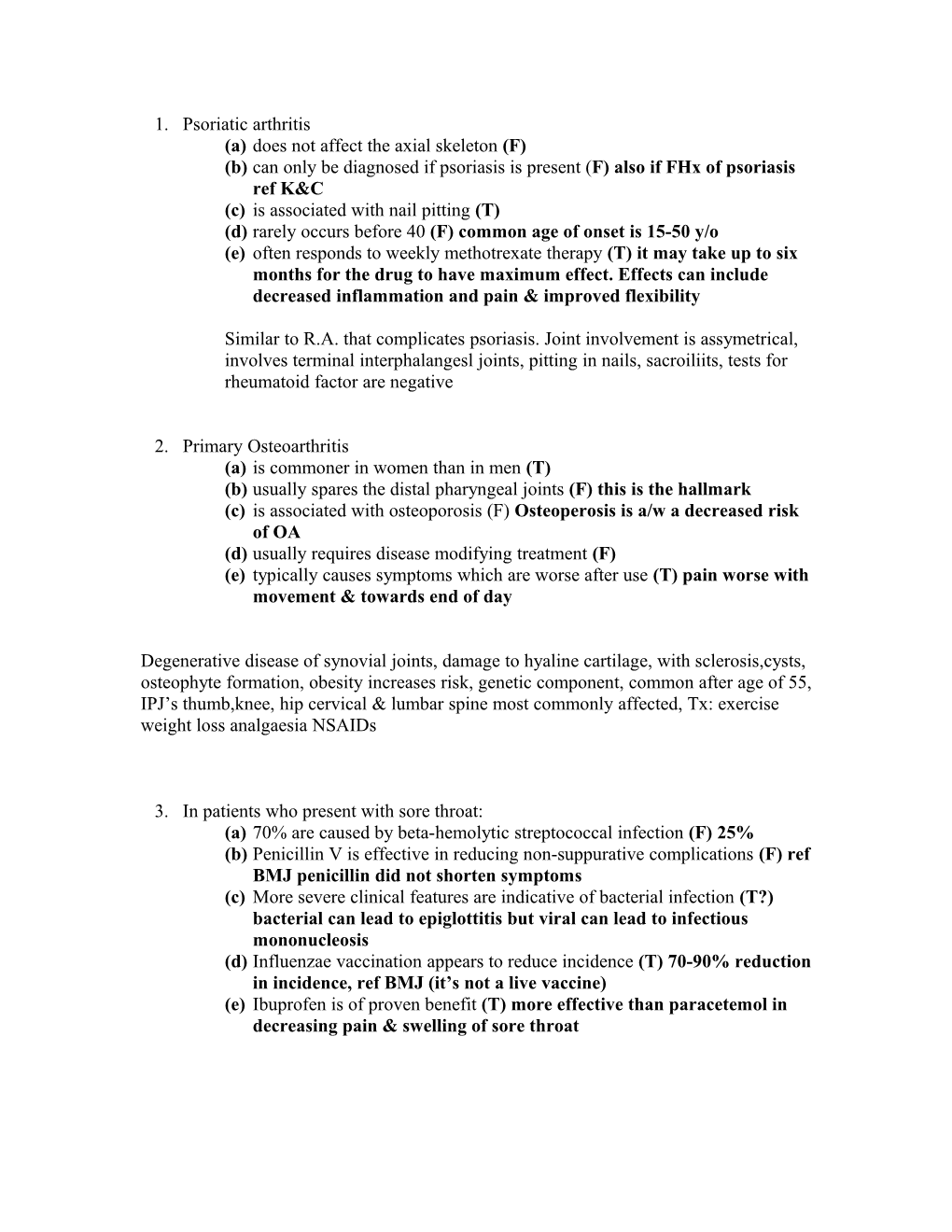
1. Psoriatic arthritis (a) does not affect the axial skeleton (F) (b) can only be diagnosed if psoriasis is present (F) also if FHx of psoriasis ref K&C (c) is associated with nail pitting (T) (d) rarely occurs before 40 (F) common age of onset is 15-50 y/o (e) often responds to weekly methotrexate therapy (T) it may take up to six months for the drug to have maximum effect. Effects can include decreased inflammation and pain & improved flexibility
Similar to R.A. that complicates psoriasis. Joint involvement is assymetrical, involves terminal interphalangesl joints, pitting in nails, sacroiliits, tests for rheumatoid factor are negative
2. Primary Osteoarthritis (a) is commoner in women than in men (T) (b) usually spares the distal pharyngeal joints (F) this is the hallmark (c) is associated with osteoporosis (F) Osteoperosis is a/w a decreased risk of OA (d) usually requires disease modifying treatment (F) (e) typically causes symptoms which are worse after use (T) pain worse with movement & towards end of day
Degenerative disease of synovial joints, damage to hyaline cartilage, with sclerosis,cysts, osteophyte formation, obesity increases risk, genetic component, common after age of 55, IPJ’s thumb,knee, hip cervical & lumbar spine most commonly affected, Tx: exercise weight loss analgaesia NSAIDs
3. In patients who present with sore throat: (a) 70% are caused by beta-hemolytic streptococcal infection (F) 25% (b) Penicillin V is effective in reducing non-suppurative complications (F) ref BMJ penicillin did not shorten symptoms (c) More severe clinical features are indicative of bacterial infection (T?) bacterial can lead to epiglottitis but viral can lead to infectious mononucleosis (d) Influenzae vaccination appears to reduce incidence (T) 70-90% reduction in incidence, ref BMJ (it’s not a live vaccine) (e) Ibuprofen is of proven benefit (T) more effective than paracetemol in decreasing pain & swelling of sore throat 4. A 41 year old male with poorly controlled type 1 diabetes for 17 years and recently treated hypertension complains of swollen feet and ankles. Possible causes are: (a) diabetic nephropathy (T) (b) autonomic neuropathy (T) (c) recurrent hypoglycemia (?) (d) insulin allergy (?) (e) treatment with calcium channel antagonists (T) cause oedema
5. In acute poisoning, the following are appropriate specific reversal agents: (a) lead- Fuller’s earth (F) used to treat paraquat (herbicide) OD. To treat lead OD: dimercaprol, EDTA, penicillamine (b) Opiates-naloxone (T) (c) Benzodiazepines-flumazenil (T) (d) Warfarrin-red cell concentrate (F) give VitK, prothrombin complex concentrate 2,7,9,10 or fresh frozen plasma 15ml/kg (e) Digoxin-digoxin specific antibody fragments (T) tradename = digibind
6. The following are recognized causes of decompensation in patients with chronic liver disease: (a) Hypoglycemia (T) hypoglycemia is a manifestation of (especially fulminant) hepatic failure because of failure of gluconeogenesis and depletion of glycogen stores. BUT hyperglycemia can occur as well, it’s a common manifestation of chronic liver disease because of insulin resistance. (b) Cefotaxime (T) S/E’s include disturbances in liver enzymes, hepatitis & cholestatic jaundice, ref: BNF (c) Constipation (T) lactulose is given to improve encephalopathy on the basis the you’re excreting out the toxins so I presume constipation has opposite effect-retention of toxins (d) pethidine (T) may precipitate coma in hepatic impairment ref: BNF (e) lactulose (F) this is given to improve encephalopathy
7. A 25 year old man presents with sore throat which had been present 4-5 days. On examination his temperature was 38 degrees. His tonsils were enlarged and inflamed. He had bilateral axillary, supraclavicular and inguinal lymphadenopathy. His lymph nodes were tender. The following should be included in the differential diagnosis: (a) CML (F) non tender lymph nodes (b) Infectious mononucleosis (T) (c) Acute taxoplasmosis (T) (d) Chickenpox (F) (e) HIV infection (F)
8. The following are features of pernicious anemia (a) gastric atrophy (T) (b) malabsorption syndrome (T) decreased intrinsic factor which is needed to absorb B12 (c) mild icterus (T) in chronic severe B12- deficiency,lemon yellew tint (d) paresthesia with impaired vibration and position sense (T) subacute combined combined degeneration of the cord due to B12 deficiency (e) decreased MCV on routine hematological testing (F) increased MCV
Macrocytic anaemia, usually due to B12 def. Auto antibodies against intrinsic factor in stomach which is needed for B12 absorption. Gastrectomy, Crohns are other causes. Middle aged & elderly women, silver hair, blue eyes, lemon yellow tint, vitilgo, fatigue, lethargy, SOB, Tx: vit B12 injections (hydroxycobalamin) 5 times at 2 day intervals and then every 3 months for life.
9. In hereditary hemachromatosis (a) inheritance is autosomal dominant (F) AutRecessive chromosome 6 (b) chondrocalcinosis is a recognized feature (T) occurs in 40% (c) bronze skin pigmentation is due to iron deposition (F) due to melanin rather than iron (d) cardiac failure may be a presenting feature (T) occurs in 15% (e) hepatoma is an important complication (T) primary hepatic CA occurs in ~20% whether treated or not, screen alpha feto protein
Autosomal recessive, chr 6, increased iron absorption & deposition esp in liver pancreas & heart, Occurs most commonly in men over 30 y/o. A/w: DM, skin pigmentation, hepatomegaly, arrhythmias, osteoarthritis, polyarthropathy. Dx: increased iron & ferritin, saturated iron binding capacity, liver biopsy shows iron staining. Tx:weekly venesection until iron levels normal, maintenance venesection every 3 months
10. The following statements about atopic dermatitis are true (a) At some time in their lives, approximately 15% of children develop it (T) (b) UVB is a relatively safe second line treatment (T) (c) Antecubital and popliteal fossae are typical sites (T) (d) Methotrexate may be useful in severe cases (e) Restriction diets are of little proven value in most patients (T) 11. Which of the following treatments are appropriate for the condition listed? (a) Tar for psoriasis (T) also good for chronic atopic eczema (b) Topical steroids for atopic dermatitis (T) (c) Oral steroids for rosacea (?) topical steroids precipitate it as well as hot drinks,C2H5OH & sunlight, give oxytetracycline (d) Cyclosporine for atopic dermatitis (T) (e) Systemic steroids for psoriasis (F) topical steroids
12. Patients with antibody deficiency syndromes typically present with: (a) disseminated viral infections (b) pyogenic bacterial infections (c) bronchiectasis (d) pneumocystis carinii (e) hearing deficit
13. Patients who have undergone splenectomy or who are hyposplenic: (a) are particulary predisposed to viral infections and therefore have influenza immunization annually (?) (b) are particulary predisposed to overwhelming infections caused by pyogenic encapsulated bacteria (T) (c) can withhold antibiotic prophylaxis provided their immunizations are uptodate (d) are predisposed to malaria infections (T) (e) often have a low white cell count (F) usually normal or raised
14. In malignant spinal cord compression (a) pain is the initial symptom in more than 90% patients (?) P/C: spastic paresis, tetraparesis, pain @ level of compression & sensory loss below level of compression (b) cervical spine is most commonly affected (F) thoracic 70%, cervical 20% (c) nerve root irritation produced unilateral or bilateral radicular pain (T) (d) normal plain xrays of the spine will outrule a diagnosis of spinal cord compression (F) spinal MRI is best, also must do CXR, etc to identify primary neoplasm or infection (e) initial management should ordinarily include high dose corticosteroids (T)
15. In pagets disease of bone (a) hypercalcemia is a frequent finding (F) serum Ca++ is usually normal,only get increased Ca++ in severe Paget’s where there is uncoupled resorption (b) both increased osteoblastic and osteoclastic activity occur (T) the disease is basically increased remodeling so there is increased resorption & production (c) sarcoma of long bones is a complication (T) <1% get osteogenic sarcoma, most common sites are femur and pelvis (d) bone pain responds to bisphosphonates (F) only decreases bone turnover, give analgaesics & NSAIDs for bone pain (e) renal calculi are a recognized problem (?) couldn’t find it listed as a complication anywhere but Paget’s can lead to hypercalcaemia in severe cases which would predispose to renal calculi so T?
Pagets is a disease that involves increased bone remodeling, generally a disease of the elderly, Causes: FHx & viral infection of osteoclasts, Complications: fracture, spinal compression, deafness, osteogenic sarcoma,high output heart failure. Tx: analgaesia, NSAIDs, bisphosphonates
Question 16 a) T b) T c) T d) T? e) F
Syndenham’s Chorea may be associated with valvular abnormalities (Rheumatic Fever) Opening snap on auscultation and mid diastolic murmur are associated with mitral stenosis. Presystolic accentuation of a murmur??. Mitral stenosis associated with an accentuated S1, followed by S2, and an opening snap (OS) S4 is due to atrial contraction and therefore will not be present in a fib.
