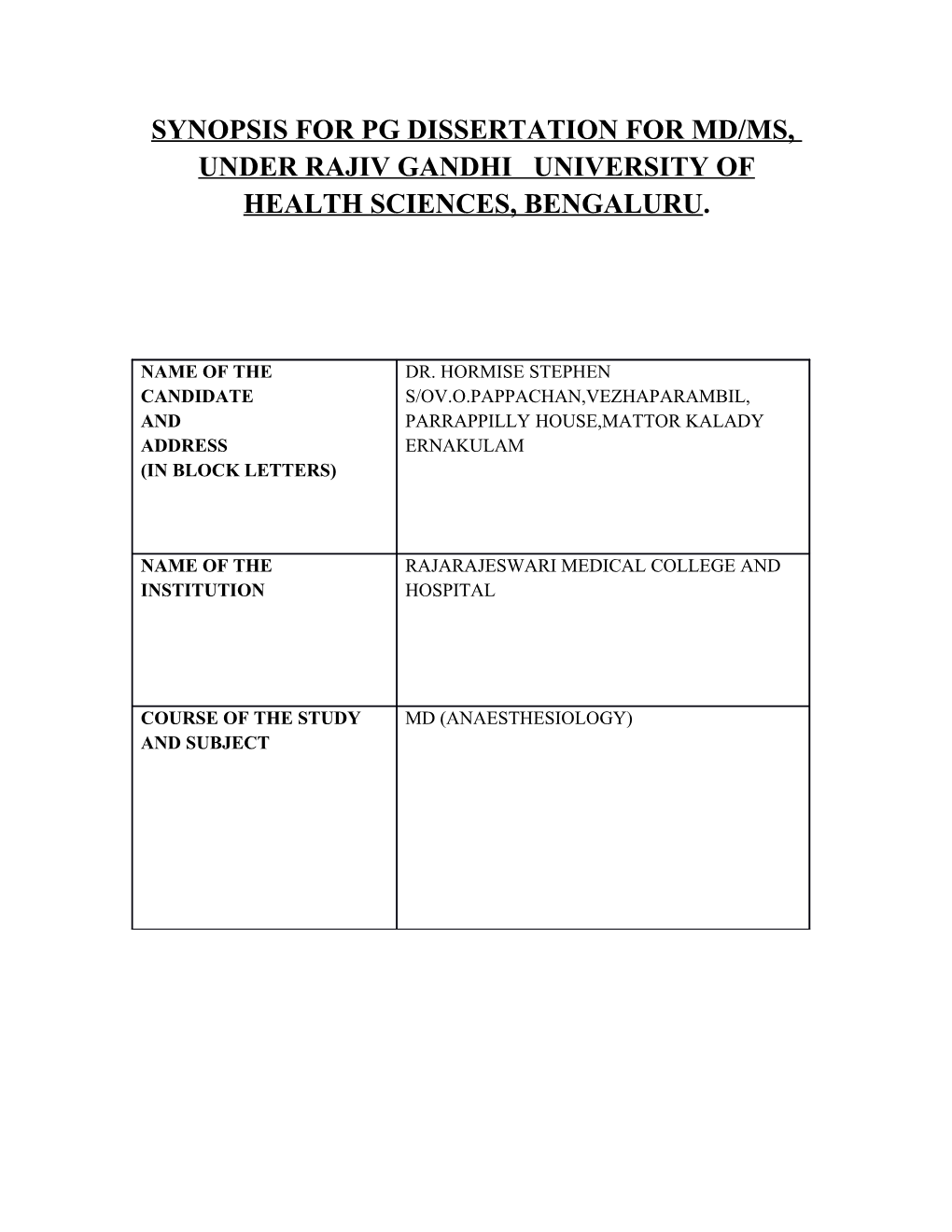
SYNOPSIS FOR PG DISSERTATION FOR MD/MS, UNDER RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BENGALURU.
