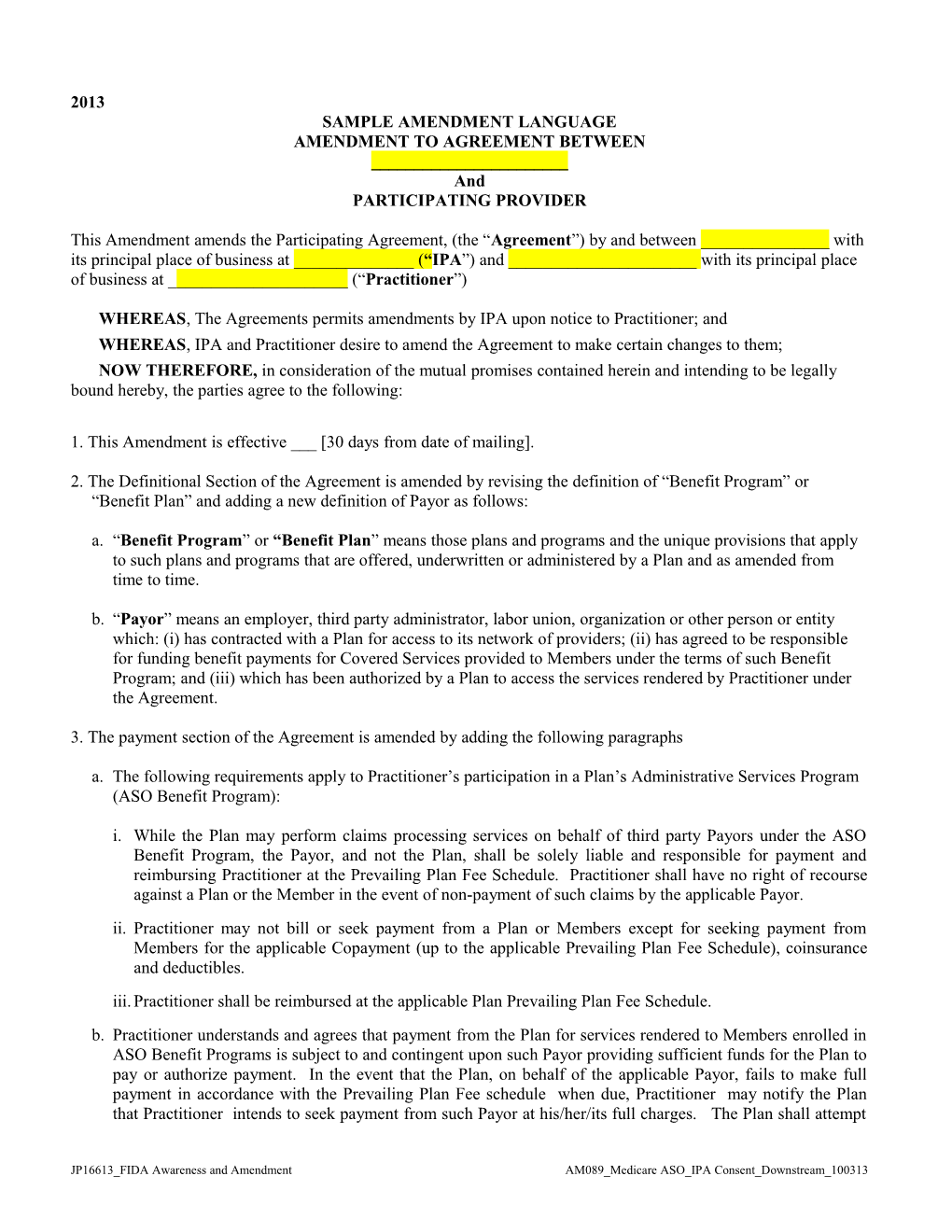
2013 SAMPLE AMENDMENT LANGUAGE AMENDMENT TO AGREEMENT BETWEEN ______And PARTICIPATING PROVIDER
This Amendment amends the Participating Agreement, (the “Agreement”) by and between ______with its principal place of business at ______(“IPA”) and ______with its principal place of business at ______(“Practitioner”)
WHEREAS, The Agreements permits amendments by IPA upon notice to Practitioner; and WHEREAS, IPA and Practitioner desire to amend the Agreement to make certain changes to them; NOW THEREFORE, in consideration of the mutual promises contained herein and intending to be legally bound hereby, the parties agree to the following:
1. This Amendment is effective ___ [30 days from date of mailing].
2. The Definitional Section of the Agreement is amended by revising the definition of “Benefit Program” or “Benefit Plan” and adding a new definition of Payor as follows:
a. “Benefit Program” or “Benefit Plan” means those plans and programs and the unique provisions that apply to such plans and programs that are offered, underwritten or administered by a Plan and as amended from time to time.
b. “Payor” means an employer, third party administrator, labor union, organization or other person or entity which: (i) has contracted with a Plan for access to its network of providers; (ii) has agreed to be responsible for funding benefit payments for Covered Services provided to Members under the terms of such Benefit Program; and (iii) which has been authorized by a Plan to access the services rendered by Practitioner under the Agreement.