Question 17 a) T b) T c) ?? d) F? e) F
Hypertension is a major risk factor for aortic dissection. Aortic dissection is associated with hypertension (high blood pressure) and many connective tissue disorders. Vasculitis (inflammation of an artery) is rarely associated with aortic dissection. It can also be the result of chest trauma. 72 to 80% of individuals who present with an aortic dissection have a previous history of hypertension. The highest incidence of aortic dissection is in individuals who are 50 to 70 years old. The incidence is twice as high in males as in females (male-to-female ratio is 2:1). Half of dissections in females before age 40 occur during pregnancy (typically in the 3rd trimester or early postpartum period). A bicuspid aortic valve (a type of congenital heart disease involving the aortic valve) is found in 7-14% of individuals who have an aortic dissection. These individuals are prone to dissection in the ascending aorta. The risk of dissection in individuals with bicuspid aortic valve is not associated with the degree of stenosis of the valve.Marfan syndrome is noted in 5-9% of individuals who suffer from aortic dissection. In this subset, there is an increased incidence in young individuals. Individuals with Marfan syndrome tend to have aneurysms of the aorta and are more prone to proximal dissections of the aorta.Chest trauma leading to aortic dissection can be divided into two groups based on etiology: blunt chest trauma (commonly seen in car accidents) and iatrogenic. Iatrogenic causes include trauma during cardiac catheterization or due to an intra-aortic balloon pump.Aortic dissection may be a late sequalae of cardiac surgery. 18% of individuals who present with an acute aortic dissection have a history of open heart surgery. Individuals who have undergone aortic valve replacement for aortic insufficiency are at particularly high risk. This is because aortic insufficiency causes increased blood flow in the ascending aorta. This can cause dilatation and weakening of the walls of the ascending aorta. I found no association with aortic Coarctation but it causes hypertension so perhaps this may be associative??? There is no link with Addisons.
Question 18 a) F b) F c) F d) F e) ??
One spontaneous episode of PE is treated by warfarin for 6 months. Only lifelong if identified cause for the PE e.g. thrombophilia. If asymptomatic not put on anticoagulation for life. If >2 spontaneous episodes plan is more uncertain but may veer towards anticoag for life. Third trimester and postpartum are the maximum risk periods for thrombosis is pregnancy. DDAVP can be used for prophylaxis in bleeding disorders e.g. vWD NOT in thrombophilia. Prophylaxis for thromboembolic disease is LMWH, heparin or warfarin. The response to LMWH is more predictable than heparin and no monitoring is usually required. ? does this make less of a risk of bleeding complications?
Question 19 a) T b) F c) F d) F e) T
Horner’s Syndrome: miosis, eNophthalmous, ptosis and ipsilateral loss of sweating (anhydrosis) due to interruption of face’s sympathetic supply eg at brainstem (demyelination, vasc dis), cord (syringomyelia), thoracic outlet (Pancoasts tumour) or on the sympathetic nerves trip on the internal carotid (carotid aneurysm) Question 20 a) F b) F c) T? d) F e) T
Motor neuron disease is a progressive degenerative disease of upper and lower MOTOR neurons in the spinal cord, cranial nerve motor nuclei and within the cortex. (spinothalamic = sensory) M:F = 3:2 Symptoms usually present between the ages of 50-70, and include progressive weakness, muscle wasting, and muscle fasciculations; spasticity or stiffness in the arms and legs; and overactive tendon reflexes. Patients may present with symptoms as diverse as a dragging foot, unilateral muscle wasting in the hands, or slurred speech. Degeneration is of motor neurons only not cognitive impairment.
Question 21 a) T b) F c) T d) T e) F
ACEIs used for hypertension, post MI, for heart failure. Streptokinase used in STEMI.
Question 22 a) T b) F c) T d) ?F e) F
ACEIs are very useful in diabetics as they decrease intraglomerular pressure, reducing renal damage. Reducing BP reduces microalbuminuria and attenuates loss of GFR. ACEIs redure microalbuminuria and slow progression to CRF even if normotensive. Beta-blockers not generally used in diabetics (altho not absolutely contra-indicated)
Question 23 a) F b) F c) T d) F e) ? Non-pharm management NB for all hypertension. Beta-blockers are diabetogenic and therefore not recommended for use. New recommendations for HTN rx: <55 1st choice is ACEI, >55 or blacks a Thiazide diuretic or calcium channel blocker. No mention of contra-indication with hyperlipidaemia in BNF.
Question 24 a) F b) T? c) F d) T e) F
Postpartum thyrodititis usually self limiting? Carbimazole can’t be used while breast feeding and isn’t used anyway. In the first phase of this condition, you experience signs and symptoms of overactive thyroid (hyperthyroidism). This usually lasts two to four months. Treatment may include beta blockers to reduce symptoms of overactive thyroid. In the second phase, you have signs and symptoms of underactive thyroid (hypothyroidism). This also lasts two to four months. Treatment may include thyroid replacement hormone.
Stop lithium if possible – if not can give thyroxine
Treatment for hirsutism is eflornithine.
Chlorpormazine not listed as treatment for hyperprolactinaemia in BNF. Treatment is bromocripine, cabergoline.
Question 25 a) T b) T c) T d) T e) F
Presentations of Coeliac Disease: steatorrhoe/offensive stools, bloating, nausea, vomiting, aphthous ulcers, angular stomatitis, weight loss, fatigue, weakness, iron-deficiency anaemia, osteomalacia, failure to thrive (children).1/3 may be asymptomatic. Dermatitis herpetiformis is associated with celiac disease (itchy blisters in groups eg on knees, elbows and scalp) Howell Jolly bodies are nuclear remnants seen in RBCs post splenectomy, rarely leukaemis, megaloblastic anaemia, iron-deficiency anaemia, hyposplenism (eg celiac disease, neonates, thalassaemia, SLE, lymphoma, leukaemia, amyloid) The mucosal of the proximal small bowel is predominantly affected, the mucosal damage decreasing in severity towards the ileum as the gluten is digested into smaller non-toxic fragments. Question 26 a) F b) T c) T d) F e) T
A Fib has absent x descent/a wave in JVP Pulsus alternans occurs in LVF Pulsus paradoxus is found in pericardial effusion, constrictive pericarditis and asthma. Plauteau pulse is found in aortic stenosis.
Question 27 a) T b) T c) F? d) F e) T
Plasmapharesis can be used as treatment in hyperviscosity syndrome due to myeloma, waldenstroms macroglobulinaemia, polycythaemia, leukaemia.
Plasmapheresis is a process in which the fluid part of the blood, called plasma, is removed from blood cells by a device known as a cell separator. The separator works either by spinning the blood at high speed to separate the cells from the fluid or by passing the blood through a membrane with pores so small that only the fluid part of the blood can pass through. The cells are returned to the person undergoing treatment, while the plasma, which contains the antibodies, is discarded and replaced with other fluids. Medication to keep the blood from clotting (an anticoagulant) is given through a vein during the procedure. Today, plasmapheresis is widely accepted for the treatment of myasthenia gravis, Lambert-Eaton syndrome, Guillain-Barré syndrome and chronic demyelinating polyneuropathy. Its effectiveness in other conditions, such as multiple sclerosis, polymyositis and dermatomyositis, is not as well established.
An important use of plasmapheresis is in the therapy of autoimmune disorders, where the rapid removal of disease causing autoantibodies from the circulation is required in addition to slower medical therapy.Other uses are the removal of blood proteins where these are overly abundant and cause hyperviscosity syndrome.
Examples of diseases that can be treated with plasmapheresis:
Guillain-Barré syndrome Chronic inflammatory demyelinating polyneuropathy Goodpasture's syndrome Hyperviscosity syndromes: o Cryoglobulinemia o Paraproteinemia o Waldenström macroglobulinemia Myasthenia gravis Thrombotic thrombocytopenic purpura (TTP) Wegener's granulomatosis Lambert-Eaton Syndrome
Plasmapheresis is a plasma donation not platelets
Question 28 Repeat – see q18
Question 29 a) T b) T c) F d) F e) F
Management of obstructive sleep apnoea: - weight reduction - avoidance of tobacco and alcohol - CPAP via nasal mask at night is effective - Surgical procedures include tonsillectomy, uvulopalatopharyngoplasty – UPPP, tracheostomy
Question 30 a) F b) T c) F d) ?? e) F eosinophilic granuloma of lung (histiocytosis X) - Neither inspiratory rales (crackles) nor clubbing is common.
Clubbing is a feature of CFA, not EAA.
Idiopathic pulmonary haemosiderosis is a disease mainly of children. Lympohangiomyomatosis – couldn’t find it.
31. A 32 year old former IV drug user presents with a several week old history of low grade fever, night sweats and shortness of breath. The following diagnoses are likely (f) pneumocystis carinii pneumonia (g) crytospiridosis (h) pneumococcal pneumonia (i) toxoplasmosis (j) pulmonary TB TFTFT Assuming that an IV drug abuser is now either immunosuppressed, or carrying a blood borne disease such as hep B/C. The question seems to be asking which of the following can cause respiratory complications of HIV/immunosuppression.
Pneumocystis carinii causes pneumonia in the immunosuppressed. It presents with a dry cough, fever and bilateral crepitations. Treat with co-trimoxazole. Prophylaxis is required if CD4 count is under 200. Cryptospiridium is a protozoa that can cause outbreaks of diarrhoea and abdominal pain from contaminated water supplies. It is self limiting in immunocompetent hosts but can be life threatening in the immunosuppressed (up to 20 litres of stool per day!). Pneumococcal pneumonia can also affect the immunocompromised and, presumably, it’s much worse. Toxoplasma gondi is the chief CNS pathogen in AIDS and it presents with focal neurological signs. Treat with primethamine (+folinic acid) and sulfadiazine or clindamycin for 6 months, with lifelong secondary prophylaxis. Pulmonary TB: see Oxford Handbook pp564-567.. TB will probably make an appearance on the MCQ is some form or another.
32. A 24 year old student present with jaundice three weeks after returning from a holiday in Mexico. The following make a diagnosis of Hepatitis A likely: (k) sharing needles (l) foreign travel (m) Incubation period (n) Recent blood transfusion (o) Extrahepatic manifestation FTTFF Hepatitis A is picornavirus which is transmitted via the faeco-oral route. Incubation period is 2-6 weeks. Prodromal features include fever, malaise, arthralgia. A patient with active infection will have anti-HAV IgM. IgG indicates old infection with no active disease. Once infection is established, treatment is supportive. 1-4% of patients will develop fulminany hepatitis and death from Hep A is rare (<1%). Chronic hepatitis does not occur. I have no idea what (e) means in this question.
33. A 61 year old male patient presents with renal colic and the following biochemistry results: Na+ 135 mmol/L, K+ 3.7 mmol/L, Urea 10 mmol/L, Ca++ 2.9 mmol/L, Total protein 95 g/L, albumin 28 g/L. The following are the most likely diagnoses: (p) Hypercalcemia of malignancy (q) Nephritic syndrome (r) Multiple myeloma (s) Sarcoidosis (t) Hyperparathyroidism
TFTFT Increased: Urea, Calcium, Total Protein. Decreased: Albumin.
Increased Urea: Drugs (cytotoxics, thiazides, pyrazinamide) Increased cell turnover Decreased excretion (primary gout, chronic renal failure, lead nephropathy, hyperparathyroidism, pre-eclampsia) Increased Calcium Malignancy, Hyperparathyroidism, Sarcoid, Vit D intox, Benign hypocalciuric hypercalcaemia (very rare) (Treat hypercalcaemia with rehydration and furosemide) Decreased Albumin Liver disease, Nephrotic synd, Burns, Protein losing enteropathy, malabsorption, malnutrition, late pregnancy, posture, genetic variations, malignancy.
I am unsure of these answers but here is my reasoning. Renal colic suggests stones and can occur with hypercalcaemia. a, c) Malignancy is consistent with all findings. Myeloma is definitely consistent with the raised total protein. b) Nephritic synd: Proteinuria and haematuria. Not renal colic and not hypercalcaemia. e) Hyperparathyroidism will cause the hypercalcaemia, hyperuricaemia and renal stones.
34 A 72 year old woman presents with recent chest pain, an uninformative ECG and an elevated troponin level. This indicates a. unstable angina b. dermatomyositis c. crush injury d. induction by exercise e. myocardial infarct
FFFFT Unstable angina will not cause a raised troponin.