NAME OF THE DR. HORMISE STEPHEN CANDIDATE S/OV.O.PAPPACHAN,VEZHAPARAMBIL, AND PARRAPPILLY HOUSE,MATTOR KALADY ADDRESS ERNAKULAM (IN BLOCK LETTERS)
NAME OF THE RAJARAJESWARI MEDICAL COLLEGE AND INSTITUTION HOSPITAL
COURSE OF THE STUDY MD (ANAESTHESIOLOGY) AND SUBJECT RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES KARNATAKA BANGALORE
ANNEXURE -1
SYNOPSIS SUBMISSION MD ANAESTHESIOLOGY RAJARAJESWARI MEDICAL COLLEGE AND HOSPITAL BANGALORE-560074
SYNOPSIS TOPIC:-
“ A COMPARATIVE STUDY OF RESPIRATORY MECHANICS AND HEMODYNAMIC STABILITY IN PATIENTS UNDERGOING LAPAROSCOPIC SURGERY: PROSEAL LARYNGEAL MASK AIRWAY VERSUS THE I-GEL”
BY:- Dr.HORMISE STEPHEN DEPARTMENT OF ANESTHESIOLOGY RAJARAJESWARI MEDICAL COLLEGE, BANGALORE - 560074
GUIDE NAME:-
Dr. SAHAJANAND.H PROFESSOR & HOD DEPARTMENT OF ANESTHESIOLOGY, RAJARAJESWARI COLLEGE AND HOSPITAL BANGALORE-567004
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA BANGALORE ANNEXURE – II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
: Dr.HORMISE STEPHEN Name of the candidate and DEPARTMENT OF ANESTHESIOLOGY 1 address ( in block letters) RAJARAJESWARI MEDICAL COLLEGE, BANGALORE - 560074 : DR. HORMISE STEPHEN Permanent address S/O V.O.PAPPACHAN,VEZHAPARAMBIL, PARRAPPILLY HOUSE,MATTOR KALADY ERNAKULAM
: RAJARAJESWARI MEDICAL COLLEGE, 2 Name of the institution BANGALORE– 560074
3 Course of study and subject : M.D. (Anesthesiology) Date of admission to the : 4 30thMay 2012 course : A comparative study of respiratory mechanics and hemodynamic stability in patients undergoing laparoscopic 5 Title of Topic surgery: Proseal Laryngeal mask airway versus the I-Gel
6 Brief Resume of the intended work 6.1 Need for the study Laparoscopic surgery cause changes in respiratory mechanics following carbondioxide pneumoperitonium. The pulmonary compliance is decreased and the resistance is increased leading to high airway pressure.Therefore higher inspiratory pressures are required to provide adequate tidal volume and minute ventilation.1 intra-abdominal pressure of 15-20mmHG is associated with increase in the peak airway pressure of about 50%.decrease in lung compliance by 25% and increase in PaCo2 by 10% ,leading to inadequate ventilation, gastric insufflations, increase risk of regurgitation, and subsequent pulmonary aspiration3-4. The Proseal larangeal mask airway(PLMA) and I-gel are two supraglotic airway devices introduced in 2000 and 2007. These devices provides higher oropharangeal seal pressure than the classic laryngeal mask airway,have a additional drain tube and have been designed for use with spontaneously as well as positive pressure ventilation5-6. The Proseal LMA has been used as a alternative for tracheal tube for many laparoscopic surgeries9-10.The aim of study is to compare the respiratory mechanics and hemodynamics using either the PLMA or i-gel in adult patients undergoing laparoscopic surgery. 6.2 Review of Literature
Pelosi P,Foti G. concluded that laproscopic surgeries cause abdominal carbondioxide insufflation which leads to reduction in compliance of respiratory system and functional residual capacity, a marked increase in the resistance of respiratory system no change in oxygenation.an increase in end tidal carbon dioxide tension and that these changes were not affected by the duration of anesthesia.1
Levitan R M ,Kinkle W studied the positioning and mechanics of this new device I-gel in 65 non-embalmed cadavers with 73 endoscopies,16 neck dissections, and six neck radiographs in each of the neck dissections and radiographs the bowl of the device covered the laryngeal inlet. They found that despite of the lack of an inflatable cuff i-gel achieved proper positioning for supraglottic ventilation2.
In a preliminary crossover study by by Brain A L, Verghese C comparing Proseal LMA with the standard mask in 30 adult female patients showed no difference in insertion, trauma, or quality, of airway, At 60cmH2o intracuff pressure, the new LMA gave twice the seal pressure of the standard device and permitted blind insertion of a gastric tube in all case. He concluded that Proseal LMA reduces the risk of gastric insufflation and pulmonary aspiration and thus merits further study.5
In a study done by Brimacombe J, Keller C concluded that PLMA achieves a more effective seal than i-gel and PLMA facilities gastric tube placement but an introducer tool is necessary for insertion.7
In another study done by Uppal V, Fletcher G, there was no significant difference between the leak fraction of the I-gel and the tracheal tube at 15 and 20cm H2o during pressure controlled ventilation. He found that I-gel can be used as an alternative to tracheal tube during pressure controlled ventilation with moderate airway pressure.8
Dumontl ,Mattys studied respiratory mechanics and arterial blood gases in 15 morbidly obese patients undergoing laparoscopic gastroplasty under general anaesthesia and controlled ventilation. He concluded that on studying the intraoperative respiratory mechanics, laparoscopic surgeries are safe in obese patients under general anesthesia with controlled ventilation.10
In a study by Schmidbauer W. three supra laryngeal airway devices were inserted into eight unfixed cadaver models with exposed esophagus that had been connected to a water column producing both a slow and a fast oesophageal pressure increase. He concluded that PLMA provides a better seal of oesophagus than i-gel and that tracheal aspiration may be prevented with their use11
6.3 Objectives of the study
1)To Compare the respiratory mechanics and hemodynamic stability of Supraglottic airways I-gel and Proseal LMA.