3. The payment section of the Agreement is amended by adding the following paragraphs
a. The following requirements apply to Practitioner’s participation in a Plan’s Administrative Services Program (ASO Benefit Program):
i. While the Plan may perform claims processing services on behalf of third party Payors under the ASO Benefit Program, the Payor, and not the Plan, shall be solely liable and responsible for payment and reimbursing Practitioner at the Prevailing Plan Fee Schedule. Practitioner shall have no right of recourse against a Plan or the Member in the event of non-payment of such claims by the applicable Payor. ii. Practitioner may not bill or seek payment from a Plan or Members except for seeking payment from Members for the applicable Copayment (up to the applicable Prevailing Plan Fee Schedule), coinsurance and deductibles. iii. Practitioner shall be reimbursed at the applicable Plan Prevailing Plan Fee Schedule. b. Practitioner understands and agrees that payment from the Plan for services rendered to Members enrolled in ASO Benefit Programs is subject to and contingent upon such Payor providing sufficient funds for the Plan to pay or authorize payment. In the event that the Plan, on behalf of the applicable Payor, fails to make full payment in accordance with the Prevailing Plan Fee schedule when due, Practitioner may notify the Plan that Practitioner intends to seek payment from such Payor at his/her/its full charges. The Plan shall attempt
JP16613_FIDA Awareness and Amendment AM089_Medicare ASO_IPA Consent_Downstream_100313 to resolve the payment dispute by contacting the Payor and using commercially reasonable efforts to get the claim paid. Practitioner may seek payment directly from the Payor only if: (i) Practitioner first inquires in writing to the Plan as to whether the Payor has defaulted; (ii) the Plan confirms in writing that Payor has defaulted, and (iii) Practitioner provides the Plan an additional fifteen (15) days prior written notice of its intention to seek payment from Payor. For purposes of this paragraph, Practitioner may seek payment from a Payor only if the failure to pay a claim is due to: (i) a systematic failure by a Payor to fund clean/nondisputed claims payments related to Members covered through that Payor; or (ii) a single failure by a Payor to fund payment for more than sixty (60) days after the receipt of Practitioner’s clean claim. A default in payment does not occur in the case of a dispute as to whether certain claims should be paid or the amounts that should be paid for certain claims related to the application of the terms of this Agreement and/or cases where the dispute resolution process as defined in this Agreement is being followed. 4. The Medicaid Addendum is hereby modified to include the following wording:
The following provision applies to health care services rendered by Practitioner to: (i) Medicaid Managed Care, (ii) Family Health Plus (FHPlus) and (iii) Managed Long Term Care (MLTC) members covered under a Benefit Plan pursuant to the Plan’s contracts with the New York State Department of Health.
a. Practitioners who wish to let their patients know of their affiliations with one or more Managed Care Organizations (MCOs) must list each MCO with whom they have contracts.
b. Practitioners who wish to communicate with their patients about managed care options must advise patients, taking into consideration ONLY the managed care options that best meet the health needs of the patients. Such advice, whether presented verbally or in writing, must be individually based and not merely a promotion of one MCO over another.
c. Practitioners may display a Plan’s outreach materials provided that appropriate material is conspicuously posted for all other MCOs with whom the Practitioner has a contract.
d. Upon termination of a Provider Agreement with a Plan, Provider who has contracts with other MCOs that offer Medicaid, FHPlus or MLTC products may notify their patients of the change in status and the impact of such change on the patient.
6. The Medicare paragraph set forth in the Miscellaneous Section of the Agreement is revised in its entirety as follows:
Medicare Advantage and Medicare-Medicaid Dual Eligible Members. For services rendered to a Plan’s Medicare Advantage Members and Medicare-Medicaid Dual Eligible Members in accordance with the Agreement, the provisions in the “Medicare Advantage/Medicare–Medicaid Dual Eligible Addendum” set forth below, which are incorporated herein by reference as if fully set forth in the Agreement, shall be binding on the parties hereto. With respect to such Medicare Advantage/Medicare-Medicaid Dual Eligible Members, these provisions shall prevail over any provision in the Agreement that may conflict or appear inconsistent with any provision in the Addendum.