From http://www.emedicine.com/emerg/topic932.htm The troponins are regulatory proteins found in skeletal and cardiac muscle. The 3 subunits that have been identified include troponin I (TnI), troponin T (TnT), and troponin C (TnC). The genes that code for the skeletal and cardiac isoforms of TnC are identical; thus, no structural difference exists between them. However, the skeletal and cardiac subforms for TnI and TnT are distinct, and immunoassays have been designed to differentiate between them. This explains the unique cardiospecificity of the cardiac troponins. Skeletal TnI and TnT are structurally different. No cross-reactivity occurs between skeletal and cardiac TnI and TnT with the current assays.
Elevated troponin levels have been documented in other disease states and situations that are not associated with atherosclerotic coronary artery disease, including the following: • Pacing, automated implantable cardioverter-defibrillator • Tachyarrhythmias • Hypertension • Myocarditis • Myocardial contusion • Acute and chronic congestive heart failure • Cardiac surgery • Renal failure • Pulmonary embolism • Subarachnoid hemorrhage • Sepsis • Hypothyroidism • Shock
35. Tuberculous cavitation on CXR: a. Is usually multiple b. Is usually thick walled c. May contain Nocardia d. Is usually in the mid/lower lobes e. Is low in bacteria count FTFFT Cavitation occurs in TB when the caseous material liquefies, is extruded out of the bronchi, and eventually liquefies. This is more common in secondary TB. Primary TB is classically charicterised by a calcified tubercle in the middle or lower zone (Ghon Focus) with a calcified perihilar lymph node (Ghon Complex). Secondary TB tends to involve the apices due to the higher O2 tension. Nocardia is an acid-fast gram positive rod. Infections are frequently misdiagnosed as TB as it is acid-fast and it causes the same disease process. Nocardia is inhaled and grows in the lungs to produce lung abscesses and cavitations. Treatment is with trimethoprim and sulfamethoxazole.
36. A 55 year old black US male has radicular chest pain. Serum Na+ is 122 mmol/L and ESR is 96 mm/hr. Which of the following are the likely diagnosis? a. dissecting aneurysm b. bony metastatic manifestation c. multiple myeloma d. spinal plasmacytoma e. sickle cell crisis FFTFF
The raised ESR would be consistent with myeloma, and renal insufficiency may cause hyponatraemia in that case. As for the others, I have no idea. Please email any corrections to this question to Ben because I can’t make sense of what’s going on.
37. In a patient presenting with dermatitis of the face and a previous history of atopic dermatitis, the appropriate therapy would include: a. dermovate b. emollients c. synalar d. betnovate e. hydrocortisone FTFFT Atopic dermatitis is treated with steroids and emollients. Low potency steroids are used on the face, ie hydrocortisone.
38. The following conditions should be treated with topical steroids a. Contact dermatitis b. Rosacea c. Acne d. Lichen planus e. Eczema herpeticum TFFTF Contact Dermatitis is treated the same as atopic dermatitis except there is the additional avoidance of the precipitant. Topical steroids and emollients are appropriate. Rosacea: Steroids are contra-indicated. Use metronidazole or tetracyclines. Acne: Treatment options: TOPICAL (benzoyl peroxide, retinoids, astringents, antibiotics) or SYSTEMIC (antibiotics, cyproterone acetate, isotretinoin, steroids). Lichen Planus: Potent topical steroids usually suppress irritation. Eczema Herpeticum: Widespread herpes simplex infection which occurs in atopic eczema. Lymphadenopathy and constitutional symptoms may occur. Steroids (used for atopic eczema) should be stopped until the eczema herpeticum has resolved. Treatment is with iv acyclovir.
39. In a 47 year old lady with disseminated breast carcinoma, dyspnea may be caused by: a. Lymphangitis carcinomatosa b. Pericardial effusion c. Massive ascites d. Superior vena cava obstruction e. Tamoxifen therapy TTTTF Lymphangitis carcinomatosa: LC occurs as a result of the initial hematogenous spread of tumor to the lungs, with subsequent malignant invasion through the vessel wall into the pulmonary interstitium and lymphatics. Tumor then proliferates and easily spreads through these low-resistance channels. Less commonly, direct infiltration occurs as a result of contiguous mediastinal or hilar lymphadenopathy or an adjacent primary bronchogenic carcinoma. The usual presenting complaint is of breathlessness in a patient with known malignancy. Occasionally, patients may have a dry cough or hemoptysis. Symptoms often precede the development of any radiographic abnormality. Pericardial Effusion: Causes – Bacteria, Fungi, MI, Dressler’s, Uraemia, RA, Myxoedema, Trauma, Surgery, MALIGNANCY, Radiotherapy, Procainamide, Hydralazine. Clinical Features – Dyspnoea, raised JVP. Massive ascites: This is unlikely to present with dyspnoea but it may be a cause of dyspnoea. SVC obstruction: Superior vena cava syndrome (SVCS) is characterized by gradual, insidious compression/obstruction of the superior vena cava (SVC). Although the syndrome can be life threatening, its presentation is often associated with a gradual increase in symptomatology. Dyspnoea is the most common symptom, followed by trunk or extremity swelling. Tamoxifen does not cause dyspnoea. Its main side effects are hot flushes and nausea.
40. A 48 year old dentist complains of fatigue for three months, and is found to have markedly elevated serum transaminase and bilirubin levels. Serum alkaline phosphatase is marginally elevated. The differential diagnosis includes: a. Gilbert’s syndrome b. Hepatitis C c. Drug induced hemolysis d. Primary biliary cirrhosis e. Biliary cholelithiasis FTFFF Gilbert’s: Asymptomatic isolated hyperbilirubinaemia which can be precipitated by fasting. Hepatitis C: Probably the most likely given the occupation that was given in the stem. Drug induced haemolysis: Would not raise AST and ALT, although it may be associated with gallstones. Primary Biliary Cirrhosis: Increased Alk Phos and GGT, mildly increased AST and ALT. Late disease will have and increased bili and PT with a decreased PT. Lethargy and pruritis may precede jaundice by months to years. 9 times more common in women, but I guess women can also be dentists. Alk Phos only being marginally increased make this unlikely. Biliary Cholelithiasis: Increased Alk Phos and GGT.
41. The following associations are correct: a. Primary hyperparathyroidism and high phosphate b. Primary hyperparathyroidism and MEN c. Secondary hyperparathyroidism and hypocalcemia d. Secondary hyperparathyroidism and hypophosphatemia e. Tertiary hyperparathyroidism and anemia FTTTF PTH increases Ca reabsorption and PO4 excretion.
MEN1: Parathyroid hyperplasia, Pituitary adenoma, Pancreatic tumours MEN2a: Medullary Thyroid Ca, Pheochromocytoma, Parathyroid hyperplasia MEN2b: Men2a + neurocutaneous signs –parathyroid hyperplasia.
Secondary hyperparathyroidism is secondary to hypercalcaemia. Chronic Renal failure is associated with anaemia and causes secondary (not tertiary, although may eventually) hyperparathyroidism.
42. Alport’s syndrome a. Is the most common hereditary nephritis b. Is due to a defect in the alpha-7 chain of type IV collagen c. Is a Y-linked disease d. Is associated with anterior lenticonus e. Is a contraindication to renal transplantation TTFTF Alport’s syndrome is X-linked dominant, aut dom, or rarely aut rec. Genes code for type IV collagen. Signs include progressive haematuric nephritis, sensorineural deafness and lenticonus (bulging of the lens capsule). Renal transplantation is the treatment of choice for ESRD in individuals with Alport syndrome. The results of renal transplantation for patients with Alport syndrome compare favorably with results in persons with other diagnoses.
43. The following are features of mitral stenosis a. A loud first heart sound b. Prominently displaced apex beat c. An opening snap soon after the heart sound suggests severe disease d. Graham-Steell murmur e. Giant v waves TFTTF
Palpation of the precordium reveals a quiet apical impulse. In pulmonary hypertension and RV hypertrophy, a RV parasternal lift may be encountered.
On auscultation, a loud S1 is present because the transmitral gradient holds the mitral valve open throughout diastole until ventricular systole closes the fully opened valve with a loud closing sound (S1). In advanced mitral stenosis, as the mitral leaflets become so damaged that they neither open nor close well, S1 eventually quiets.
S2 is physiologically split with a loud pulmonic component (P2) in the presence of pulmonary hypertension. S2 is usually followed by another early diastolic sound, called the opening snap (OS). The interval between S2 and the OS provides a good estimate of LA pressure and thus the severity of the mitral stenosis. When LA pressure is high, the OS closely follows S2 (0.06 s), but when it is normal, the OS occurs later (0.12 s), and it may mimic the S3 gallop. As mitral stenosis worsens, the S2-OS interval shortens.
The OS is followed by the characteristic low-pitched early-diastolic murmur. This murmur can be soft in patients with low cardiac output. In such patients, modest exercise, such as isometric handgrip, may increase the intensity of the murmur. A presystolic accentuation of the mitral stenosis murmur is also heard coincident with the atrial contraction. In the presence of pulmonary arterial hypertension, another diastolic murmur of blowing quality due to resultant pulmonary regurgitation (Graham Steell murmur) often becomes audible.
44. Cystic Fibrosis a. Results from a mutation in the CF transmembrane regulator b. Is characterized by a reduced transepithelial potential difference c. Shows significant clinical response to N-acetyl-cysteine d. Causes death prematurely principally from gastrointestinal complications e. In managed with aerosolized tobramycin to delay pulmonary exacerbations TFFFT
(b) This is all that I could find on potential differences: Potential difference (PD) (voltage) measured from nasal mucosa and the reading obtained by a reference electrode inserted into the forearm correlates with the movement of sodium across cell membranes, which is a physiologic function rendered abnormal by a CFTR mutation. The nasal potential difference (NPD) is a sensitive test of electrolyte transport that can be used to support or refute a diagnosis of CF. A normal mean value standard error (SE) is 0.9-24.7 mV; an abnormal value is 1.8-53 mV. When measurements are repeated after mucosal perfusion with amiloride to block an epithelial sodium channel, the drop in PD is greater in patients with CF (73%) than in control subjects (53%). Normally, subsequent perfusion with chloride-free solution and isoproterenol produces a sharp increase in the PD but has little effect when CFTR function is abnormal. As a result of the lack of commercially available equipment and the practical difficulties with NPD measurement, this test is performed in only a few research centers to diagnose CF in patients in whom making a diagnosis is difficult or a sweat test is not technically possible because of skin problems.
(c) While some patients benefit from mucolytics such as N-acetylcysteine, a universal benefit does not exist (http://www.emedicine.com/med/topic246.htm). (d) Premature death is primarily from respiratory complications. (e) Nebulised anti-pseudomonal antibiotics are thought to prevent recurrent exacerbations, reduce antibiotic usage and maintain lung function. (http://www.cysticfibrosismedicine.com/htmldocs/CFText/tobi.htm)
45. In Ulcerative Colitis a. Men and women are equally affected b. The rectum is generally spared c. The presence of pyoderma gangrenosum relates to disease activity d. There is an increased incidence of both large bowel and biliary carcinoma e. Elemental diets have a significant therapeutic benefit in acute relapse FFFTF
(a) No sex predominance (b) UC is generally considered to always affect the rectum, with contiguous involvement that can include the entire large intestine. (c) Pyoderma gangrenosum occurs in 1% of patients with UC. An indolent chronic ulcer may occur even when disease is in remission. Intralesional therapy with steroids is useful, and colectomy results in healing in approximately one half of patients. (d) UC is assoc with Primary Sclerosing Cholangitis, which has an increased risk of biliary carcinoma. UC also has a significant risk of bowel ca.
46. Renal artery stenosis: (a) False: Not sure, couldn’t find any literature to support either way, however, I would imagine that a relatively high percentage of those going for a peripheral angiography would have renal artery stenosis(arteriopathy), but not 50%. (b) True: The affected kidney often atrophies (c)False: Non cardiogenic flash pulmonary oedema is generally associated with severe B/L renal artery stenosis. Flash pulmonary oedema is acute onset pulmonary oedema of any cause. The treatment consist of management of the underlying condition(revascularisation of the kidneys) and direct treatment of the pulmonary oedema(O2, loop diuretic, nitrates, morphine) (d)True: The renin –angiotensin system is activated in the underperfused kidney which in turn leads to increased aldosterone. The aldosterone is responsible for decreased serum potassium. (e) False: Similar to coronary arteries – A stenosed coronary artery does not “always” progress to complete occlusion.
