone or Budesonide) or IV steroids (Hydrocortisone or steroids were prescribed? Methylprednisolone). Do not include rectal or topical steroids.
a) Prednisolone i, ii, iii, iv st b) Budesonide It can occasionally be difficult to define the dose at initiation or increase. For example, if the 1 doctor prescribed 20mg prednisolone this would be the initial dose and later that day a 2nd doctor increased it to 40mg then this would c) Hydrocortisone be the increased dose. You may need to use your judgment to decide a significant increase in therapy and the dose. d) Methylprednisolone In general, this will be the maximum daily dose in first 72 hours after admission. Record the highest dose prescribed i. Initial dose? in the first 48 hours of any steroid (oral or IV) prescription. (Mg/day) ii. What date was If the patient was admitted on steroids and the dose was increased, record the increased dose the therapy initiated? iii. Was therapy
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 11 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number increased during this Source: Drug charts, medical, nursing or therapy records, hospital patient administration records admission? Yes / No iv. What date was therapy increased? 3.3 Which other therapies did the patient receive? 3.3.1 Anti-TNF therapy i. Record date anti-TNF therapy started (Infliximab or Adalimumab) initiated if applicable to this admission. Yes / No ii. Select this if the patient required no further therapies during this admission. i) Start Date ii) Did the patient respond? Yes / No Source: Medical or nursing notes 3.3.2 Clinical Trial i. Please record the name of the clinical trial Yes / No ii. Record the date the clinical trial started with this patient i) Please specify: iii. ‘No’ Select this if the patient required no further therapies during this admission ii) Start date iii) Did the patient respond? Yes / No Source: Medical or nursing notes 3.3.3 Significant Other Please include only significant other medical therapies. If the patient underwent surgery at this point, select ‘no’ and therapies? all relevant surgical data will be captured in section 4 Yes / No i) Please provide the name of the other therapy provided i) Please specify ii) Start Date iii) Did the patient respond? Yes / No Section 4: Surgical Interventions (If you indicated b) transferred to another site for surgery in your answer to Q1.3.1v, ignore all of section 4. Q4.1.1 will automatically default to ‘No’ on the web tool if that is the case 4.1 Surgical Therapy 4.1.1 Did the patient have surgery “Yes” includes any operation including minor Perianal surgery. on this admission? Answer “No” if only examination under anaesthetic (EUA) was performed without any intervention. Do not include endoscopic procedures. Yes / No Source: Medical Notes / Nursing Notes. 4.1.2 What date was the decision Record the date that the initial decision was taken to undertake surgery for Crohn's Disease. This may occasionally made to operate made? difficult to determine. The date that the decision was made to operate may be prior to the admission date ie in the
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 12 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number outpatient department. Note the date the decision was definitely made to operate rather than “planning”. _ _ / _ _ / _ _ _ _ If notes state something like ‘if CRP>??, and diarrhoea unchanged in 2 days then will need surgery’ then indicate Not known date as 2 days from that entry. Source: Medical case notes 4.1.3 What was the date of the Record date first operation was performed surgery? Use format: day (DD), month (MM) year (YYYY) DD/MM/YYYY
_ _ / _ _ / _ _ _ _ Source: Medical Notes / Nursing Notes. 4.1.4 Was there a delay of more than 24 hours between Compare the dates of 4.1.2 and 4.1.3 to determine if there was a ‘delay’ between the decision being made and the decision to operate and actual date of the operation. If there was a delay of 24 hours or more then please indicate what the reason for this surgery for non-elective delay was. patients? Yes / No
4.1.4i If yes, what was the reason for the delay?