2) Oropharyngeal leak pressure
3)Any device related adverse events.
7 Materials and methods 7.1 Source of data
Study will be conducted on 60 patients undergoing laparoscopic surgery in Rajarajeshwari Medical College and teaching hospital, Bangalore for 18 months.
7.2 Methods of collection of data ( including sampling procedure, if any)
A Comparative, Randomized, 2Arm(Group), Open Label Clinical Anesthesia study will be conducted on 60 adult patients undergoing laparascopic Surgery in Rajarjeshwari Medical College and Teaching Hospital, Bangalore. Sampling Method: Simple Random Sampling. Using computer generated table. The duration of study will be of 18 months i.e. from November 2012, to April 2014
Inclusion criteria
Patients aged between 20 to 60 years of either sex ASA I or ASA II scheduled for elective laparoscopic surgery, with either PLMA or I-gel as airway device.
Exclusion criteria Patients with upper respiratory tract infection, Anticipated difficult airway with mouth opening less than 2.cm, Hiatus hernia,GERD disease, History of Hypertension, Diabetes,Bronchial Asthma,or Heart Disease. Lack of Patient Consent, History of allergy to one or more drugs.
Study design, sample size and sampling methods.
This randomized prospective study will be carried out on 60 adult patients of ASA physical status I and II, scheduled for laparascopic surgeries. After the approval by the institutional Ethical Committee, written informed consent will be obtained from all the patients before being included in the study.They will be randomly allocated to following groups of 30 each: Group P: patients will receive PLMA Group I: Patients will receive I-Gel All patients will receive Tab.Diazepam 5mg orally,Tab.Ranitidine 150mg on the night before surgery. Before arriving, at the operation room a18-gauge peripheral venous cannula will be inserted and according to study protocol all patients will be prehydrated with 500ml of Lactated Ringer solution. Premedicated with Inj.midazolam 0.04mg/kg and 0.2mg of glycopyrrolate intravenously. In the O.R. base line readings of Heart Rate(HR) , Systolic Blood Pressure(SBP), Diastolic Blood Pressure(DBP), Mean Arterial Pressure(MAP), Oxygen Saturation(Sa02), and End Tidal CO2(ETCO2) will be measured The measurements of HR, SBP, DBP, MAP, ETCO2 will be taken at intervals of 1, 3, and 5minutes will be recorded. Patients will be induced with 2.5% of Inj. Thiopentone4-6mg/kg (sleep dose) and depth of anesthesia will be monitored by loss of eyelash reflexes. Inj. Vecuronium 0.1mg/kg will be administered. After mask ventilation for three minutes,the appropriate sized airway device will be inserted . Effective ventilation with device was defined as a square wave capnogragh trace and bilateral chest movements on manual ventilation. Patients will be maintained with 33% of oxygen in nitrous oxide, isoflurane and vecuronium in divided doses. Peroperative analgesia was provided with InjFenatyl 1-2 mcg/kg.The tidal volume and respiratory frequency will be adjusted and intermittent positive pressure ventilation (IPPV)will be continued by mechanical ventilator to maintain end tidal carbon dioxide level between 35-45 mm Hg. Pneumoperitonium will be created by insufflations of carbon dioxide and operation table will be tilted 15 degree reverse trendelenburg position. Intra abdominal pressure was not allowed to exceed 15 mm Hg throughout the surgery. The oropharangeal seal pressure was determined by closing the expiratory valve of the circle system at a fixed gas flow of 5 liters and the air way pressure at which equilibrium was reached.the presence of gas leak at seal pressure was detected as an audible sound escaping from the mouth or by the gel displacement test. The following respiratory data will be monitored at the following time points: 1,5 and 10 minutes after insertion of device, after pneumoperitonium at 5,15 ,45, 60,90 and 120 minutes. Dynamiccompliance, Peak airway pressure The measured minute volume Any regurgitation of fluid through the gastric channel or airway tube will be noted. Heart rate(HR),non-invasive Systolic blood pressure(SBP),Diastolic Blood pressure(DBP),Mean arterial blood pressure (MAP), oxygensaturation (SpO2),end tidal carbon dioxide(EtCO2) will be recorded at 1,5 and 10 minutes after insertion of device, After pneumoperitonium at 5,15 ,45, 60,90 and 120 minutes and after removal of device. At the end of surgery residual neuromuscular block will be reversed with appropriate dose of Inj.neostigmine and Inj. glycopyrrolate intravenously. After reversal patients will be monitored in the post anesthesia care area.
