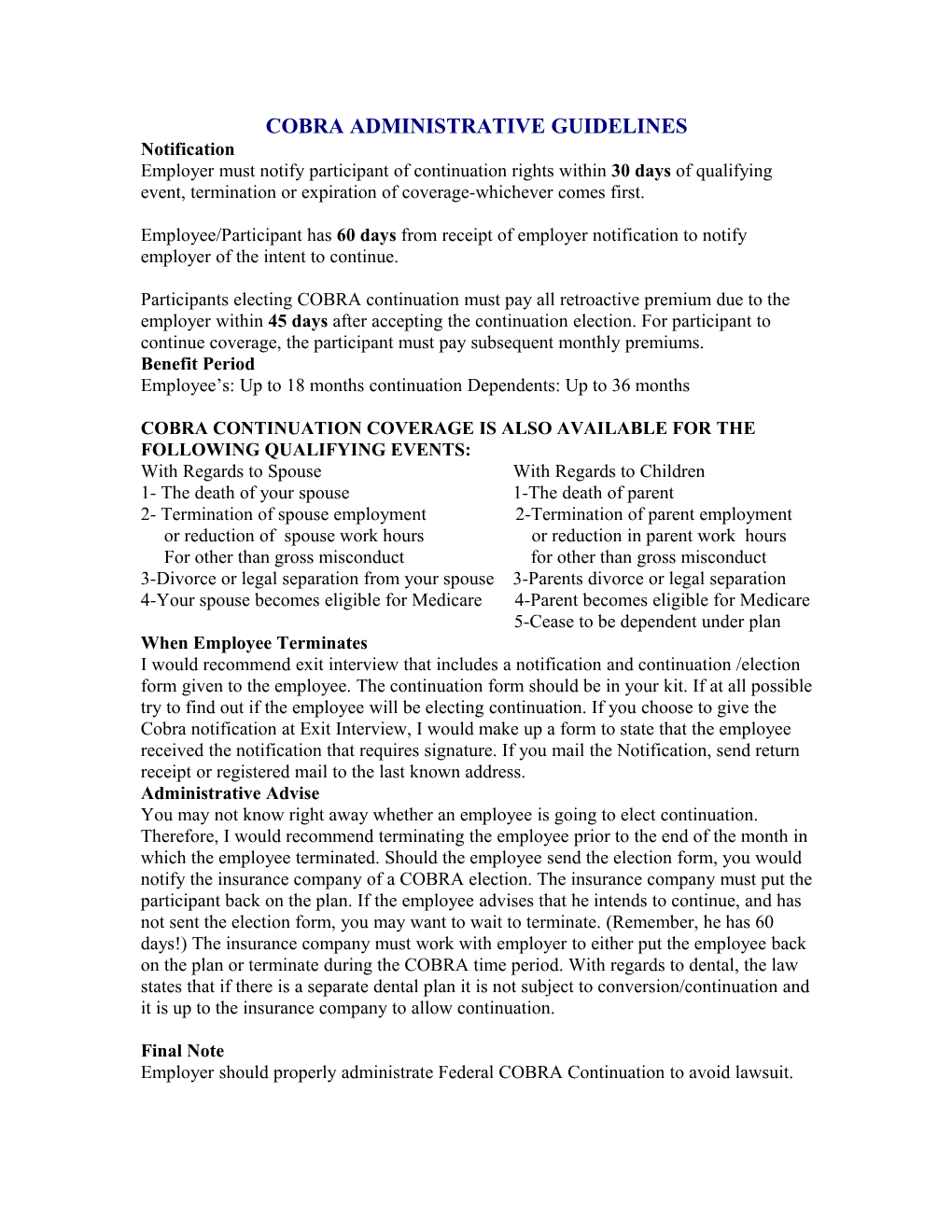
COBRA ADMINISTRATIVE GUIDELINES Notification Employer must notify participant of continuation rights within 30 days of qualifying event, termination or expiration of coverage-whichever comes first.
Employee/Participant has 60 days from receipt of employer notification to notify employer of the intent to continue.
Participants electing COBRA continuation must pay all retroactive premium due to the employer within 45 days after accepting the continuation election. For participant to continue coverage, the participant must pay subsequent monthly premiums. Benefit Period Employee’s: Up to 18 months continuation Dependents: Up to 36 months
COBRA CONTINUATION COVERAGE IS ALSO AVAILABLE FOR THE FOLLOWING QUALIFYING EVENTS: With Regards to Spouse With Regards to Children 1- The death of your spouse 1-The death of parent 2- Termination of spouse employment 2-Termination of parent employment or reduction of spouse work hours or reduction in parent work hours For other than gross misconduct for other than gross misconduct 3-Divorce or legal separation from your spouse 3-Parents divorce or legal separation 4-Your spouse becomes eligible for Medicare 4-Parent becomes eligible for Medicare 5-Cease to be dependent under plan When Employee Terminates I would recommend exit interview that includes a notification and continuation /election form given to the employee. The continuation form should be in your kit. If at all possible try to find out if the employee will be electing continuation. If you choose to give the Cobra notification at Exit Interview, I would make up a form to state that the employee received the notification that requires signature. If you mail the Notification, send return receipt or registered mail to the last known address. Administrative Advise You may not know right away whether an employee is going to elect continuation. Therefore, I would recommend terminating the employee prior to the end of the month in which the employee terminated. Should the employee send the election form, you would notify the insurance company of a COBRA election. The insurance company must put the participant back on the plan. If the employee advises that he intends to continue, and has not sent the election form, you may want to wait to terminate. (Remember, he has 60 days!) The insurance company must work with employer to either put the employee back on the plan or terminate during the COBRA time period. With regards to dental, the law states that if there is a separate dental plan it is not subject to conversion/continuation and it is up to the insurance company to allow continuation.
Final Note Employer should properly administrate Federal COBRA Continuation to avoid lawsuit.