a) Improvement in severity of Crohn’s b) Cancelled due to lack of theatre time c) Cancelled for other clinical reasons (e.g. correction of hypokalaemia) d) Patient declined surgery or needed time to consider Source: Medical case notes, operation notes e) Other please specify 4.1.5 Was the patient seen by a Entries from stoma nurse may be in the medical, nursing notes or separate stoma care nursing notes. If you have stoma nurse during this difficulty finding this information, contact your stoma nurse (if you have one) and ask. admission? Yes / No i. Enter date first seen by stoma nurse during this admission. Do not include if the patient was seen in the outpatient department but not during this admission i. If yes, what date was the DD / MM / YYYY patient first seen by a stoma
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 13 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number nurse? Source: Medical notes/Nursing notes 4.1.6 What was the grade of the The operation notes should include details of all those present at the operation. Please indicate who was the most senior surgeon senior member of staff that was present at the operation, they may not have necessarily performed or led on the present? operation.
a) Consultant Paediatric Consultant Paediatric Surgeon: a surgeon who has Surgeon Consultant Colorectal surgeon: a surgeon who has a specialist interest in colorectal surgery and is a member of ACPGBI b) Consultant Colorectal Consultant GI surgeon (non-colorectal): a GI surgeon with a non-colorectal specialty interest e.g. upper GI or Surgeon hepato-biliary-pancreatic surgery c) Consultant GI Surgeon Consultant General Surgeon: a surgeon with general rather than specialist interest (non-colorectal) Other Surgical Consultant: a surgeon with a specialist interest which is non-GI e.g. vascular surgeon, breast d) Consultant General Surgeon surgeon, gynaecologist, transplant surgeon e) Other Consultant Surgeon Specialist registrar: includes research registrar f) Specialist Registrar Other: state which grade e.g. F2, staff grade, associate specialist g) Other, please specify Source: Medical notes, operation note, nursing or anaesthetic notes. If you are unsure about which grade of surgeon performed the surgery contact your surgical colleagues who may be able to help you. 4.1.7 What were the indications for Record the primary indication(s) for surgery prior to operation. In some cases there may be multiple indications, surgery? (Select all that for example perforation and abscess drainage. apply) Failure of medical therapy: Failure of any type of medical therapy and surgery performed because of continued a) Failure of Medical Therapy symptoms. Do not grade as failure of medical therapy if any more specific indication is present Toxic megacolon: transverse colon >5.5cm on X-ray (plain abdominal X-ray or CT scan) b) Toxic megacolon Bleeding: if primary indication was to stop uncontrolled or continued bleeding c) Bleeding Obstruction: If preoperative symptoms or radiology suggested significant obstruction d) Obstruction Completion proctectomy: Record as completion proctectomy if this was the primary reason cited for the operation. e) Completion protectomy High Grade, Low Grade, Ungraded Dysplasia: Record as dysplasia/cancer if planned surgery where there was known to be colonic dysplasia or cancer. Do not include if found after surgery f) High Grade Dysplasia Cancer: Record if dysplasia or cancer from pre-operative histology g) Low Grade Dysplasia Perforation: Record as perforation if known to have a perforation pre-operatively h) Ungraded Dysplasia Abscess: Include intra-abdominal abscess, perineal abscess, ischio-rectal abscess i) Cancer Formation of ileostomy: Record as formation of ileostomy if this was the primary reason cited for the operation j) Perforation Closure of stoma: Record as closure of stoma if this was the primary reason cited for the operation Other: try to keep to the above indications wherever possible. If there is an exceptional indication please state what k) Abscess this is l) Formation of ileostomy m) Closure of stoma
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 14 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number n) Other indication, please Source: The primary indication for surgery will usually be recorded on the operation note. If it is not recorded there specify you may have to infer the indication from preceding entries in medical notes or the results of investigation (eg radiology showing abscess or perforation) 4.1.8 Type of intervention (select all Try to keep to the listed broad interventions wherever possible. that apply) If there was a major intervention (eg colectomy) together with a minor intervention, only record the major a) Segmental / extended intervention. colectomy b) Subtotal colectomy p) other - If there is an exceptional indication not included in this list please state what this is. c) Protocolectomy d) Stricturoplasty e) Ileal / Jejunal Resection f) Resection of intra- abdominal fistula g) Proctectomy h) Completion proctectomy i) Ileocolonic resection j) Drainage of abscess k) Formation of ileostomy or colostomy l) Revision of stoma m) Perineal procedure n) Closure of stoma o) Division of adhesions 4.1.8i p) Other intervention, please Indicate ‘yes’ if surgery was completed laparoscopically or laparoscopically-assisted. This will be indicated in the specify operation notes. If the operation was started laparoscopically but required to be converted to an open operation answer ‘No’ Was the surgery done laparoscopically / Source: If you are unsure about which type of operation was performed contact your surgical colleagues laparoscopically-assisted? Yes / No 4.1.9 Was the ASA status recorded ASA is the American Society of Anaesthesiologists grade that is widely used as a predictor of operative mortality. pre-operatively? This information should be recorded in the anaesthetic records that are usually in a separate part of the case notes. Yes / No It may be entered in the medical hand written case notes prior to surgery.