Complications such as incidence of any airway complications caused by supraglottic devices. Post-extubation cough, breath holding or laryngospasm, Presence of blood on the I-gel or LMA Lip and dental injury.
5. Each patient will be questioned to determine any of the following complications (in recovery room and 24 hours postoperatively): Sore throat (constant pain, independent of swallowing), Dysphagia (difficulty or pain with swallowing), Dysphonia (difficulty or pain with speaking), Numbness of the tongue or the oropharynx,
The changes in the respiratory mechanics between two groups were our primary outcome measure and the oropharyngeal leak pressure and adverse events were the secondary outcome measures.
STATISTICS The data will be analyzed using SPSS version software for windows 7. For categorized parameters chi-square test will be used, Fisher exact test will be used for data less than 5 in each cell, while for numerical data t-test will be used to compare two groups. The level of significant used will be p<0.05.
Does the study require any investigation or intervention to be 7.3 conducted on patients or other humans or animals? if so please describe briefly Yes
This study will be conducted on the 60 patients undergoing surgery under
general anaesthesia with either PLMA or I–Gel under controlled
ventilation.
7.4 Has ethical clearance been obtained from your institution in case of 7.3 ?
Yes. Ethical clearance has been obtained from Institutional Ethical Committee of Rajarajeshwari Medical College, Bangalore. 8 List of References
1. Pelosi P, Foti G, Cereda M, Vicardi P, Gattinoni L. Effects of carbon dioxide insufflation for laparoscopic cholecystectomy on the respiratory system. Anaesthesia. 1996;51:744–9. 2. Levitan RM, Kinkle WC. Initial anatomic investigations of the I-gel airway: A novel supraglottic airway without inflatable cuff. Anaesthesia 2005; 60:1022-66. 3. Cunningham AJ, Brull SJ. Laparoscopic cholecyst-ectomy: anesthetic implications. AnesthAnalg. 1993;76:1120–33. 4. O'Malley C, Cunningham AJ. Physiologic changes during laparoscopy. AnesthesiolClin N Am. 2001;19(1):1–19. 5. Brain AIJ, Verghese C, Strube PJ. The LMA ‘ProSeal’-a laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. 6. I-gel user guide. 2007. http:/www.i-gel.com. -i-gel instruction manual. 7. Brimacombe J, Keller C. The ProSeal laryngeal mask airway: a randomized, crossover study with the standard laryngeal mask airway in paralysed, anesthetized patients. Anesthesiology. 2000;93:104–9.
8. Uppal V, Fletcher G, Kinsella J. Comparison of the i-gel with the cuffed tracheal tube during pressure-controlled ventilation. Br J Anaesth. 2009;102(2):264–8.
9. Piper SN, Triem JG, Rohm KD, Maleck WH, Schollhorn TA, Boldt J. ProSeal-laryngeal mask versus endotracheal intubation in patients undergoing gynaecologic laparoscopy. Anasthesiol Intensivmed Notfallmed Schmerzther. 2004;39:132–7
10. Dumont L, Mattys M, Mardirosoff C, et al. Changes in pulmonary mechanics during laparoscopic gastroplasty in the morbidly obese patient. ActaAnaesthesiol Scand. 1997;41:408–13
11. Bercker S, Schmidbauer W, Volk T, Bogusch G, Bubser HP, Hensel M, Kerner T. A Comparison of seal in seven supraglottic airway devices using a cadaver model of elevated esophageal pressure. AnesthAnalg. 2008;106:445–8. 9 Signature of Candidate
*Useful study. 10 Remarks of guide *Use of supraglottic airway in elective laparoscopic surgery is being investigated to know the hemodynamic stability and changes in respiratory mechanics.
11 11.1 Name and Dr.SAHAJANADA H designation of the MBBS, MD Guide PROFESSOR DEPARTMENT OF ANESTHESIOLOGY RAJARAJESHWARI MEDICAL COLLEGE, BANGALORE.
11.2 Signature
11.3 Co- guide (if any)
11.4 Signature
11.5 Head of the Dr.SAHAJANADA H Department MBBSMD PROFESSOR & HEAD DEPARTMENT OF ANESTHESIOLOGY RAJARJESHWARI MEDICAL COLLEGE, BANGALORE.
