South Hackney Recovery Team CMHT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

London Metropolitan Archives South Hackney
LONDON METROPOLITAN ARCHIVES Page 1 SOUTH HACKNEY SCHOOL ACC/3454 Reference Description Dates Cassland County Secondary School (formerly South Hackney Central School ) ACC/3454/001 Logbook for Lauriston Road Central School 1910 Aug Lauriston Road Central School -1913 Mar 1 volume ACC/3454/002 Logbook for South Hackney Central School;For 1913 Sep Logbook 1928-1937 see -1918 May LCC/EO/DN4/SOU/LB/1 South Hackney Central School 1 volume ACC/3454/003 Waiting List and Admission Register for South 1928 Apr-1944 Hackney Central School (some pages illegible Feb as ink has run) South Hackney Central School 1 volume ACC/3454/004 Waiting List and Admission Register for South 1942 Sep Hackney Central School -1948 Apr South Hackney Central School 1 volume ACC/3454/005 Admission Register South Hackney Central 1944 Aug School (from 1951 Cassland County Secondary -1958 Jun School) For Admission Register see LCC/EO/ DIV4/LAU/LB/1-6 South Hackney Central School 1 volume ACC/3454/006 Register of school leavers (entered in Register 1951 Jul-1960 of Children over Compulsory School Age) Apr Cassland County Secondary School 1 volume ACC/3454/007 Weekly attendance record with names of 1955 Sep school leavers -1956 Jul Cassland County Secondary School 1 volume ACC/3454/008/001 H.M.Inspector's reports on Cassland County 1952 Nov Secondary School & Lauriston County Secondary School LONDON METROPOLITAN ARCHIVES Page 2 SOUTH HACKNEY SCHOOL ACC/3454 Reference Description Dates ACC/3454/008/002 H.M.Inspector's reports on Cassland County 1952 Nov Secondary School & -

Asda Crossharbour District Centre
STRATEGIC DEVELOPMENT COMMITTEE 9th June 2021 Report of the Corporate Director of Place Classification: Unrestricted Application for Planning Permission Reference PA/19/02534 Site Asda – Crossharbour District Centre, 151 East Ferry Road, London, E14 3BT Ward Blackwall and Cubitt Town Proposal A hybrid planning application (part detailed, part outline) for the demolition of existing buildings and the comprehensive, mixed-use, re- development of the site, comprising a maximum of 218,991sqm (GEA) of floorspace. Full details are submitted for 526 residential units (Class C3), flexible commercial floorspace, including a new foodstore (17,087sqm GIA - A1-A4/B1), a primary school (D1), community uses (D1), public bus parking and a site wide basement, with associated uses as part of the development including car parking (up to 410 spaces), cycle parking, and an energy centre. Building heights would range between a maximum of 17.4m AOD (3 storeys above ground level) and 60m AOD (15 storeys above ground level). Creation of new vehicular and pedestrian access and public realm works, including all ground floor hard and soft landscaping and other works incidental to the proposals, including a programme of interim works (which include a temporary multi-storey car park with 349 car parking spaces and a temporary access lobby to the retail foodstore). Outline permission (with layout, scale, appearance and landscaping at upper levels being reserved) is sought for up to 111,137sqm GEA above podium level, comprising of between 1217 and 1446 residential units (C3), with associated private and communal podium amenity and landscaping, within four buildings with maximum heights ranging between up to 45.850m (AOD)/12 storeys and up to 115.50m (AOD)/32 storeys. -
Map Series of Walks Connecting Hackney's
The route passes some interesting architecture. MAP SERIES OF WALKS Haggerston Pool. Splendidly ornate building. Opened Gainsborough Studios (north of Shoreditch Park); City in 1904 and now abandoned. of London skyline including the Gherkin; St Leonard’s CONNECTING HACKNEY’S St Mary’s Garden. Run by Thrive, a charity which Hospital, Hoxton Street; LCC blocks (Tyssen Street); provides horticultural training. Open during the day: Geffrye Museum; old and new houses along Pearson PARKS & OPEN SPACES another wonderful haven in urban south Hackney, with Street; Fellows Court (1960s housing), Haggerston trees, shrubs, flowers and vegetables. Monthly open Pool; Whiston Estate (1950s design similar to days and often plants