Brian C. Toolan MD Orthopaedic Foot and Ankle Surgery The University of Chicago Section of Orthopaedic Surgery and Rehabilitation Medicine 5841 S. Maryland Ave. MC 3079 Chicago Illinois 60637 Phone 773.702.6984 Fax 773.702.0076
Plantar Fasciitis
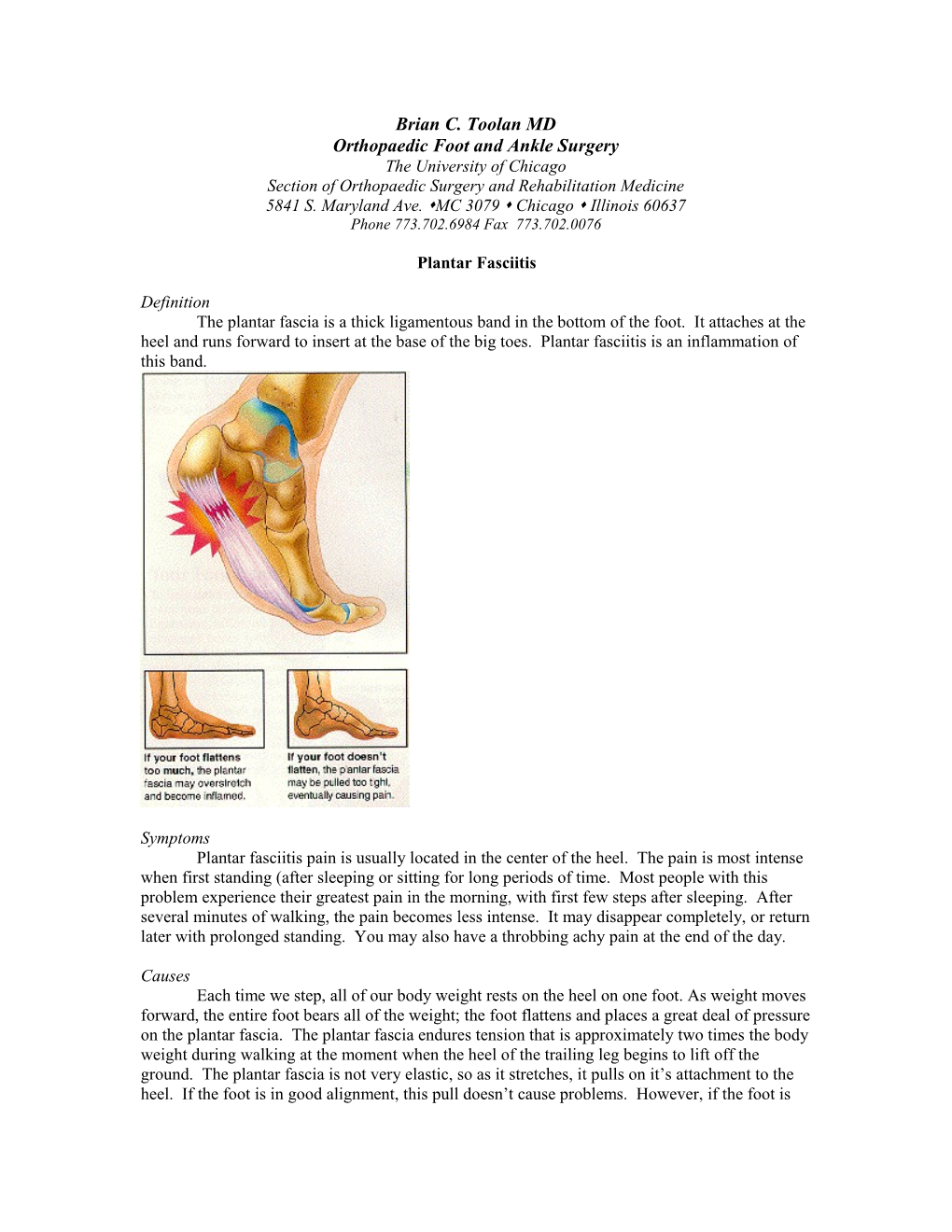
Definition The plantar fascia is a thick ligamentous band in the bottom of the foot. It attaches at the heel and runs forward to insert at the base of the big toes. Plantar fasciitis is an inflammation of this band.