47. Heart sounds: (a) False: A loud S1 actually indicates a pliable valve therefore a soft S1 in mitral stenosis indicates severe disease. Other factors involved in assessing the severity of mitral stenosis are (a)early opening snap, (b) low volume pulse, (c) Signs of pulmonary hypertension eg, loud P2 (b) True: Splitting occurs in inspiration due to delay of closure of the pulmonary valve (P2). This is due to the increased volume load in the right ventricle from the negative intrathoracic pressure created. (c) True: LBBB will lead to reversed splitting of the Second heart sounds, ie, A2 occuring after P2 on full expiration. Incidentally, LBBB occasionally develops into complete heart block and/or sudden death, however more important factors are cardiovascular and systemic disease (d) True: Larger pressure gradients exist in the systemic circulation. (e) False: S3 occurs due to very rapid diastolic filling. Commonly described as a gallop rhythm it is heard loudest at the apex and on full expiration. Causes: Normal in children and young adults, High output states eg, pregnancy and thyrotoxicosis, Left ventricular failure, aortic regurg, mitral regurg.
48. Ulcerative Colitis: (a) True: Occurs more commonly than in Crohn’s disease (b) True (c) False: Associated with rheumatic fever (d) True: Also seen in Crohn’s disease, autoimmune hepatitis, Wegener’s and myeloma (e) The major cancer associated with UC is adenocarcinoma, however it is increasingly ackknowledged that lymphoma very rarely complicates UC. Make up your own mind
49. Chronic Liver Disease: (a) False: Although there is an increased total body sodium, there is a proportionately greater increase in the Extracellular fluid volume (b) False: Hepatoma aka hepatocellular carcinoma (c) True: TIPS (Transjugular Intrahepatic portosystemic Shunt) procedure is indicated in refractory variceal haemorrhage. It works by bypassing the diseased liver, thereby dramatically reducing the portal pressure. However, as the portal blood bypasses the liver, many toxic metabolites accumulate, thereby precipitating encephalopathy (d) True: As blood is digested, many toxic metabolites(eg, ammonia) overwhelm the diseased liver => encephalopathy (e) False: Quite the reverse
50. The following drugs are paired with common indications for their use: (a) True: The other main indications for ACE inhibitors are: Hypertension and diabetic nephropathy (b) False: Beta blockers may precipitate status asthmaticus. Several studies are examining the use of Beta blockers in asthmatics. Other C/I: 2nd and 3rd degree heart block, severe peripheral arterial diseasecardiogenic shock and prinzmetal’s angina (c) False: Indicated in paracetamol overdose. The treatment of TCA overdose involves Diazepam to prevent convulsions and correction of acidosis and hypoxia(IVI sodium bicarbonate) (d) False: Verapamil is indicated for arrhytmias whose origin is supraventicular. The treatment of VT involves amiodarone/lignocaine or if compromised – DC shock (e) True: Best treatment is control of the underlying malignancy, however bisphosphonates are often used. Calcitonin is used for refractory cases.
51. The following may cause falls in the elderly (a) True (b) True (c) True: postural hypotension (d) True: Medications are the most common cause of falls in the elderly (e) False: Increase the likelihood of fractures, not falls
52. On examination of the chest (a) False: If dull, consider; cosolidation(which may co-exist with hyperinflation), Collapse or pleural effusion. (b) False: Wheeze is due to airways narrowing. (1) polyphinic: suggests diffuse airways disease, eg, COPD, Asthma. (2) Fixed monophonic: Localized narrowing eg, bronchial carcinoma (3) Sequential inspiratory wheeze: Reopening of a collapsed airway eg extrinsic allergic alveolitis (c) True: Due to compression of the overlying lung. Features; the expiratory sound is louder, classically there is a gap between inspiration and expiration, hollow, blowing quality. Heard when turbulence from large airways are transmitted to the peripheries eg consolidation(Common), pleural effusion, collapsed lung. (d) False: Extrathoracic; During inspiration there is a relatively positive pressure acting on the trachea, therefore it is being “Squeezed” by the surrounding atmospheric pressure. (e) True: Provided it is a tension pneumothorax. Other causes; large pleural effusion, mediastinal mass
53. Immediately following an ischaemic stroke (a) False: However there are two instances when one should consider aggressive blood pressure management in a stroke patient, 1) Malignant hypertension, 2) Dissection of an artery eg, aorta, carotid (b) True: Rigidity develops over weeks o months. (c) True: Look for a cardiac cause eg, Atrial fibrillation, myocardial infarction (d) False: This is a controversial topic due to conflicting studies, however, a significant proportion of normal individuals have poor gag reflex. Conclusion: Absent gag alone would not be an indication, but would form part of the swallowing assessment. (e) True: Caveat; Exclude a haemorrhagic stroke
54. The following associations are correct (a) True: Battles sign consists of bruising behind the ears +/- CSF ottorhoea. From fracture of the petrous temporal bone. Associated with a dural tear. (b) True: Raccoon eyes +/- CSF rhinorhoea (c) False: Hydrocephalus can be loosely defined increased CSF in the cranium; resulting in enlarged ventricles and/sulci. This would not be consistent with a mass effect on the brain ieexternal pressure on the brain will actually decrease the space occupied by CSF. However, with resolution of a SOL, a space may remain due to cerebral atrophy – Hydrocephalus ex vacuo (d) True
55. Ulcerative Colitis (a) False: It is more common In non-smokers and in those with appendices(ie those who have not received appendectomies) (b) True: About 15% of those with pancolitis will develop colorectal carcinoma within 20 years. Also 20% of those who develop primary sclerosing cholangitis will develop cholangiocarcinoma (c) True: Backwash ileitis in the terminal ileum (d) False: Mucosal inflammation(mainly neutrophil), goblet cell depletion and crypt abscesses are histological features of UC (e) True
56. Breast carcinoma (a) True: provided it is part of the triple assessment for breast cancer: 1) Clinical assessment 2) Radiology; mammagraphy(women > 35 y/o), US(both diagnostic[women both > and < 35y/o] and to aid biopsy), MRI(useful in symptomatic patients with implants and also to detect local recurrence. 3) Histology; Fine needle aspirate or core biopsy. If there is any disparity between these three, an open biopsy is considered. (b) False: About 80% of Breast cancers are Ductule. Other types include invasive lobular, tubular, cribriform, mucinous and medullary. (c) False: Never ignore eczema of the nipple. Paget’s disease of the nipple is associated with invasive ductule carcinoma (d) True: Therefore assess Calcium and perform a skeletal survey.
57. Abdominal pain may be caused by (a) True: An atypical presentation (b) Mesenteric infarction: Classic triad of severe abdominal pain, no abdominal signs and rapid hypovolaemia. Exclude atrial fibrillation as a source of embolus (c) True: Especially acute intermittant porphyria( no cutaeneous manifestations).An acute attack can present with colicky abdominal pain, nausea and vomiting, thereby mimicking an acute abdomen. Cavé anaesthetics, as they can worsen the attack (d) True: Referred pain from pleural involvement (e) True: Pain in the loin radiating to the groin +/- fever and nausea.
58. Groin Lymphadenopathy (a) True: However the rectal lymphatics drain into the inferior mesenteric nodes (b) False: Cercix drains into iliac nodes while the body drains into the inguinal nodes. (c) False (d) True (e) True
59. Pulsus alternans (a) False (b) False: Likely to cause arrhythmias (c) True (d) True (e) False This is characterized by regular alternate beats that are both weak and strong. It is seen in severe myocardial failure and is due to prolonged recovery time of the myocardium. It also occurs with abnormal tachycardia – in this case it is a compensatory mechanism
60. Pericardial rub (a) False: A rub only occurs with inflammation of the pericardium (b) True (c) True (d) True (e) False
A pericardial friction rub is a scratching sound which may be heard in both diastole and systole. It’s intensity is altered by the posture of the patient, eg, it is often heard loudest when the patient is sitting up and breathing out. Cause: usually idiopathic(query viral infection?). Less common causes of pericarditis are a heart attack, a bacterial infection, an injury to the chest, radiation treatments for cancer, kidney failure, HIV infection, tuberculosis, autoimmune diseases such as lupus, or certain drugs.
61. (a) F-exam may be normal in pulmonary TB even if radiological abnormalities are present. Primary pulmonary TB infection is classically silent. (b) F-clubbing occurs due to complications of TB,e.g. bronchiectasis,not primarily due to the disease itself. (c) ?T-I can’t find a reference for this anywhere but TB is an inflammatory process so I assume it would be raised (d) T-Pulmonary TB, especially postprimary disease, nearly always causes abnormalities on the chest radiograph. Typically, the disease is parenchymal without nodal enlargement, and it manifests as cavitary lesions. Upper-lobe involvement with cavitation and the absence of lymphadenopathy are helpful in distinguishing postprimary from primary TB. Anterior or basal segments may be involved in as many as 75% of cases, in addition to the usually involved pulmonary segments, namely, the apical or posterior segments of the upper lobe or the superior segment of a lower lobe. (e) Pneumothorax may occur as a complication of TB infection. However, I can’t find any percentages for this
62(a) ? (b) ? (c) ? (d) ? (e) T
63(a) T- decreased production of gastric intrinsic factor,needed to bind B12 to facilitate absorbtion (b) T- causes decreased absorbtion of B12 in terminal ileum due to atrophy of intestinal mucosa (c) T- B12 deficiency causes a macrocytic anaemia with an increased MCV (usually >100fl) (d) T-similar mechanism to celiac disease (e) F-proximal small bowel resection should not affect B12 absobtion,terminal ileal resection, however, will greatly decrease the amount of B12 absorbed.
**I’m assuming this question was supposed to read vitamin B12 MALabsorbtion. If not, then just reverse my answers.
64(a) F-pupil is dilated due to failure of parasympathetic innervation. Pupil constriction occurs with ptosis as part of horner’s syndrome (partial ptosis ,miosis, anhidrosis & enopthalmos) due to failure of sympathetic innervation (b) T-due to the failure of the medial rectus muscle and the unopposed action of the lateral rectus muscle (c) T-ipsilateral ptosis due to damaged innervation to levator palpebrae (d) F-corneal reflx is mediated by CN5 (sensory/afferent) and CN7 (motor/efferent) (e)F-obviously
65(a) F- this occurs in subarachnoid haemorrhage (b) T-also alcoholics & patients on anticaogulants (c) T- very slight injury may precipitate a subdural haemorrhage (d) F-usually a venous bleed so HTN has little or no aetiological role (e) F-evacuation via a burr hole usually leads to full recovery (OHCM pp.366)
66. (a) T (b) T (pp.629 K&C) (c) F- there are elevated urea & creatinine levels (d) T (e) F
67 (a) F-sweating is common in hypoglycemia and the patient is usually warm & clammy (b) T (c) F (d) F-deep,irregular respiration (Kussmaul’s breathing) occurs in DKA (e) T
68 (a) T (b) ? (c) ? (d) T-sedatives & antidepressants may be causative factors in hypothermia (e) T- arrythmias & cardiac arrest in particular 69(a) T (b) T (c) F- the neutrophil count is decreased in brucella infection (d) T (e) T
70(a) T- pain may be referred and/or radiate from hip to knee and vice versa (b) ? T (c) ? (d) F-patellar tap is used to demonstrate the presence of a join effusion. A patello- femoral lesion can be examined for by sliding the patella sideways over the underlying femoral condyles. (e) F-usually worsens or first becomes symptomatic during pregnancy
71(a) F- incubation period of typhoid fever varies with the size of the infecting dose and averages 7-14 (range, 3-60) days (b) F- Most patients are moderately anemic, have an elevated erythrocyte sedimentation rate, thrombocytopenia, and relative lymphopenia. (c) T- At approximately the end of the first week of illness, about a third of patients develop bacterial emboli to the skin known as rose spots. These are considered a classic symptom in typhoid fever, but they occasionally appear in shigellosis and nontyphoidal salmonellosis. Rose spots constitute a subtle, extremely sparse (often <5 spots), salmon-colored, blanching, truncal, maculopapular rash with 1- to 4-cm lesions that generally resolve within 2-5 days. Relative bradycardia and a dicrotic pulse are also common during this stage of illness. (d) F- Constipation often develops early and is likely due to obstruction at the ileocecal valve by swollen Peyer patches. It may last for the entire duration of illness. In the third week, the patient commonly has pronounced abdominal distension & some individuals may produce liquid, foul, green-yellow diarrhea (pea soup diarrhea). During the incubation period, 10-20% of patients have transient diarrhea (enterocolitis) that usually resolves before the onset of the full- fledged disease. Young children and individuals with AIDS are more likely to have diarrhea that is probably due to blunted secondary immunity. The incidence of constipation versus diarrhea varies geographically, perhaps because of local differences in diet or S typhi strains or genetic variation. (e) T- Produces rapid improvement in patient's general condition, followed by defervescence in 3-5 d. Cures approximately 90% of patients. By the 1970s, widespread resistance to the drug developed. Ampicillin and co-trimoxazole became treatments of choice. However, in the late 1980s, some S typhi strains developed simultaneous plasmid-mediated resistance to all 3 drugs. Fluoroquinolones and third-generation cephalosporins have filled the breach, but some resistance exists to both.