for sale. Bankside Power Station – now Tate Modern); Broadway Market (C19 buildings, and Gas Holders); Haggerston Park. Created in 1970s on land which Hothouse by railway bridge on Martello Street; was once the site of Gas Works, bombed in 1944. A Hackney Town Hall; Hackney Empire. Lots of cafés dock linked the works to the Regent’s Canal (opened and places to stop and enjoy wildlife and views. in 1820). The dock is now filled in and planted with silver birch. Fine wisteria curls round columns near Shoreditch Park. Area badly bombed in World War II. Whiston Road entrance. Trees in walled section Two sections separated by Bridport Street. Mostly include dawn redwood, red oak, Norway maple, managed as amenity grassland, also tennis courts, Midland thorn, hawthorn, yew, prunus, willow and children’s play area and a large Play Park. Round the cotoneaster, as well as shrubs and flowers. Across the perimeter are seats and trees (cherries, false acacia, grassed sports area is newly created gateway from whitebeam, tree of heaven, giant redwood) – home to Dove Row and Whiston Estate. -

Delivery Charge
DELIVERY CHARGE N1 Canonbury Kings Cross, Islington, Pentonville Hoxton £15.00 N2 East Finchley, Fortis Green, Hampstead Garden £15.00 N3 Finchley, Church End, Finchley Central £15.00 Finsbury Park, Manor House, Harringey (part) stroud £10.00 N4 green (part) N5 Highbury Highbury Fields £15.00 N6 Highgate, Hampstead Heath (part) £15.00 Holloway, Barnsbury (part) Islington (part), Tufnell £10.00 N7 park (part) N8 Hornsey, Crouch End, Harringey (part) £10.00 N9 Lower Edmonton, Edmonton (part) £10.00 N10 Muswell Hill £10.00 New Southgate, Friern Barnet, Bounds Green, Arnos £12.00 N11 Grove (part) N12 North Finchley, Woodside Park £15.00 N13 Palmers Green £10.00 N14 Southgate, Oakwood, Arnos Grove (part) £10-£15 South Tottenham, Harringey (part) West Green, Seven £6.00 N15 Sisters, Stamford Hill (part) Stoke Newington, Stamford Hill (part) Shacklewell, £6.00 N16 Dalston, Newington Green (part) N17 High Cross, Bruce Grove, Northumberland Park £6.00 N18 Upper Edmonton, Edmonton (part) £10.00 Upper Holloway, Archway, Tufnell Park (part) Hornsey £10.00 N19 (part) N20 Whetstone, Totteridge, Oakleigh Park £15.00 N21 Winchmore Hill, Bush Hill, Grange Park £12.00 N22 Wood Green, Bounds Green (part), Bowes Park £10.00 E1 Wapping £15.00 Bethnal Green, Haggerston Shoreditch, Cambridge £16.00 E2 Heath E3 Bow, Bromley-by-bow, Old Ford, Mile End, Three Mills £20.00 Chingford, Sewardstone, Highams Park, Upper £16.00 E4 Edmonton (part) E5 Upper Clapton, Lower Clapton, Stoke Newington (part) £12.00 E6 East Ham, Beckton, Upton Park, Barking £25.00 E7 Forest -
Annual Report 1929
THE LONDON COMMITTEE OF DEPUTIES OF THE BRITISH JEWS (FOUNDED IN 1760) GENERALLY KNOWN AS THE BOARD OF DEPUTIES OF BRITISH JEWS ANNUAL REPORT FOR 1929 3€ Q. 4Z 8 23 FINSBURY SQUARE LONDON, E.C.2 1930 UBftf^ 3 £ a. X? FORM OF BEQUEST. I bequeath to the LONDON COMMITTEE OF DEPUTIES OF THE BRITISH JEWS {generally known as the Board of Deputies of British Jews) the sum of £ free of duty, to be applied to the general purposes of the said Board and the receipt of the Treasurer for the time being of the said Board shall be a sufficient discharge for the same. CONTENTS. Alphabetical List of Deputies ... ... ... ... 5 List of Congregations and Institutes represented on the Board 18 Committees ... ... ... ... - ... ... 24 27 ... ... ... ד.. Annual Report—Introduction Law and Parliamentary Committee ••• ••• 29 Aliens Committee ••• *•• ••• 35 Shechita Committee ... ... .... ... 36 38 ••• ׳ ••• ••־ ••• Press Committee Education Committee ••• ••• ••• - •• • 39 40 ״. Foieign Appeals Committee Finance Committee ••• ••• ••• 40 ••• ... Palestine 40 Joint Foreign Committee ••• ••• ••• 44 Appendix A. — Memorandum on Civil Service Appointments ... ... ... ... ... 51 Appendix B.—Memorandum on Aliens Legislation ... 55 59 ••* ••• ••׳ ••• ••• ••• Accounts Secretaries for Marriage ••• ••> ••• ••• 64 Secretary : J. M. RICH, M.A., LL.B. 23 Finsbury Sq., E.C-2 Telephone : Clerkenwell 1187 and 8642 ' י.Telegraphic Address : " Lemonds London Solicitor: CHARLES H. L. EMANUEL, M.A. 5 THE BOARD OF DEPUTIES OF BRITISH JEWS. ALPHABETICAL LIST OF DEPUTIES. Revised to August 14th, 1930. Showing attendances during 1929. No. of meetings held, 10, (The date of.a Deputy's first election to the Board is not necessarily the date of his election for the Constituency he now represents.) First Elected No. -