Symptoms Plantar fasciitis pain is usually located in the center of the heel. The pain is most intense when first standing (after sleeping or sitting for long periods of time. Most people with this problem experience their greatest pain in the morning, with first few steps after sleeping. After several minutes of walking, the pain becomes less intense. It may disappear completely, or return later with prolonged standing. You may also have a throbbing achy pain at the end of the day.
Causes Each time we step, all of our body weight rests on the heel on one foot. As weight moves forward, the entire foot bears all of the weight; the foot flattens and places a great deal of pressure on the plantar fascia. The plantar fascia endures tension that is approximately two times the body weight during walking at the moment when the heel of the trailing leg begins to lift off the ground. The plantar fascia is not very elastic, so as it stretches, it pulls on it’s attachment to the heel. If the foot is in good alignment, this pull doesn’t cause problems. However, if the foot is not in proper alignment, it can cause an abnormal stretching in the inflexible plantar fascia, which in turn pulls abnormally hard on the attachment on the heel. Alignment problems that contribute to plantar fasciitis include pronated feet (feet roll inward), flat feet or fallen arches, and supination (the foot rolls outward). People with high arches tend to have feet that supinate or roll outward, and a short tight plantar fascia. Another cause is Achilles tendon tightness. The Achilles tendon also attaches to the heel bone. If the Achilles tendon is too tight, this tension gets redistributed to the plantar fascia. When you aren’t walking, the Achilles tendon is relaxed and shortens naturally. It must elongate and stretch out all over again, putting stress on the plantar fascia. This also helps to explain while your heel pain is usually worse in the morning or when you stand up. In both cases, the abnormal stress placed on the attachment of the plantar fascia at the heel usually causes pain and swelling. If this process continues the plantar fascia can tear. The body will fill in this torn area with scar tissue, which is less elastic than the plantar fascia. The pain can actually be accredited to tearing of the plantar fascia after it has contracted at night or at rest. Other causes include a change or increase in activities, no arch support in the shoe, being overweight, a sudden injury, shoes with little cushioning on hard floors or ground shoes that do not have flexible soles, wearing very high heeled shoes, or spending too much time on your feet.
Treatment Treatment is directed toward realigning the foot as it goes through the gait cycle to prevent the effect on the plantar fascia of supination and pronation. To accomplish proper alignment, orthotics are used. Orthotics gently hold up the foot in a proper, neutral position when the foot hits the ground preventing supination or pronation. They also perform the function of supporting the arch, and cushioning the heel to help alleviate pain. Night splints are also helpful in treating plantar fasciitis. The purpose of night splints is to keep the Achilles tendon and plantar fascia from contracting at night. By not contracting, they stay stretched out and alleviate the pain you have in the morning. Night splints do take some time to get used to. They should be worn as much as possible at night, every night or the first two months. The third month you will begin to wean your self from the splints. To do this the first week, wear the splint five nights a week. The second week, wear the splint 3 night, third week two night and last week one night. Anti-inflammatory medication may also help to alleviate some of the pain and inflammation. You may be prescribed a prescription strength anti-inflammatory. Ice is also effective to reduce inflammation. Physical therapy may be initiated for a few sessions to show you stretching exercises. Stretching the Achilles tendon by doing a “runner’s stretch” is very effective for relieving pain. Also stretching the arch of the foot is effective. These stretching exercises should be performed several times a day. You may also benefit from doing them first thing in the morning to help alleviated the morning pain. Physical therapy can also perform basic modalities, which include heat, ice and iontophoresis.
It is important to remain patient during your treatment. It usually takes approximately 3 months to return to a pain free state. Maintenance stretching should also be done to prevent reoccurrence. The amount of time it takes for the pain to immediately go away depends on the amount of time the symptoms were present before treatment.