72(a) F (b) F (c) T (d) T (e) ? BNF says KCl supplements can cause oesophageal or small bowel ulceration,but I don’t know if this applies to enteric coated preparations. I assume not but I can’t find a reference anywhere.
73(a) T-exposure may cause asbestosis and/or mesothelioma (b) F-I’ve never heard of painter&decorator’s lung! (c) T-exposure may cause berylliosis (d) ?T-Strongyloidiasis: Patients may report skin contact with sand or soil, abdominal pain or distension, and/or diarrhea, with or without immunocompromise. Marked wheezing and/or respiratory distress may occur (e) ?T- dust is a risk factor for occupational asthma but I can’t find a specific reference to cotton dust
74(a) T-low fibre diet and disordered colonic peristalsis are implicated in diverticular disease (b) F-pathophysiology of IBD is unknown,believed to be genetic or immunological in nature (c) F-I can’t find a link between these. (d) T- a high fat,low fibre diet is implicated in the development of colorectal ca. (e) F-contributing factors include exposure to nitrosamines in the environment or food, chronic ingestion of hot liquids or foods,cigarette smoking and chronic alcohol exposure, Plummer-Vinson syndrome, caustic injury to the esophagus, vitamin or nutritional deficiencies
75(a) T- The most frequent transfusion reactions are fever, chills, urticaria, or shortness of breath, which resolve promptly without specific treatment or complications (b) T-Nonimmune hemolytic transfusion reactions occur when RBCs are damaged prior to transfusion, resulting in hemoglobinemia and hemoglobinuria without significant clinical symptoms. (c) F (d) ? T -ARF is a rare complication of hemolysis and hemoglobinuria. Most often, it is associated with transfusion reactions (e)
76FTTFT Infectious mononucleosis=Glandular fever EBV infection 90% of adults were infected asymptomatically in childhood with EBV but infectious mononucleosis is symptomatic EBV infection usually in adolescents. EBV infects B-lymphocytes followed by T-Cell proliferation (mononucleosis), theses are cytotoxic to EBV infected cells. Glandular Fever Syndrome lymphadenopathy, prominent pharangitis and spleen is palpable in 50% of cases. Paul Bunnell/Monospot test is negative after 3 months. Abnormal LFT’s is commom, occasionally jaundice.
77FTFTT Mitral incompetence All left sided murmours are heard better on expiration LEFT EXPIRATION RIGHT INSPIRATION Auscultation: soft or absent S1 S3 pansystolic max at apex radiates towards axilla A gallop rhythm= S3 therefore MR may be associated with a gallop rhythm. Also indirect S3 is associated with cardiac failure and MR is associated with cardiac failure. Causes of MR: 1- intrinsic valve disease: rheumatic heart disease infective endocarditis myxomatous (connective tissue tumour) degeneration chordae tendinae rupture papillary rupture/dysfxn
2– functional due to left heart failure
78TTFFF The following are well recognized complications of therapy with ACE inhibitors: Dry cough First dose htn (esp if used in conjunction with heart failure where loop diuretics are also being used Taste disturbance Rashes Neutropenia Renal impairment and proteinuria Recommended in DM therefore think don’t cause serum lipids/blood glucose
79TFTTT The following drugs and their side effects are correctly paired Chloramphenicol causes aplastic anaemia Phenitoin causes osteomalacia since it causes a plasma calcium.
80FTFTT The following are known associations of rheumatoid disease Prolongued early morning stiffness Pericarditis ( uncommon)-10% having pericardial friction rub. Subcutaneous nodules on extensor surfaces/over bony prominces/in juxta-articular regions. Scleritis – pain especially on eye movement Pleural Effusion – may cause the right sided stony dullness.
81TTFFF Sjogrens syndrome Autoimmune disorder causing decreased saliva production-Dry mouth Mucous production and therefore physical resistance to inhaled pathogens and therefore RTI Tests for RA are positive in 50% Keratoconjunctivitis results from atrophy and fibrosis of lacrimal glands not ducts.
82TTTT Non-thrombocytopenic purpura and bruising may is bleeding for a reason other than platelets. Kala-azar = Visceral leishmaniasis(protozoa) which causes epitaxis. Since this epitaxis is due to capillary damage I’m assuming Kala- azar can cause non- thrombocytopenic purpura and bruising. Platelet storage pool disorder causes bleeding due to platelet aggregation and recruitment, normal no of platelets. Scurvy, capillary defect.
83TT(?) FFT Diabetes DM1 concordance 36% v’s DM2 concordance 60-100% Commonest cause of death in DM is Cardiovarcular disease- DM1=44%,DM2=52% DM need to insulin in times of infection to risk of DMKA. Lipohypertrophy is due to impure insulin causing a localized immune rxn, I don’t class this as an allergy, is this right? Cause of loss of warning of impending hypoglycaemia is autonomic neuropathy, warning with hypoglycaemic events.
84TFFTF Hypoglycemia Alcohol causes glucose consumption required to degrade and excrete alcohol. Thiazide diuretics can cause hyperglycaemia Influenza can cause hyperglycaemia. Unaccustomed exercise will cause an increase in energy/glucose consumption. IM has a slower rate of absorption and therefore will lower insulin availability and will cause hyperglycaemia??
85FFFTT Farmers lung Asthma Prevelence 10-15% general pop Farmers lung Prevelence rare general pop and farmers Shows non-caseating collection of histocytes ie. Non caseating granuloma Perihilar lympadenopathy is rare. Acute: Symptoms occur 4-6hrs post exposure although antibodies are present before and after symptoms. Responds well to steroids acutely and responds poorly in late stages.
86TFTT Asthma PEFR- classically morning dipping FRC- air in lungs at the end of tidal breath. From search think FRC is unaffected in Asthma ?? FEV-1 decreases in obstructive airway disease therefore I expect with bronchodilator. Transfer factor is vol of gas transferred between alveolar gas and pulmonary capillary blood-
87FFFF Case history In CRF need to match fluid intake with output therefore can’t say fluid requirement until know output. CRF rarely require protein restriction. I don’t think protein restriction would be “meddlesome” but not 100% ?? Requirement for renal replacement depends on progressive creatine over time so I can’t say when patient will require renal replacement therefore F.
88. TTTFF Reiters Syndrome Conjunctivitis, Arthritis, urethritis, can be uveitis associated Usually large joints – lower limb mono or oligoarthritis or enthesis (jxn of tendon+bone) doesn’t affect muscles! Chronic or relapsing Spondyloarthritides ie. Reiters syndrome – 83% HLA-b27 positive Can get sacroilitis and spondilits which cause constant pain and stiffness- can be worse in morning.
89. TTFTF Throtoxicosis
Thyroid eye disease is caused by autoimmunity and most common cause of thyrotox is Graves-75%. Since Graves is autoimmume-its most likely cause of thyroid eye disease. Eye signs may worsen with radio-iodine rx. Afib in thyrotoxicosis is usually treated by controlling rate and treating thyrotox. Use digoxin with caution in thyroid disease- BNF Absence of goitre makes graves unlikely but doesn’t exclude it. 90.TTTFF Hyperparathroidism phosphate reabsorption from kidney- hypophatemia Malignant Hyperthermia Hyponatremia
With mononeuritis complex you must rule out Goodpastures. Progressive membranoproliferative GN Malignant hypertension since didn’t find a connection on the web.
91. The following are associated with inflammatory bowel disease aCarcinoma of biliary tract T bPyoderma gangrenosum T cRenal calculi T dSeropositive arthritis F eSeronegative arthritis T
Cholangiocarcinoma in UC In Crohn’s and UC Oxalate calculi e)Anklylosing spondtlitis, Monoarthritis and Sacroileitis
Other associations during active phase Conjunctivitis Iritis Episleritis Mouth ulcers Fatty liver Liver abscess/Portal pyaemia Mesenteric or portal vein thrombosis Venous thrombosis Arthralgia Erythema nodosum Pyoderma gangrenosum
Associations unrelated to disease activity Autoimmune hepatitis Sclerosing cholangitis and cholangiocarcinoma (UC) Gallstones Renal amyloidosis and oxalate calculi Sacroileitis/Ankylosing spondylitis (Crohn’s with HLA-B27) Metabolic bone disease 92.Case history: male, heavy smoker, weight loss, cough, presents with weakness of quadriceps and anterior tibial muscles, absent knee and ankle jerk, flexor plantar responses, sensory loss in the saddle area, poor anal tone and weakness of knee extension. The likely diagnosis is: a.Transverse myelitis F b.S.A.C.D.C. F c.Radiculoneuropathy F d.Conus of the cord F e.Lesion of the cauda equine T
Inflammatory demyelinating disorder. Often flu like illness preceeding. In some patients it’s the first manifestation of MS. Acute/subacute paraparesis. It’s a flaccid paralysis so weakness and loss of reflexes. Ascending sensory level loss doesn’t fit above case. Subacute combined degeneration of the cord. Due to B12 deficiency. Absent ankle jerks due to neuropathy. Knee jerks may be absent or exaggerated due to cord lesion. Extensor plantar due to cord disease (UMN). Loss of vibration and proprioception due to involvement of the posterior columns. Sensory loss less common and mild. Saddle anaesthesia doesn’t fit Radiculoneuropathy. Disorder of nerve roots. Due to compressive lesions eg. Disc prolapse or tumours. L3, L4 Knee extension. Saddle area S3, 4, 5. Doesn’t fit Conus causes extensor plantar response plus absent knee and ankle jerks and altered saddle sensation Cauda Equina. Saddle anaesthesia. Decreased anal tone. Difficulty urinating. Progressive motor weakness/Gait disturbance. Sensory level. Flaccid and areflexic. Flexor plantar. Causes: Canal stenosis. Lumbosacral nerve lesions. Secondary malignancy (Breast, LUNG, PROSTATE)
In the valvular disease of the aortic valve a. The least common congenital abnormality is bicuspid valve F b. The more severe the stenosis becomes, the louder the murmur becomes T c. The aortic valve is at risk of bacterial endocarditis T d. The most likely cause of significant stenosis is rheumatic fever in early life F e. Sudden death may occur in aortic stenosis T
A) Most common B) Narrower opening means increased turbulence and therefore louder murmur. This is clinically unreliable. Murmur also gets shorter with increasing stenosis because greater pressures need to be generated to create blood flow. C) All valves at risk. BE in aortic valve results in valve damage and rergurg in some cases D) Most likely causes are senile degenerative and calcification of bicuspid valve. Rheumatic fever is a cause but not the most likely. E) Sudden death is rare but is more likely if other symptoms of stenosis have been prominent for a while. Which of the following are true of chest pain within the last 6 hours a. A man presenting with chest pain, less than 15 minutes duration, pressing pain, with normal ECG can be assured it is non-cardiac in origin F b.A man presenting with chest pain, 30 minutes, pressing pain, radiating to jaw and arm, with ST elevation on ECG, needs to be admitted to coronary care unit with view to thrombolysis T c. A man presents with chest pain, 30 seconds, pressing pain, with ST elevation on ECG, needs to be admitted to coronary care unit and given prophylactic lidocaine F d. He needs hospital admission F
A) This is a good plan if you don’t mind having your ass sued when he keels over and dies on the way out the door. Could be angina or loads of other stuff. B) More than 20 min suggest MI rather than angina. Morphine, Oxygen, Apsirin, Nitrates first. Thrombolysis is indicated for ST elevation MI. Prevents progression to Q wave transmural MI. Not indicated for non ST elevation eg. ST depression or T wave inversion. C) Lidocaine is given post MI to prevent ventricular arrhythmias. Not entirely certain he needs this after his 30 sec of chest pain but up to 30% of MIs are painless. Anyway it is not shown to reduce mortality when used prophylactically. (BNF P83) D) It depends on the history. I’d say no
Myelofibrosis is characterized by: a.Increased B12 F b.Often unproductive marrow aspirate T c.Decreased neutrophil alkaline phosphatase d.Leukoerythroblastic anemia T e.Folate deficiency is common T
A) Can’t find a reference to it so assuming its false B) The marrow is initially hypercellular with excess megakaryocytes. They release growth factor which results in proliferation of fibroblasts. Fibrosis makes it difficult to aspirate anything. They use a trephine biopsy instead. C) . D) Immature cells on blood film Reticulocytes and nucleated red cells and granulocyte precursors. Also tear drop poilikocytes and giant platelets E) Due to increased cell breakdown. Need supplementation
Marrow fibrosis, extramedullary hematopoiesis, Large spleen. White cell and platelet count can be low to high. Usually high at diagnosis (Soooo Helpful!) Urate high Presents with lassitude, weight loss and night sweats. Age over 50 96The following are true of duodenal ulcer a.Relapse rate is higher with campylobacter colonization F b.H2 blockers are only used short term F c.High dose antacids may heal ulcers F d.H2 blockers have been superceded by oxyprenolone F
A) Couldn’t find any info on it so assuming it’s false B) PPIs are preferred for long term use but there is technically nothing to stop the use of H2 blockers long term. C) According to the BNF liquid magnesium-aluminium antacids promote healing but less well than antisecretory drugs. Other books say antacids are crap and don’t heal ulcers. Prof Quigley said they don’t heal ulcers in his lecture so going with him on this one. D) What in the name of god is oxyprenolone. Its not in the BNF so going with false. I would say true if the said PPI
97The following are characterized by pustules a.Psoriasis vulgaris T b.Rosacea T c.DLE F d.Dermatitis herpetiformis F e.Erythema marginatum F A) If psoriasis vulgaris is the same thing as pustular psoriasis then this is true. 2 types. Generalised is very severe with swinging pyrexia. Localised affects palms and soles. B) Characterised by a papulopustular rash on cheeks, centre of forehead and chin. Treated with oral tetracycline C) Discoid lupus characterized by hyperkeratosis and follicular plugging. May cause scarring alopecia. D) Intensely itchy blisters over extensor surfaces of limbs and over the back. Linear IgA deposition at the dermoepidermal junction. E) Starts as red macules which fade at the centre but remain red at the edges. Associated with rheumatis fever.