Supplement to the London Gazette, February 25, 1871
SUPPLEMENT TO THE LONDON GAZETTE, FEBRUARY 25, 1871. NAME. RESIDENCE. OCCUPATION. Foster, William Burdett 76, East India-road, Poplar, E. Gentleman Fax-bridge, John 19, Bedford-place, Commercial-road, E. Oilman Gadsdon, Benj. 40, Union-street, Bishopsgate Ironmonger Gadsdon, Charles 40, Union-street, Bishopsgate Ironmonger Grant, James 41, Guildford-street, Russell-square Gentleman Gould, John 33, Chicksand-street, Whitechapel Manufacturing Chemist Gates, George Chesham House, Clifton-road, Brighton Gentleman Gainer, Joseph Stonehouse, Gloucestershire Gentleman Galloway, R. The Gresham Club, City, E.G. Gentleman Grey, Lieut. H. R. E. Care of Messrs. Tory, Hildreth, and Lieutenant R.N, Ommanney, 41, Norfork-street, Strand Gross, Charles Bexley-road, Erith, S.E. Gentleman Goodwin, Benjamin Belgrave-terrace Oakfield-road, Hackney Gentleman Grillon, Gustave 5, Stafford-place, Pimlico Gentleman Gatenby, Robt. 66, Christian-street, St. George's, E. Coffee Roaster Giles, Richard M., deceased 2, Woodgrange-villas, Forest Gate, E. (James Marsh and John Wilson, executors) Gillum, Stephen F., and f Gentleman Mary Ann, his wife Layfield House, Sudbury Goode, John Richard, sen. Woodford, Essex Gentleman Hall, Benjamin, Jun. 54, Bromley-street, Commercial-road E. Gentleman Hunter, Edward The Glebe, Blackheath Gentleman Hubbard, John (deceased), 171, High-street, Shadwell Mary Hubbard and another Executors Hedgman, James Elm Bank, Barnes, Surrey Gentleman Hadow, Patrick D. 122, Leadenhall-street, London, E.C. Gentleman Holmes, Ann 32, Groom-bridge-road, South Hackney Spinster Hopper, Thos. Duck 25, Eastcheap, E.C. Merchant Hammack, Henry Lawrence 59, Bishopsgate-street, E.C. Architect Hall, Benjamin 54, Bromley-street, Commercial-road E. Gentleman Haigh, John 293, Mile End-road, E Haberdasher Hart, Amy Ayton House, Seven Sisters'-road, Stoke Spinster Newington Holding, George 31, Great St. -

Hackney Transport Strategy 2014-2024
Hackney Transport Strategy 2014-2024 Walking Plan Summer 2014 PJ55910 Hackney Transport Strategy 2014‐2024 Walking Plan Contents 1. Introduction Page 3 2. Daughter Documents Page 6 3. Why the need for a Walking Plan? Page 7 4. Policy Frameworks Page 10 5. Walking in Hackney – current trends and targets Page 11 6. Challenges and barriers to walking more in Hackney Page 17 7. Proposed Actions, Policies and Proposals Page 22 8. Action Plan for Walking Page 30 9. Delivery Plan – Funding and Priorities Page 48 10. Monitoring Page 55 11. Bibliography Page 56 Tables Table 1: Hacking Walking to Work comparison table Page 13 Table 2: Travel to school mode share in Hackney Page 15 Table 3: Barriers to walking Page 17 Table 4: Consultation Issues Raised Page 19 Table 5: Impacts of Workplace Travel Plans Page 46 Table 6: Public Realm Major Schemes Page 50 Table 7: Local Improvement Schemes Page 52 Table 8: Smarter Travel/ Encouragment Measures Page 54 Figures Figure 1: Census 2001 walking to work levels in Hackney Page 14 Figure 2: Hackney Central APP proposed public realm interventions Page 33 Figure 3: Hackney Wick AAP proposed public realm & open space improvements Page 36 Figure 4: Legible london ‐ Existing & proposed short term extension of LL signage Page 34 2 Hackney Transport Strategy 2014‐2024 Walking Plan 1. Introduction Walking remains the most basic and commonly used form of transportation. The vast majority of all journeys start with and end with a walk regardless of the modes used in between. This Walking Plan outlines Hackney Council’s commitment towards walking and sets out a set of policies and proposals for the period 2014 to 2024 to make walking a normal, safe and attractive choice for travel and recreation for our residents and those that work, visit and pass through the borough. -
Stories of a Hackney Generation