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 15 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number
The ASA status can be difficult to find. If you are not familiar with surgical or anaesthetic notes please contact your If yes, what was the ASA anaesthetics department who should be able to tell you where this information is documented. Status? 1 / 2 / 3 / 4 / 5 / N/A Source: Anaesthetic notes. Operation or medical notes
4.2 Surgical Complications 4.2.1 Did the patient suffer from any Wound Infection - This is defined as one or more of the following: evidence of purulent discharge from wound, of these complications wound infection requiring additional antibiotic therapy, and/or requires further surgery following their surgery? Rectal stump complications - For example continued bleeding per rectum which requires additional medical (select all that apply) therapy or further surgery during the admission or dehiscence of rectal stump Intra-abdominal bleeding - Confirmed by imaging and/or requiring angiogram or further surgery. a) Wound Infection Intra-abdominal sepsis - Confirmed by imaging (ultrasound, CT or MRI scan) and/or requiring either surgical or b) Rectal stump complications radiological drainage Anastomotic leakage - Evidence of leakage of luminal contents in surgical drain, collection of fluid around c) Intra-abdominal bleeding anastomosis either by radiology or further surgery during the admission d) Intra-abdominal sepsis Stoma complications - These will include ischaemia, retraction or separation of stoma, peristomal fistula or high e) Anastomotic leakage output stoma (defined as requiring additional IV fluids more than one week after surgery). Only include this as a high f) Stoma complications output stoma if this is the primary reason for continuing IV fluids g) Deep vein thrombosis (DVT) Deep Vein Thrombosis (DVT) - Confirmed by ultrasound, CT or other imaging modality Pulmonary Embolus (PE) - Confirmed by V/Q scan or CT pulmonary angiography or pulmonary angiography h) Pulmonary embolus (PE) Ileus requiring TPN - Record if prolonged ileus after surgery such that PN was initiated to provide nutrition or PN i) Ileus requiring TPN was continued which had been started prior to surgery j) Cardiac Cardiac - Myocardial infarction (raised troponin T, or troponin I), congestive cardiac failure (clinical or radiological k) Respiratory evidence) Respiratory - Defined as symptomatic chest infection/pneumonia requiring additional antibiotic therapy l) Clostridium difficile- Clostridium difficile-associated diarrhoea (CDAD) - Select if the patient presented with CDiff related diarrhoea associated diarrhea (CDAD) following surgery when there was no indication of the infection prior to surgery m) Other, please specify n) No complications 4.3 Post-Operative Prophylactic Therapy 4.3.1 Was the patient prescribed Record any of these drugs that were started or continued after surgery. any of the following drugs on discharge? d) 5-ASA drugs include: Salazopyrine, Balsalazide, Pentasa, Asacol, Olsalazine, Salofalk (please select all that apply)
a) Azathioprine
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 16 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number b) Mercaptopurine c) Metronidazole d) 5-ASA e) Methotrexate f) Infliximbab g) Other, please specify Source: Discharge summary / medical or nursing notes / drug chart h) None Section 5: Discharge Arrangements (If the patient died during the admission or you indicated either b) transferred to another site for surgery or c) transferred to another site for further medical management in your answer to Q1.3.1v ignore all of section 5 5.1 Discharge Arrangements 5.1.1 Was the patient taking oral Record whether the patient was taking oral steroids when discharged. steroids on discharge? Yes / No / N/A Source: Discharge summary, drugs on discharge note to GP, medical or nursing notes, patient administration system 5.1.1i Was a