98The following are worsened by sunlight a.Vitiligo T b.Rosacea F c.DLE F d.Psoriasis vulgaris F e.Seborrheic dermatitis F
A) Sunburn or trauma may precipitate. Melanocytes present but abnormal production of melanin. B) Photosensitivity is a differential but can’t find anything to say it’s a trigger C) Butterfly rash is photosensitive but not the discoid lupus as far as I can tell. D) Well UV light used in treatment so probably not. E) Caused by pityrosporum ovale infection. Can’t find a reference to it being worsened by sunlight
99The following are true of HLA-DR3 a.It is most specific for Graves disease ? b.It is of no value for connective tissue disordersF c.It is characteristic of celiac disease F d.It increased the relative risk of IDDM T e.It is associated with NIDDM F
A) HLA B8, DR 2 or DR 3. It is associated but is it the most specific? B) HLA B8, DR2 or DR3 in SLE C) HLA DQ2 D) HLA DR 3 and or 4 E) Can’t find a reference to HLA involvement in Type 2
100Myotonic dystrophy is characterized by a.facial weakness T b.frontal baldness T c.cataract T d.hypertrophic sternomastoids F e.proximal muscle weakness F A) Temporalis, Facial muscles, Sternomastoid B) And C) True but don’t know why. D) Muscle wasting E) Classically distal muscles
Autosomal dominant. Trinucleotide repeat on chr 19. Other features: Atrophy of testes and ovaries, cardiomyopathy, mild endocrine abnormalities and mental impairment. Die in middle age of intercurrent illness.
101Bloody diarrhea is characteristic of a.Cholera F b.Enteric (typhoid) fever F c.Amoebic dysentery T d.Schistosomiasis mansoni T e.Tropical sprue F
A) Severe painless diarrhea succeeded by vomiting. Then rice water diarrhea when normal gut content has been passed. Enormous fluid loss accompanied by cramps. No blood. B) 1st week fever, headache, myalgia, relative bradycardia, constipation, (diarrhea and vomiting in children) End of first week rose spots on the trunk, splenomegaly, ab distension, diarhoea, cough and epistaxis. Then bronchitis, delirium and other complactions coma and death if untreated. No reference to bloody diarrhea. C) Diarrhoea alternating with constipation. Sometimes mucus and streaks of blood. Offensive stool odour. May be tenderness along the line of the colon. D) Malaise, ab pain, frequent stools with blood stained mucus. May be hepatosplenomegaly. E) Chronic progressive malabsorption. PC Diarrhoea, ab distension, anorexia, fatigue, wgt loss. No reference to bloody diarrhoea
Causes of bloody diarrhea Campylobacter Shigella Non typhoidal salmonellae Enteroinvasive e coli Enterohaemorrhagic e coli Clostridium difficile Vibrio parahaemolyticus Entamoeba histolytica Diverticular disease Rectal or colonic malignancy IBD Bleeding haemorrhoids Anal fissure Ischaemic colitis Intussusception
102The following are associated with normal small bowel villous appearances on biopsy a.Gluten sensitive enteropathy F b.Irritable bowel syndrome T c.Post-gastrectomy steatorrhea T d.Tropical sprue F e.Pyloric stenosis T
Causes of subtotal villous atrophy Coeliac, Tropical sprue, Dermatitis herpetiformis, Lymphoma, AIDS enteropathy, Giardiasis, Hypogammaglobulinaemia, Radiation, Whipples, Zollinger ellison A) Subtotal villous atrophy with marked inflammatory infiltrate. B) Normal histology. All other investigations normal also. C) Steatorrhoea due to enzyme loss? D) Partial villous atrophy E) Can’t find reference to this assuming its false 103Pneumothorax a.Causes fever F b.Causes chest pain T c.Causes blood stained sputum F d.May be of sudden onset T e.May cause cyanosis T
A) Can’t find a reason why it would unless associated infection B) Sudden onset unilateral C) Can’t find a reason why it would D) Virtually always E) Tension pneumothorax with a mediastinal shift
Air in the pleural cavity. Spontaneous most common in males aged 15 to 30. Aetiology – smoking, height and sub pleural blebs. Secondary more common in older patients eg. COPD, TB, Asthma, lung abscess, pulmonary infarct, bronchogenic carcinoma lung fibrosis, CT disorders, sarcoid, trauma, iatrogenic.
104Polymyalgia rheumatica a.Causes shoulder girdle pain T b.Is associated with raised ESR T c.Steroids are often helpful T d.Patients rarely die of the disease T e.Can only be diagnosed on muscle biopsy F
A) This is classical with night pain and early morning stiffness. Also weight loss, fatigue, depression and night sweats B) ESR > 40mm/hr in majority C) Only effective treatment. Have dramatic response. If they don’t respond then it wasn’t PMR. Needed for up to 2 years. D) I wouldn’t have thought they died from this at all. So its either true that they rarely die or false because they don’t die from PMR at all. E) PMR is a clinical syndrome of muscle pain, stiffness and increased ESR. Other tests that could be done include CK which is usually normal and alk phos which is usually increased.
105The following are typical presentations a.Toxoplasmosis Choroiditis T b.Q-fever endocarditis T c.Leptospirosis Renal failure T d.Paget’s disease heart failure T
A) Retinochoroiditis. Mainly due to congenital but can arise in de-novo infection B) Q fever Fever, Myalgia, sweats, headaches, cough, hepatitis. If chronic suspect endocarditis. Not sure if endocarditis is therefore typical presentation. C) Fever, jaundice, headache, red conjunctiva, tender legs, purpura, haemoptysis, haematemesis, meningitis, myocarditis and renal failure. D) High output CCF, pain and enlargement of the skull, femur and clavicles, bowed tibia, pathological fracture, nerve deafness
106Third nerve palsy a.Is associated with small pupil b.May be viral c.Is characterized by inability to look down and out d.May be caused by a lesion of posterior cerebral artery e.Is associated with diabetes
Left Third Nerve “Surgical”, Dilated pupil, “Down & Out”
Answers Causes of third nerve palsy are diabetes, giant cell ateritis, syphilis, posterior communicating artery aneurysm, ‘coning’ of temporal lobe, midbrain tumor and infarction
Signs of Complete Third Nerve Palsy, 1. Unilateral complete ptosis 2. The eye facing down and out 3. A fixed and dilated pupil
Sparing of the pupil means that the pupil is of normal size and reacts normally. This is because the parasympathetic fibres that cause the pupil to constrict run in a discrete bundle on the surface of the Third Nerve and remains undamaged (unless they get squashed by tumor or aneurysm) . (a) False, associated with a large pupil if “Surgical” i.e. posterior communicating artery aneurysm, tumor, otherwise normal
(b) False
(c) False, the person can look down and out
(d) False, associated with posterior COMMUNICATING artery aneurysm
(e) True, any nerve in the body can be involved in diabetic mononeuritis. Isolated palsies of nerves to the external eye muscles esp. 3rd and Sixth are more common in diabetes
107The following are associated with their possible complications/associations a.Bronchial carcinoma cerebellar ataxia b.Brucellosis allergic alveolitis c.Bronchiectasis proteinuria and hepatomegaly d.Bullous emphysema jaundice+abnormal serum electrophoresis e.Fibrosiing alveolitis prominent a-wave on JVP
Answers
(a) True, non-metaplastic neurological complication . Other such complications are confusion, fits, cerebellar syndrome, proximal myopathy, peripheral neuropathy, polymyositis (symmetrical proximal muscle weakness from muscle inflammation), Eaton-Lambert syndrome (Myasthenia like syndrome that occurs with small cell lung cancer)
(b) False, Allergic alveolitis think Farmers Lung, Bird Fanciers Lung etc
(c) False, Bronchiectasis is used to describe abnormal and permanently dilated airways signs:- finger clubbing, coarse inspiratory crackles
(d) True, Caused by α1-Antitrypsin Deficiency. α 1- Antitrypsin is anti protease enzyme that inhibits neutophil elastase (nasty stuff made by white cells which destroy alveolar wall connective tissue leading to emphysema). Deficiency also leads to cirrhosis (hence jaundice), mechanism unknown. Genetic Variants are characterized by their electrophoretic mobilities as medium, slow or very slow.
(e) True, Fibrosing Alveolitis is characterized by inflammatory cell infiltrate and pulmonary fibrosis, of unknown cause. It leads to pulmonary hypertension and Cor pulmonale. A- wave on JVP due to atrial systole, Giant a waves occur when right atrial pressures are raised because of raised pressure in pulmonary circulation.
108Features of brucellosis include a.Phylectenular conjunctivitis b.Allergic alveolitis c.Lymphadenopathy
Answers Brucellosis is a gram negative bacterial infection, a zoonosis ( carried by your friendly domestic animal, vet and Kerry Farmer). Symptoms can be indolent and last for years- fever, sweats, malaise, anorexia, vomiting, weight loss, hepatosplenomegaly, constipation, diarrhea, myalgia, backache etc. Complications- Osteomyelitis, Infective Endocarditis, Abscesses, Meningoencephalitis. Diagnose with blood culture. Stuff them with Doxycycline and Streptomycin.
(a) False, Consists of multiple small yellow grey nodules near the limbus, this is associated with Tuberculosis (b) False, caused by inhalation of allergens, trying to confuse us with Berylliosis (lung fibrosis due to exposure to beryillium) the sneaky physicians.
(c) True
109Hypothermia (accidental) in the elderly a.Is frequently associated with shivering b.T3 should be used c.Rectal thermometer should be used d.Rapid rewarming is advised e.Is associated with bradycardia
Answers
(a)False, generally the elderly do not notice anything wrong, so do not try to warm themselves up, younger people do shiver
(b)False, only if hypothyroid, which can cause hypothermia, hence do thyroid function tests
(c) True, less than 35 Deg Cel. is definition of hypothermia, need to monitor rectal temperature during treatment (delegate to unfortunate junior staff member)
(d) False, rapid rewarming leads to peripheral vasodilatation and shock and death
(e)True
110The following abolish paroxysmal atrial tachycardia a.Valsalva manoevre b.Carotid massage c.Eyeball pressure d.Digoxin e.Beta blocker
Paroxysmal Atrial Tachycardia often comes on suddenly (paroxysmal) and causes a rapid heartbeat (tachycardia) from abnormal atrial electrical signals. The atria are above the ventricles, their position is often referred to as supraventricular; therefore, this condition may be called paroxysmal supraventricular tachycardia (PSVT). About half of patients with PSVT have no heart disease and simply generate abnormal signals because of other conditions, such as thyroid disease. Nicotine from smoking, caffeine, or stress may cause this condition. Adenosine used for diagnosis and treatment.