Diversity Stories of a Hackney Generation CONNECT HACKNEY ageing better Clockwise from top left: Newton Dunbar, Patricia Charlesworth, Centre 151, Harold Rubin, Anita Jacques, Clair Battaglino I hope by sharing these stories, people “living and working in Hackney are inspired to continue to celebrate the diversity the borough holds...” Introduction Connect Hackney works to tackle loneliness and isolation amongst people aged 50 and over. The issue of loneliness and isolation is multifaceted, and personal to each person who experiences it. One way we are tackling the issue is by providing more opportunities for older people to play an active role within their community, showcasing the valuable contributions they make. Hackney is a melting pot of people from a diverse mix of backgrounds, each with their own story of how Hackney became their home. What I’ve personally enjoyed about the Diversity Project is the unearthing of these stories and hearing how Hackney has changed. But within that, also seeing how much Hackney people celebrate the diversity of the borough, with people from different races, cultures, religions and sexual identities living side-by-side. These stories, similar to the ones we shared in our Windrush publication last year, provide an opportunity for these stories to be heard, both now and for generations to come. The more we understand about each other, the more opportunities we create for people to make new social connections, be valued and respected, and lead more fulfilling lives. I hope by sharing these stories, people living and working in Hackney are inspired to continue to celebrate the diversity the borough holds, particularly amongst its older residents; ensuring that no matter where you come from, your religious beliefs, who you love, or your age, you feel welcomed, valued and respected for the person you are. -

Telling the Truth Through False Teeth by Rossana Tich
At the Heart of Hackney since 1967 2012 THE HACKNEY SOCIETY SPACENews and views about Hackney’s builtS environment Issue 37 Summer 2012 // ISSN 2047-7457 Telling the Truth through False Teeth By Rossana Tich Over the past few months, a mid- Alex Chinneck believes, ‘These factories 20th-century factory, earmarked may be industrially redundant, but I think it for demolition, on Tudor Road, E9 is important to preserve them and recognise the architectural contribution they make has slowly and painstakingly been installation period I have heard many different to London’s eclectic skyline and streets. It transformed into a work of art by Alex interpretations of what the work means and seems odd that we tear down structures that Chinneck in association with Sumarria why I have done it. Everyone is welcome to have been built to last.’ Lunn Gallery. People passing by have interpret the intervention in their own way; I been doing a double take, realising In total 312 panes from 13 windows have just hope they enjoy it.’ been replaced with 1,248 pieces of glass – that the original broken windows had Telling the Truth Through False Teeth four pieces form the perfect break in every been replaced with … broken windows, Artist: Alex Chinneck (http://www. pane. The familiar is made unfamiliar by the albeit 312 identically smashed panes. alexchinneck.com/) in association with repetition and exactness of the work – the Sumarria Lunn Gallery. Location: corner The site was once a shoe factory and most combination of engineering and accident of Mare Street and Tudor Road, Hackney, recently a cannabis factory! Chinneck spent a completes the illusion. -
London Borough of Hackney Third Local Implementation Plan (2019
London Borough of Hackney Third Local Implementation Plan (2019-2022) March 2019 Contents List of Figures and Tables 4 Foreword 5 Executive summary 6 1. Introduction and preparing a LIP 9 Introduction 9 Local approval process 9 Statutory consultation 9 Statutory duties 10 LIP approval 10 2. Borough Transport Objectives 11 Introduction 11 Local context 11 Changing the transport mix 20 Outcome 1: London’s streets will be healthy and more Londoners will travel actively 28 Outcome 2: London’s streets will be safe and secure 41 Outcome 3: London’s streets will be used more efficiently and have less traffic on them 52 Outcome 4: London’s streets will be clean and green 61 Outcome 5: The public transport network will meet the needs of a growing London 69 Outcome 6: Public transport will