steroid reduction The reduction programme should be documented either in the discharge summary or in a copy of the letter sent to the programme started on patient’s GP. discharge? Yes / No / N/A Source: Discharge summary, drugs on discharge note to GP, medical or nursing notes, patient administration system 5.1.1ii Were bone protection Bone protection agents such as calcium, calcium with vitamin D, Bisphosphonates (Alendronate, Risendronate, agents prescribed? Disodium Etindronate) Yes / No / N/A Source: Discharge summary; Discharge letter to the GP; Medical or nursing notes 5.1.2 Was patient on an immunosuppressive on discharge? Yes / No / N/A
5.1.2i If yes, which one? a) Cyclosporin b) Methotrexate c) 6MP Source: Discharge summary, drugs on discharge note to GP, medical / nursing notes, patient administration system, d) Azathioprine drug chart e) Other, please specify
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 17 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number 5.1.3 Was there a plan for The maintenance programme should be documented either in the discharge summary or in a copy of the letter sent to maintenance Anti TNF on the patient’s GP. discharge? Yes / No / N/A Source: Discharge summary, drugs on discharge note to GP, medical or nursing notes, patient administration system Section 6: Outpatient Visits 6.1 Patient History 6.1.1 Did the patient have This only includes previous outpatient visits in your Trust / Health Board. Do not include outpatient visits to other previous outpatient visits for organisations for management of Crohn’s. Crohn’s Disease at this hospital in the 12 months? * If no, you do not need to answer any further questions in this section Yes / No* Source: From medical, nursing or therapy records or hospital patient admin records. 6.1.2 How many times was the Include all recorded OPD visits (for the management of Crohn’s Disease) over 12 months. Do not include day cases patient reviewed for their (eg endoscopy, blood transfusions and drug infusions) or OPD visits for other reasons. Do not include outpatient Crohn’s Disease in an visits to other hospital trusts for Crohn’s Disease. outpatient’s clinic in the 12 months prior to the start The number of visits must be between 1 and 20 date of this admission? _ _ Source: The most appropriate data source will be PAS. Alternatively, hand-written case notes and typed letters. 6.1.3 Approximately how many The patient may have been seen by more than one health care professional in a single visit and it is important to times was the patient seen record all of these contacts, please count each staff member individually by the following staff in the 12 months prior to the start You will need to check typed letters/handwritten notes for mention of ‘seen by…’ or ‘discussed with…’ date of this admission? i. Paediatric Consultant ii. Paediatric IBD Nurse Specialist iii. Paediatric SpR iv. F2 (SHO) Source: Medical / nursing / clinic notes 6.1.4 What was the date of the last This is the last documented OPD visit for Crohn’s Disease prior to admission. If the last visit was the one which visit at the Outpatient initiated the inpatient admission being audited in sections 1 to 5 please ignore it and use the previous one. Department prior to admission? Source: Medical / nursing / clinic notes 6.1.5 Was the patient’s height recorded during the outpatient visit? Yes / No Source: Medical / Nursing / Therapy notes / patient growth chart
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 18 UK IBD Audit 3rd Round – Paediatric Crohn’s Disease Help Notes Question Data Item Audit Help Notes Number 6.1.6 If the patient was 10 years or older at the time of the last outpatient visit have they had their pubertal status recorded in the past 12 months? Yes / No / NA Source: Medical / Nursing / Therapy notes /
UK IBD Audit, 3rd Round Adult Crohn’s Disease Proforma Help Notes, Updated 10.05.11
Copyright Royal College of Physicians, London 19