11.6 Signature
12 12.1 Remarks of the Chairman and Principal
12.2 Signature CERTIFICATE
The dissertation topic “ PLMA vs I-gel A COMPARATIVE STUDY OF
HEMODYNAMIC STABILITY AND RESPIRATORY MECHANICS IN
PATIENTS UNDERGOING LAPROSCOPIC SURGERIES: At Rajarajeshwari
Medical College and Hospital, Bangalore by Dr. HORMISE STEPHEN post- graduate student in the Department of Anesthesiology has been approved by the institutional ethical committee RAJARAJESWARI MEDICAL COLLEGE,
BANGALORE. INFORMED CONSENT I Dr.Hormise Stephen PG Department of anaesthesia conducting a randomized trial for award of MD degree in Anaesthesia. The topic of the study is: A comparative study of respiratory mechanics and hemodynamic stability in patients undergoing laparoscopic surgery: Proseal LMA versus the I-Gel
Objectives:
.
I have been briefed on the foregoing research being conducted by Dr. and it has been conveyed to me in my own language .I have had the opportunity to ask questions about it & all questions that I have asked have been answered to my satisfaction.I consent voluntarily to participate as a participant in this research & understand that I have the right to withdraw from the research at any time without in any way affecting my medical care. Name of the participant: ……………………………………………………………………………… Signature of the participant: ……………………………………………………………………………… Date:(d/m/y) ……………………………………………………………………………
If illiterate A literate witness must sign( If possible this person should be selected by the participant and should have no connection to the research team) I have read and witnessed the accurate reading of the consent form to the potential participant and the individual has had the opportunity to ask questions, I confirm that the individual has given consent freely.
Name of the witness...... Signature of witness:………………...... … Date:(d/m/y)……………...... Thumb impression of participant
I have read and witnessed the accurate reading of the consent form to the potential participant and the individual has had the opportunity to ask questions,I confirm that the individual has given consent freely. In case of any doubt I have been asked to contact :
Dr.Hormise Stephen PG.inANAESTHESIA
Name of Researcher:……………………………………………………… Signature of researcher:…………………………………………………… Date :( d/m/y)………………………………………………………………
. PROFORMA A comparative study of respiratory mechanics and hemodynamic stability in patients undergoing laparoscopic surgery: Proseal LMA versus the I-Gel
Group-P : LARYNGEAL MASK AIRWAY –PROSEAL Group-I : I-Gel
GENERAL CHARACTERSTIC ; Name :
Age/Gender :
IP. Number :
Ward/SU :
Date of surgery :
ASA Physical status :
Co morbidity :
Patient on any drugs :
Weight :
Height :
Body mass index :
Airway :
Mouth opening (cms.) :
Modified mallampatti grade :
Type of surgery :
Patient position during surgery :
Duration of surgery :
Monitors : SpO2
NIBP :
5 Lead ECG :
EtCO2:
Medications :Pre-medication : Inj. Metaclopramide 10 mg i.v 1 hr before induction Inj. Midazolam. 1.5 mg i.v just before induction InjGlycopyrolate 0.2 mg i.v just before induction OBSERVATIONS: Number of insertion attempt (tick any one): 1 2 3 failure
Duration of insertion attempt in seconds:
Efficacy of seal o Airway Leak pressure ( cm H2O)- Manometer method :
Gastric Insufflation: ( tick any one );
Yes No Intraoperative haemodynamics:
TIME Heart MAP EtCo2 SpO2 SBP DBP rate Baseline Post Induction 1Min.after insertion 5 Min. after insertion 10 Min. after insertion 15 Min. after insertion 20 Min. after insertion 25 Min. after insertion 30 Min. after insertion 45 Min. after insertion 1hr, after insertion 1hr.15 Min. after insertion 1hr 30 Min. after insertion 2hrs. after insertion After removal of device
MAP-Mean arterial pressur Spo2 - Oxygen saturationEtCo2 –End tidal CO2
Intraoperative respiratory mechanics: Time Compliance Peak Measured Commenst/Remarks airway minute pressure volume
Post operative device related complications (followed up for 24 hrs postoperatively)
Presence of blood in airway device Yes No
Post extubation cough Yes No
Laryngospasm Yes No
Sore throat Yes No
Dysphagia Yes No
Dysphonia Yes No
Nausea /Vomiting Yes No
Trauma to the lip/ teeth/pharynx Yes No
Arrhythmia Yes No
Odynaphagia Yes No
Ear pain / Blocked ears Yes No
Successful Gastric tube insertion Yes No
Numbness of tongue Yes No