be safe, affordable and accessible to all 73 Outcome 7: Journeys by public transport will be pleasant, fast and reliable 78 Outcome 8: Active, efficient and sustainable travel will be the best option in new developments 81 Outcome 9: Transport investment will unlock the delivery of new homes and jobs 84 Other Mayoral Strategies 90 3. The Delivery Plan 93 Introduction 93 TfL Business Plan 93 Sources of funding 95 Long-Term interventions to 2041 97 Hackney LIP delivery programme (2019-2022) 101 Risks to the delivery of the three-year programme 107 Monitoring the delivery of the outcomes of the Mayor’s Transport Strategy 112 MTS and borough outcome indicator targets 113 Appendix A Hackney Local Implementation Plan Objectives and Targets 123 Appendix B Hackney Transport -
Executive Summary Summer 2014
Hackney Transport Strategy 2014-2024 Executive Summary Summer 2014 PJ56327 Hackney Transport Strategy 2014-2024 – Executive Summary Executive Summary 1. Introduction 1.1 This is the Hackney’s Transport Strategy 2014‐2024. The Strategy sets out Hackney’s strategic transportation aims, objectives and priorities for 2014‐2024. The Strategy aims to support other Strategies including the Sustainable Community Strategy and the emerging Local Development Framework. 1.2 The vision for Hackney’s Transport Strategy is: “By 2024, Hackney’s transport system will be an exemplar for sustainable urban living in London. It will be fair, equitable, safe and responsive to the needs of its residents and businesses, facilitating the highest quality of life standards for a borough in the Capital and leading London in its approach to tackling its urban transport challenges of the 21st Century.” 1.3 By 2024, this Hackney’s Transport Strategy will have achieved the following goals: I. Hackney is renowned for having the most pedestrian and cyclist friendly neighbourhoods, streets and public realm in London. II. Hackney remains one of London’s most liveable boroughs with green, safe and thriving neighbourhoods, streets and public spaces where different communities get on and interact. III. To have played an important role in improved resident’s health and well being, as well as tackling obesity levels through higher rates of active travel. IV. To have substantially reduced road danger for all our residents but particularly more vulnerable groups such as older people and children and especially vulnerable road users such as cyclists, pedestrians and motorcyclists. V. To have continued the reduction in car ownership and created an environment where owning a private car is not the norm. -
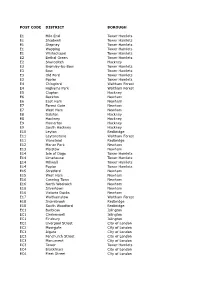
POST CODE DISTRICT BOROUGH E1 Mile End Tower Hamlets E1
POST CODE DISTRICT BOROUGH E1 Mile End Tower Hamlets E1 Shadwell Tower Hamlets E1 Stepney Tower Hamlets E1 Wapping Tower Hamlets E1 Whitechapel Tower Hamlets E2 Bethal Green Tower Hamlets E2 Shoreditch Hackney E3 Bromley-by-Bow Tower Hamlets E3 Bow Tower Hamlets E3 Old Ford Tower Hamlets E3 Poplar Tower Hamlets E4 Chingford Waltham Forest E4 Highams Park Waltham Forest E5 Clapton Hackney E6 Beckton Newham E6 East Ham Newham E7 Forest Gate Newham E7 West Ham Newham E8 Dalston Hackney E8 Hackney Hackney E9 Homerton Hackney E9 South Hackney Hackney E10 Leyton Redbridge E11 Leytonstone Waltham Forest E11 Wanstead Redbridge E12 Manor Park Newham E13 Plaistow Newham E14 Isle of Dogs Tower Hamlets E14 Limehouse Tower Hamlets E14 Millwall Tower Hamlets E14 Poplar Tower Hamlets E15 Stratford Newham E15 West Ham Newham E16 Canning Town Newham E16 North Woolwich Newham E16 Silvertown Newham E16 Victoria Docks Newham E17 Walthamstow Waltham Forest E18 Snarebrook Redbridge E18 South Woodford Redbridge EC1 Barbican Islington EC1 Clerkenwell Islington EC1 Finsbury Islington EC2 Liverpool Street City of London EC2 Moorgate City of London EC3 Algate City of London EC3 Fenchurch Street City of London EC3 Monument City of London EC3 Tower Tower Hamlets EC4 Blackfriars City of London EC4 Fleet Street City of London EC4 St Paul's City of London EC4 Temple City of London N1 Barnsbury Islington N1 Canonbury Islington N1 Hoxton Hackney N1 Islington Islington N1 Shoreditch Hackney N2 East Finchley Barnet N2 Finchley Barnet N2 Hampstead Gdn Suburb (East) Barnet