7. The Medicare Addendum attached to the Agreement is revised in its entirety with the provisions set forth below:
JP16613_FIDA Awareness and Amendment AM089_Medicare ASO_IPA Consent_Downstream_100313 MEDICARE ADVANTAGE MEDICARE/MEDICAID DUAL ELIGIBLE
ADDENDUM
Medicare Advantage/Medicare-Medicaid Required Provisions
Plan has a contract with CMS for the provision of services to Medicare Enrollees. Accordingly, Practitioner agrees to provide all services under the Agreement in compliance with the following provisions.
Definitions:
Centers for Medicare and Medicaid Services (“CMS”): the agency within the Department of Health and Human Services that administers the Medicare program.
Completion of Audit: completion of audit by the Department of Health and Human Services, the Government Accountability Office, or their designees of a Medicare Advantage Organization, Medicare Advantage Organization contractor or related entity.
Downstream Entity: any party that enters into a written arrangement, acceptable to CMS, with persons or entities involved with the MA benefit, below the level of the arrangement between an MA organization (and applicant) and a first tier entity. These written arrangements continue down to the level of the ultimate provider of both health and administrative services.
Final Contract Period: the final term of the contract between CMS and the Medicare Advantage Organization.
First Tier Entity: any party that enters into a written arrangement, acceptable to CMS, with an MA organization or applicant to provide administrative services or health care services for a Medicare eligible individual under the MA program.
Medicare Advantage (“MA”): an alternative to the traditional Medicare program in which private plans run by health insurance companies provide health care benefits that eligible beneficiaries would otherwise receive directly from the Medicare program.
Medicare Advantage Organization (“MA organization”): a public or private entity organized and licensed by a State as a risk-bearing entity (with the exception of provider-sponsored organizations receiving waivers) that is certified by CMS as meeting the MA contract requirements.
Member or Enrollee: a Medicare Advantage eligible individual who has enrolled in or elected coverage through a Medicare Advantage Organization.
Provider: (1) any individual who is engaged in the delivery of health care services in a State and is licensed or certified by the State to engage in that activity in the State; and (2) any entity that is engaged in the delivery of health care services in a State and is licensed or certified to deliver those services if such licensing or certification is required by State law or regulation.
Related entity: any entity that is related to the MA organization by common ownership or control and (1) performs some of the MA organization's management functions under contract or delegation; (2) furnishes services to Medicare enrollees under an oral or written agreement; or (3) leases real property or sells materials to the MA organization at a cost of more than $2,500 during a contract period.
JP16613_FIDA Awareness and Amendment AM089_Medicare ASO_IPA Consent_Downstream_100313 Required Provisions:
Practitioner agrees to the following:
1. HHS, the Comptroller General, or their designees have the right to audit, evaluate, and inspect any pertinent information for any particular contract period, including, but not limited to, any books, contracts, computer or other electronic systems (including medical records and documentation of the first tier, downstream, and entities related to CMS’ contract with a Plan (hereinafter, “MA organization”) through 10 years from the final date of the final contract period of the contract entered into between CMS and the MA organization or from the date of completion of any audit, whichever is later. [42 C.F.R. §§ 422.504(i)(2)(i) and (ii)]
2. Practitioner will comply with the confidentiality and enrollee record accuracy requirements, including: (1) abiding by all Federal and State laws regarding confidentiality and disclosure of medical records, or other health and enrollment information, (2) ensuring that medical information is released only in accordance with applicable Federal or State law, or pursuant to court orders or subpoenas, (3) maintaining the records and information in an accurate and timely manner, and (4) ensuring timely access by enrollees to the records and information that pertain to them. [42 C.F.R. §§ 422.504(a)(13) and 422.118]
3. Enrollees will not be held liable for payment of any fees that are the legal obligation of the MA organization. [42 C.F.R. §§ 422.504(i)(3)(i) and 422.504(g)(1)(i)]
4. For all enrollees eligible for both Medicare and Medicaid, enrollees will not be held liable for Medicare Part A and B cost sharing when the State is responsible for paying such amounts. Practitioners will be informed of Medicare and Medicaid benefits and rules for enrollees eligible for Medicare and Medicaid. Practitioner may not impose cost-sharing that exceeds the amount of cost-sharing that would be permitted with respect to the individual under title XIX if the individual were not enrolled in such a plan. Practitioner will: (1) accept the MA plan payment as payment in full, or (2) bill the appropriate State source. [42 C.F.R. §§ 422.504(i)(3)(i) and 422.504(g)(1)(i)]
5. Any services or other activity performed in accordance with a contract or written agreement by Practitioner are consistent and comply with the MA organization's contractual obligations. [42 C.F.R. § 422.504(i)(3)(iii)]
6. Contracts or other written agreements between the MA organization and providers or between first tier and downstream entities must contain a prompt payment provision, the terms of which are developed and agreed to by the contracting parties. The MA organization is obligated to pay contracted providers under the terms of the contract between Practitioner and the provider. [42 C.F.R. §§ 422.520(b)(1) and (2)]
7. Practitioner and any related entity, contractor or subcontractor will comply with all applicable Medicare laws, regulations, and CMS instructions. [42 C.F.R. §§ 422.504(i)(4)(v)]
8. If any of the MA organization’s activities or responsibilities under its contract with CMS are delegated to any first tier, downstream and related entity:
i. The delegated activities and reporting responsibilities are specified in writing.