(a) True
(b) True, caution if possible digoxin toxicity, acute ischaemia or carotid bruit (c) False, facial immersion in cold water can be attempted to abolish rhythm, both used by the Bush administration to torture terror suspects
(d) True, however may be caused by digoxin toxicity hence do digoxin levels
(e)True, Calcium Channel blockers like Verapamil and Diltiazem can be used but never with beta-blockers
111A patient on an open ward demonstrates tubercle bacilli on several sputa. The following should be done a.Transfer patient to single room b.Incinerate all personal clothes c.Tell family it is unlikely they are infected d.Arrange skin tests and CXR for family contact e.Commence drug therapy before TB culture results available
Answers British Thoracic Society Guidelines
(a) True, as the patient is infectious via the aerosol route. Patients whose bronchial washings (Bronchoalevolar lavage, Dr Bredin’s Favourite & only hobby) are smear positive should be managed as if non-infectious unless (1) the sputum is also smear positive or becomes so after bronchoscopy, (2) they are on a ward with immunocompromised patients, or (3) they are known or suspected of having MDR-TB (Multi-drug resistant T.B.)
(b) False, not unless you own shares in your neighborhood incinerator. Marked crockery And separate washing up facilities are unnecessary, and no special precautions are needed for bed linen, books, etc. Sputum and other specimens should be incinerated along with whoever dreamed up this MCQ
(c)False, studies show one percent of close contacts get infected
(d)True, Investigations of contacts may include inquiry into symptoms of tuberculosis, BCG vaccination status, Heaf testing, and chest radiography.
(e)True, depending on facilities culture can take 4-8 weeks
112The following are complications of polycythemia rubra vera a.Acute gout b.Budd-chiari syndrome c.Stroke d.Hypercapnia e.Uveitis
Answers Ploycythemia Rubra Vera is a neoplasia of a clone from 1 multipotent cell which produces erythriod progenitor cells.
(a) True, due to increased cell turnover leads to increased uric acid production causing gout, hence Allopurinol is given to block uric acid production.
(b) True, Budd-Chiari Syndrome is Hepatic Vein congestion (e.g. thrombosis, tumor). The patient presents with acute epigastric pain and shock or portal hypertension. Typical causes are the pill, pregnancy related disease, malignancy and nocturnal haemoglobinuria. Also Polycythemia rubra vera, thrombophilia, causes of raised platelets.
(c) True, Increased risk of thrombosis (hyper-viscosity syndrome), hence put on low dose aspirin
(d) False, Normal blood gas. Polycythemia Rubra Vera is diagnosed by raised red cell mass (>125 of predicted with radioactive chronium) and splenomegaly in the presence of normal PaO2. Polycythemia may be secondary to hypoxia e.g. chronic lung disease or congenital heart disease.
(e) False, more likely to get visual disturbances and retinal haemorrhages
113The following have hematuria (microscopic/macroscopic) a.Steroid-sensitive but recurrent minimal change GN b.IgA nephropathy c.Nephropathy associated with diabetes d.Infective endocarditis e.Acute papillary necrosis
Answers
Causes of Haematuria
Renal Causes:-IgA nephropathy, glomerular nephritis, interstitial nephritis, polycystic kidney, papillary necrosis, medullary sponge kidney, infections (cystitis, pyelonephrirtis, TB, Schistosomiasis), Calculi, Neoplasia, Trauma, Vasculitis, Vascular Malformation
Extra-renal- Calculi, infection, neoplasia (bladder, prostrate, urethra), vasculitis, hypertension, sickle cell disease, trauma, cyclophospamide
Coagulation Disorders: - Hemophilia, anticoagulant therapy
(a) False, (b) True, (c) False (d) True, due to immune complex deposition, hence do urinalysis for work up of infective endocarditis (e) True
114A 55 year old woman is thought likely to have osteoporosis a.History of alcoholism would support the diagnosis b.History of thyrotoxicosis would support the diagnosis c.AP and lateral X-rays of spine are a sensitive indicator of disease progression d.Bone loss is mainly cortical rather than trabecular e.Vitamin D replacement is mandatory
Answers (a) True, other risk factors include Low BMI, family history of osteoporosis, early menopause, smoker, steroid usage, Cushing’s disease, hyperparathyroidism, hypogonadism
(b) True
(c) False, Plain X-rays only used for fractures due to osteoporosis, rubbish as an indicator of osteoporosis
(d) False, bone loss is trabecular in post menopausal osteoporosis, however cortical bone loss occurs as well in older patients (are we really expected to know this?)
(e) False, give where appropriate. (Note: - Calcium levels normal in osteoporosis)
115Psoriasis may cause a.Thimble pitting of nails b.Arthritis of distal interphalangeal joints c.Permanent scarring alopecia d.Cataracts e.Steatorrhea and malabsorption
Answers
(a)True, also show onycholysis (separation of the nail bed from the nail plate (b)True, less commonly causes seronegative rheumatoid-like joint changes, large joint mono or polyarthropathy and spondylitis(Inflammation of one or more of the vertebrae of the spine). (c)False (d)False (e)False, think dermatitis herpetiformis associated with celiac disease
116Endogenous eczema of the atopic type a.Itches in the majority of patients b.May cause weeping of the skin c.Often responds to topical corticosteroids d.Is often associated with hay fever and/or asthma e.Often involves limb flexures Answers
(a) True, intensely itchy (b) False, skin is dry (c) True (d) True, ‘atopy’ implies a genetic predisposition to develop eczema, asthma and hay fever. (e) True, tends to involve wrists, antecubital fossae, popliteal fossa and dorsa of feet
117Seborrheic eczema (seborrheic dermatitis) commonly involves a.Scalp b.Elbows and knees c.Sacrum d.Sternum and between scapulae e.Face Answers Seborrhoeic eczema is caused by the yeast Pityrosporum ovale (also called Malassezia) and the cutaneous immune response to it produces its characteristic inflammation and scaling i.e. itchy, diffuse scaling on an erythamtous background. No Cure, Topical Hydrocortisone used to treat. Ketoconazole shampoo and cream helpful.
(a)True, ‘cradle cap’ in babies (b)False, tends to affect flexures, more common in psoriasis (extensor surfaces) (c)False (d)True (e)True
118Griseofulvin is indicated in the treatment of: a.Candida infection of the nails b.Dermatophyte infection (trichophyton rubrum nail infection, tinea capitis/scalp ringworm) c.Paronychia d.Tinea versicolor e.Porphyria
Answers
Oral drug used in fungal infections esp. dermatophyte (jock itch (better known as ben thomson’s scratch disease), athlete's foot, and ringworm) when topical treatment has failed or is inappropriate. (a) False
(b) True
(c) False ( Paronychia is a chronic inflammatory process affecting the proximal nail fold and nail matrix, caused by Candida Albicans and/or bacteria, generally in people whose hands are immersed in water e.g. fishermen, housewives / house husbands etc)
(d) False, it is totally useless
(e) False, actually associated with acute attacks of pophyrias
119Carcinoma of the lip a.More often affects the lower lip than the upper lip b.Metastasizes early to the internal jugular lymph nodes c.Affects men more often than women d.Has a poor prognosis if it occurs at the angle of the mouth e.Is best treated by surgical excision
Answers
(a) True, tends to be squamous cell carcinoma with sun exposure the main aetiological factor, hence occurs on the lower lip in more than 90% of cases
(b)False, tends to metasistis primarily to the submandibular group of lymph nodes. To a lesser extent, drainage may go to submental, intraparotid, or internal jugular lymph nodes. Cervical lymphadenopathy detected clinically does not indicate lymph node metastasis. Any lymphadenopathy present is more likely to be inflammatory than metastatic. Only 60% with palpable lymphadenopathy will have metastasis.
(c) True, 6:1 male to female ratio
(d) True, lesions of the angle of the mouth are not biologically more aggressive, but it has been found that 82% recurred in the primary site. This is often because angle involvement results either from a large primary tumor or the clinician performs inadequate resection due to reconstructive considerations.
(e)True, treatment surgical with full thickness excision
120Malignant disease of a.The tonsil most commonly arises in lymphoid tissue b.The tongue can cause pain radiating to ear c.Nasopharynx may present with deafness d.The floor of the mouth is most commonly an ulcerating squamous carcinoma e.The buccal mucosa can arise in a patch of leukoplakia Answers
(a)False, most cancers arise from squamous cells, Lymphoma’s are the second most common.
(b) True, due to referred pain
(c)True, due to middle ear effusion
(d)True, squamous cell carcinoma accounts for 90 percent of tumors
(e)True, premalignant lesion, around 3% develop cancerous change
121. a.T b F c T in advanced cases paradoxical aciduria may develop d.F e F Plasma Cl is low due to loss of NaCl in vomit
Pyloric stenosis leads to a hypochloraemic hypokalaemic metabolic alkalosis. Because of the alkalosis H+ ions are moved out of cells in exchange for K+ ions and the renal excretion of H+ ions is decreased at the expense of increased renal excretion of K+ ions. Eventually hypokalaemia develops such that K+ needs to be conserved and this is done at the expense of excreting H+ ions, thus a paradoxical aciduria may occur in advanced cases.
122. a. F PTH increases Ca reabsorption in the kidney b. F PTH decreases PO reabsorption in the kidney c.T d.? e.?
123. a F this tests hypoglossal nerve function: deviates to side of lesion b F light reflex tests optic and occulomotor nerves c F d F trigeminal supplies sensation e T ask patient to wrinkle forehead, raise eyebrows, puff out cheeks, show teeth
124. a. T pinna is pushed down and forward b. T increasing deafness is a sign c ? F if perceptive deafness=sensorineural deafness d.T moving pinna is painful e.? it usually occurs in young children but I’m not sure about always
This is a complication of middle ear infection. Acute mastoiditis is the result of extension of acute otitis media into the mastoid air cells with suppuration and bone necrosis. Symptoms are: continuous and throbbing pain, otorrhoea and increasing deafness. Signs include pyrexia, general malaise, tenderness over the mastoid antrum and swelling in the postauricular area with the pinna pushed down and forward. The treatment involves general supportive treatment, antibiotics according to sensitivity and cortical mastoidectomy if not improving.
125. a F b F the frontal sinuses are not developed in early childhood thus frontal sinusitis is uncommon in the first decade of life c T usually occurs infants and small children d F e F
126. a F it is usually a fluctuant mass b T c ? Some books say it may move on swallowing but characteristically moves on protruding tongue d T thyroglossal cyst may develop anywhere along migration path of thyroid gland from base of tongue e F it is usually in the midline
127. a F b T patient complains of pain and there is tenderness over hernia c F d T this is a feature of intestinal obstruction e F patient may be anxious anyway for any reason
An irreducible hernia is one in which the contents cannot be manipulated back into the abdominal cavity. A strangulated hernia is one where the blood supply becomes compromised-firstly venous congestion, then arterial compromise eventually leading to gangrene and local peritonitis. The patient complains of pain and has features of intestinal obstruction. The hernia is tender, cough impulse is lost and there may be evidence of circulatory collapse and sepsis.
128. a F b F c T d T e T
Pancoast’s syndrome consists of apical lung cancer + ipsilateral Horner’s syndrome. There may also be shoulder or arm pain due to invasion of the brachial plexus and hoarse voice or bovine cough due to unilateral recurrent laryngeal nerve palsy and vocal cord paralysis.
129. a F There may be wasting of the THENAR eminence b T c F There may be paraesthesia in the median nerve distribution d F e T Phalen’s sign involves flexing the wrist and is positive if this results in paraesthesia or numbness within 1 minute, as can occur in carpal tunnel syndrome
130.Galeazzi’s fracture involves: a. F b. F c. T d. F e. F
Galeazzi’s fracture is a fracture of the shaft of the radius with distal ulna subluxation
131??? No answer given… 132. a. T b. F wasting of thenar eminence c. F d. F This occurs with paralysis of flexor digitorum sublemis
133. a. T Initial signs of an MI include distress, anxiety, pallor, sweatiness, tachycardia, hypotension 4th heart sound and signs of heart failure or a pansystolic murmur. Later a pericardial friction rub or peripheral oedema may occur b. T ventricular extrasystoles are the commonest post MI arrythmias c. T d. F this would increase the risk of thromboembolism e. F
134. a T b F Fluoroquinolones are considered the best treatment for typhoid eg ciprofloxacin c T penicillin by injection followed by oral treatment remains the treatment of choice for acute tonsillitis. It is recommended that treatment be continued for 10 days. But beware differential diagnosis includes infectious mononucleosis which if treated with ampicillin may provoke widespread rash d F Flucloxacillin is treatment of choice e T Amoxicillin 3g PO is recommended 1hour before dental procedures with no or local anaesthetic. If penicillin allergy alternative=clindamycin.