ii. CMS and the MA organization reserve the right to revoke the delegation activities and reporting requirements or to specify other remedies in instances where CMS or the MA organization determine that such parties have not performed satisfactorily.
iii. The MA organization will monitor the performance of the parties on an ongoing basis.
JP16613_FIDA Awareness and Amendment AM089_Medicare ASO_IPA Consent_Downstream_100313 iv. The credentials of medical professionals affiliated with the party or parties will be either reviewed by the MA organization or the credentialing process will be reviewed and approved by the MA organization and the MA organization must audit the credentialing process on an ongoing basis.
v. If the MA organization delegates the selection of providers, contractors, or subcontractor, the MA organization retains the right to approve, suspend, or terminate any such arrangement. [42 C.F.R. §§ 422.504(i) (4) and (5)].
In the event of a conflict between the terms and conditions above and the terms of a related agreement, the terms above control.
Medicare-Medicaid Program Required Provisions
Plan has a contract with CMS for the provision of services under the Medicare-Medicaid (“MMP”) Program. Accordingly, Practitioner agrees to provide all services under the Agreement in compliance with the following provisions.
1. HHS, the Comptroller General or their designees have the right to audit, evaluate and inspect any pertinent information of Practitioner Providers including books, contracts, records, including medical records, and documentation related to CMS’ contract with the Plan for a period of 10 years from the final date of the contract period or the completion of any audit, whichever is later. §422.504(i) (2) (i) and (ii)
2. Where applicable, Practitioner, suppliers and providers agree to safeguard beneficiary privacy and confidentiality of beneficiary health records. §422.504(a) 13
3. Where applicable, Practitioner may not hold beneficiaries liable for payment of fees that are the legal obligation of a Plan §422.504(g) (1) (i); §422.504(i) (3) (i).
4. Any services performed will be consistent and comply with Plan’s contractual obligations with CMS and New York State Department of Health. §422.504(i) (3) (iii).
5. Plan retains the right to approve, suspend, or terminate such arrangement. §422.504(i) (5).
6. All delegated activities and reporting responsibilities of Practitioner are clearly defined in this Agreement. §422.504(i) (4) (i).
7. The Plan may revoke any of the delegated activities and reporting requirements or specify other remedies in instances when CMS or the New York State Department of Health determines that the parties to this Agreement have not performed satisfactorily. §422.504(i) (3) (ii); §422.504(i) (4) (ii).
8. Performance of the parties is monitored by the Plan on an ongoing basis. §422.504(i) (3) (ii); §422.504(i) (4) (iii).
9. The credentials of medical professionals affiliated with the parties will either be reviewed by the Plan or the credentialing process will be reviewed and approved by the Plan; and the Plan must audit the credentialing process on an ongoing basis. §422.504(i) (4) (IV) (A) (B).
10. Practitioners must comply with all applicable Medicare laws, regulations, and CMS instructions. §422.504(i)(4) (v).
11. This Agreement incorporates the Medicare-Medicaid population.
JP16613_FIDA Awareness and Amendment AM089_Medicare ASO_IPA Consent_Downstream_100313 12. Practitioner will complete required FIDA training outlined in the New York State Memorandum of Understanding or certify to the Plan that training has been completed through another health plan or organization approved by CMS to provide such training. Training will include:
i. No balance billing of FIDA participants. ii. Cultural and linguistic competency for delivering services to FIDA participants. iii. Physical accessibility, which is defined in accordance with U.S. Department of Justice ADA guidance for providers. iv. Disability competency for delivering services to FIDA participants.
Required training for Interdisciplinary Care Team Members (IDT) only:
i. Person-centered planning process ii. Independent living and recovery iii. Wellness principles iv. Olmstead requirements v. Coordinating with behavioral health and community-based and facility-based long-term services and supports (LTSS) providers, providing information about accessing behavioral health and community-based and facility-based LTSS, and furnishing lists of community supports available. vi. How to identify behavioral health needs, how to assist the Participant in obtaining behavioral health services, how to identify community-based and facility-based LTSS needs, and how to assist the Participant in obtaining community-based and facility-based LTSS services (required only for primary care providers)
13. Practitioner agrees to use evidence-based practices specific to his/her/their area of practice.
AM089