135. a F b T c T d T atpical TB e F
Aseptic meningitis is where CSF has cells but is gram stain –ve and no bacteria are cultures on standard media. Infective causes include: Viruses (eg echovirus, mumps, cocksackie, herpes, HIV, measles, influenza); partly treated bacterial meningitis; fungi; atypical TB; Lyme disease; leptospirosis; listeria; brucella; parasites. Non-infective causes can be malignant infiltration (eg leukaemia; lymphoma); drugs (eg NSAIDs); sarcoidosis; SLE; Behcets.
136Hypercalcaemia (a) May be present with polyuria – TRUE
Polyuria due to the effect of hypercalcaemia on renal tubules, ↓ing the concentrating ability – a form of mild nephrogenic diabetes insipidus
(b) Is an indication for steroid therapy in sarcoidosis – TRUE
Systemic prednisolone should be given to patients with involvement of the eyes or persistent hypercalcaemia
(c) May occur in myeloma – TRUE
Clinicopathological features of myeloma: Bone destruction – often causing #s of long bones or vertebral collapse (which can cause spinal cord compression) & hypercalcaemia Bone marrow infiltration – with plasma cells, resulting in anaemia, neutropenia, thrombocytopenia, together with production of paraprotein, which may (rarely) result in symptoms of hyperviscosity Renal impairment – owing to deposition of light chains in the renal tubules, hypercalcaemia, use of NSAIDs and (rarely) in patients who have had the disease for some time, deposition of amyloid (d) Causes QT interval prolongation on ECG – FALSE
Hypocalcaemia causes QT interval prolongation
(e) May require treatment with mithramycin - ?FALSE
Could only find the drug MITOMYCIN: Given IV to treat upper GI and breast cancers and bladder instillation for superficial bladder tumours
137Diabetes mellitus may give rise to a.Silent myocardial infarction – TRUE
b.Acute abdomen – TRUE
Medical causes of acute abdomen include: Referred pain – pneumonia, MI Functional GI disorders Renal causes – pelviureteric colic, acute pyelonephritis Metabolic causes – DM, acute intermittent prophyria, lead poisoning Haematological causes – haemophilia & other bleeding disorders, HSP, sickle cell crisis, polycythaemia vera Vasculitis – embolic
c.Renal papillary necrosis – TRUE
Common causes: reflux nephropathy, NSAIDs, DM, sickle cell disease or trait, cadmium or lead intoxication Uncommon causes: Alport’s syndrome, Balkan nephropathy & herbal nephropathy, irradiation, Sjogren’s syndrome, Hyperuricaemic nephropathy
d.Chronic hepatitis – FALSE
Causes of chronic hepatitis: Viral: Hep B +/- Hep D, Hep C Autoimmune Drugs: e.g. methyldopa, isoniazid, ketoconazole, nitrofurantoin Hereditary: Wilson’s disease Others: IBD – UC, alcohol (rarely)
e.Polyarthritis - FALSE
138The signs of hypopituitarism a.Hypotension – TRUE
Hypoadrenalism causes mild hypotension
b.Absent pubic and axillary hair – TRUE
Gonadotrophin deficiencies → loss of libido, loss of 2° sexual hair, amenorrhoea and impotence
c.Alopecia – TRUE
Underactivity of the thyroid, pituitary or adrenals can cause diffuse alopecia, as may hyperthyroidism
d.Extreme emaciation - ? FALSE
Weight may increase (due to hypothyroidism) or decrease in severe combined deficiency (pituitary cachexia) Emaciation = wasting of the body, caused by such conditions as malnutrition, TB, cancer or parasitic worms Cachexia = a condition of abnormally low weight, weakness, and general bodily decline associated with chronic disease. It occurs in conditions such as cancer, pulmonary TB and malaria
e.Small stature – TRUE
GH deficiency hay be relatively ‘silent’ except in children, but may cause marked impaired well-being in some adults
139Coronary artery disease may result from a.Syphilis b.Excessive iron therapy c.Temporal arteritis d.Pancreatic insufficiency e.Diphteria
140In the following circumstances, the physician should be aware of the possible presence of malignancy a.Polyposis coli – TRUE
Classification of colorectal polyps Type of Polyp Pathogenesis Polyposis Syndrome Adenoma Neoplastic FAP Juvenile Hamartoma Juvenile polyposis Peutz-Jeghers Hamartoma Peutz-Jeghers syndrome Metaplastic Unknown Metaplastic polyposis Lymphoid Hyperplasia Lymphoid polyposis Inflammatory Inflammation Inflammatory polyposis
b.Ulcerative colitis – TRUE
Patients with extensive UC of more that 10 years’ duration are at an increased risk of developing colorectal cancer. Although patients with Crohn’s colitis are also at risk, this is lower than with UC
c.Diverticular disease – FALSE
Not associated with malignancy Complications of diverticular disease include: - Perforation - Fistula formation - Intestinal obstruction - Haemorrhage - Mucosal inflammation
d.Pernicious anaemia – TRUE
There is a higher incidence of gastric carcinoma with PA than in the general population; the incidence in PA is 1-3%
e.Hypertrophic pulmonary osteoarthropathy – TRUE
Often associated with carcinoma of the bronchus
141A 75 year old male patient with gross painless haematuria a.Should have a rectal examination b.May have tuberculosis c.Should be reassured if JVP is normal d.Should be given vitamin K e.Is likely to have renal stones
142In fibrosis of the left upper lobe a.TB is the likely cause – TRUE
Causes of upper zone fibrosis include: Tuberculosis – associated with calcified areas and pleural thickening Sarcoidosis – hilar lymphadenopathy may also be present Radiotherapy – usually following treatment for carcinoma of breast Ankylosing spondylitis – fibrosis usually occurs when severe Chronic extrinsic allergic alveolitis
b.Trachea is deviated to the right – FALSE
Trachea will be deviated towards the side of the upper lobe fibrosis
c.Tactile vocal fremitus increased in the left apex – FALSE
Increased in consolidation
d.Apex usually displaced to left – TRUE
Displaced towards the side of the lesion
e.Hartman’s sign is diagnostic – ???
143The clinical features of acute hepatitis include a.Dislike of cigarettes – TRUE
b.Splenomegaly – TRUE
The spleen is palpable in 10% of cases of hepatitis A Other causes of splenomegaly: - Infections esp. infectious mononucleosis, septicaemia, bacterial endocarditis and malaria - Blood dyscrasis e.g. leukaemia (esp. CML), haemolytic anaemia, myelosclerosis, polycythaemia vera - Malignant lymphoma - Portal hypertension - Lipoid storage disease - Occasionally rheumatoid disease & SLE
c.Glycosuria – TRUE
There is a higher incidence of diabetes mellitus in hepatitis C
d.Anorexia – TRUE
e.Bilirubinuria – TRUE
Cholestatic jaundice → pale stools and dark urine
144The following statements are true a.Carpal tunnel syndrome is commonest in middle aged females – TRUE More common in women but middle aged?
b.Pretibial myxoedema is seen in thyrotoxicosis – TRUE
This is a feature of thyrotoxicosis due to Graves’ thyroiditis
c.Cushing’s syndrome in females usually gives rise to amenorrhoea – ?TRUE
Cushing’s syndrome can cause amenorrhoea or oligomenorrhoea in females but not sure if it usually does
d.Acromegaly may give rise to hypertension - TRUE
e.Calcified ascending aorta on x-ray suggests syphilis – TRUE
Aortic-wall calcification occurs in syphilitic aortitis (ascending aorta)
145Diuretic therapy a.May precipitate hepatic Encephalopathy – TRUE
In hepatic failure hypokalaemia caused by diuretics (thiazide and loop diuretics) can precipitate encephalopathy, particularly in alcoholic cirrhosis Diuretics may also increase the risk of hypomagnesaemia in alcoholic cirrhosis, leading to arrhythmias Spironolactone, a K+ sparing diuretic, is chosen for oedema arising from cirrhosis of the liver
b.May cause secondary gout – TRUE
Uric acid levels in the blood are often increased because thiazides are secreted by the organic acid secretory system in the tubules and compete for uric acid secretion. This may precipitate gout (also occurs with loop diuretics)
c.May cause collapse in elderly patients – TRUE
Loop diuretics may cause hypotension leading to collapse
d.Should not be prescribed for patients with diabetes mellitus – FALSE
Diabetes mellitus is not a contraindication to the prescription of diuretics 146Erythema multiforme a.May have associated oral lesions – TRUE
Involvement of the oral, conjunctival and genital mucosae is not uncommon and, if extreme, is known as the Stevens-Johnson syndrome When there is severe mucosal involvement = Erythema multiforme major Without mucosal involvement = Erythema multiforme minor
b.Is a vasculitic eruption seen in rheumatic fever – FALSE
The dermatological manifestations of rheumatic fever include: Subcutaneous nodules: small, mobile painless nodules on extensor surfaces of joints and spine Erythema marginatum: geographical-type rash with red, raised edges and clear centre; occurs mainly on trunk, thighs, arms
Causes of erythema multiforme: Idiopathic 50% of cases (no cause found) Viral Herpes simplex, hepatitis B, orf, adenovirus, Mumps, mycoplasma Bacterial Streptococci Fungal Coccidoidomycosis, histoplasmosis Drugs Antibiotics, phenytoin, NSAIDs Other LE, pregnancy, malignancy
c.May be very toxic and require steroid therapy – FALSE
Systemic steroids are often prescribed to moderate the acute symptoms, although it is debatable whether they affect the outcome and may ↑ mortality
d.Is frequently seen in amyloidosis – FALSE
e.May be fatal – ? FALSE
147Acute myocarditis a.Is usually viral in origin – TRUE
Viruses include coxsackie virus, adenovirus, CMV, echovirus, influenza, polio, hepatitis, HIV
b.May be produced by steroid therapy – FALSE Drugs causing hypersensitivity reactions, e.g. methyldopa, penicillin, sulphonamides, antituberculous may cause acute myocarditis
c.Produces T-wave abnormalities on ECG – TRUE
ECG demonstrates ST and T wave abnormalities and arrhythmias
d.May result in ventricular dysrhythmias – FALSE
Atrial arrhythmias
e.Frequently shows Bell’s sign – ???
148Rheumatoid disease a.May lead to impotence – FALSE
b.Usually requires steroid therapy – FALSE
They are powerful disease-controlling drugs, but are best avoided in the long term because side effects are inevitable
c.May involve temperomandibular joints – TRUE
25% of cases of rheumatoid arthritis involve the TMJ
d.Occasionally leads to hypersplenism – TRUE
Hypersplenism can result from splenomegaly due to any cause. It is commonly seen with splenomegaly due to haematological disorders, portal hypertension, RA (Felty’s syndrome) and lymphoma. Hypersplenism produces: - Pancytopaenia - Haemolysis due to sequestration and destruction of red cells in the spleen - ↑ed plasma volume
1% of patients with RA have Felty’s syndrome
e.May affect the lungs – TRUE
Pulmonary manifestations of RA: Fibrosing alveolitis Pleural nodules Pleuritis Serositis causing pleural effusions Obstructive bronchiolitis
149Acute nephritis is a recognised feature of the following disease a.Brucellosis – FALSE
May cause: - Bone and joint infection: esp. sacroilitis and spondylitis - Respiratory infection: bronchitis, abscesses - Acute or chronic meningitis - Rarely endocarditis, genitourinary infection (?)
b.Ankylosing spondylitis – FALSE
c.Polyarteritis nodosa – FALSE
Aneurysmal dilatation of medium-sized arteries may be seen on renal arteriography Associated with slowly progressing renal failure
d.Polyposis coli – FALSE
e.Bacterial endocarditis – TRUE
Acute renal failure may occur from immune complex disease, haemodynamic upset (acute heart failure), damage during cardiac surgery and nephrotoxic antibiotics