RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA
SYNOPSIS
FOR REGISTRATION OF SUBJECT FOR DISSERTATION
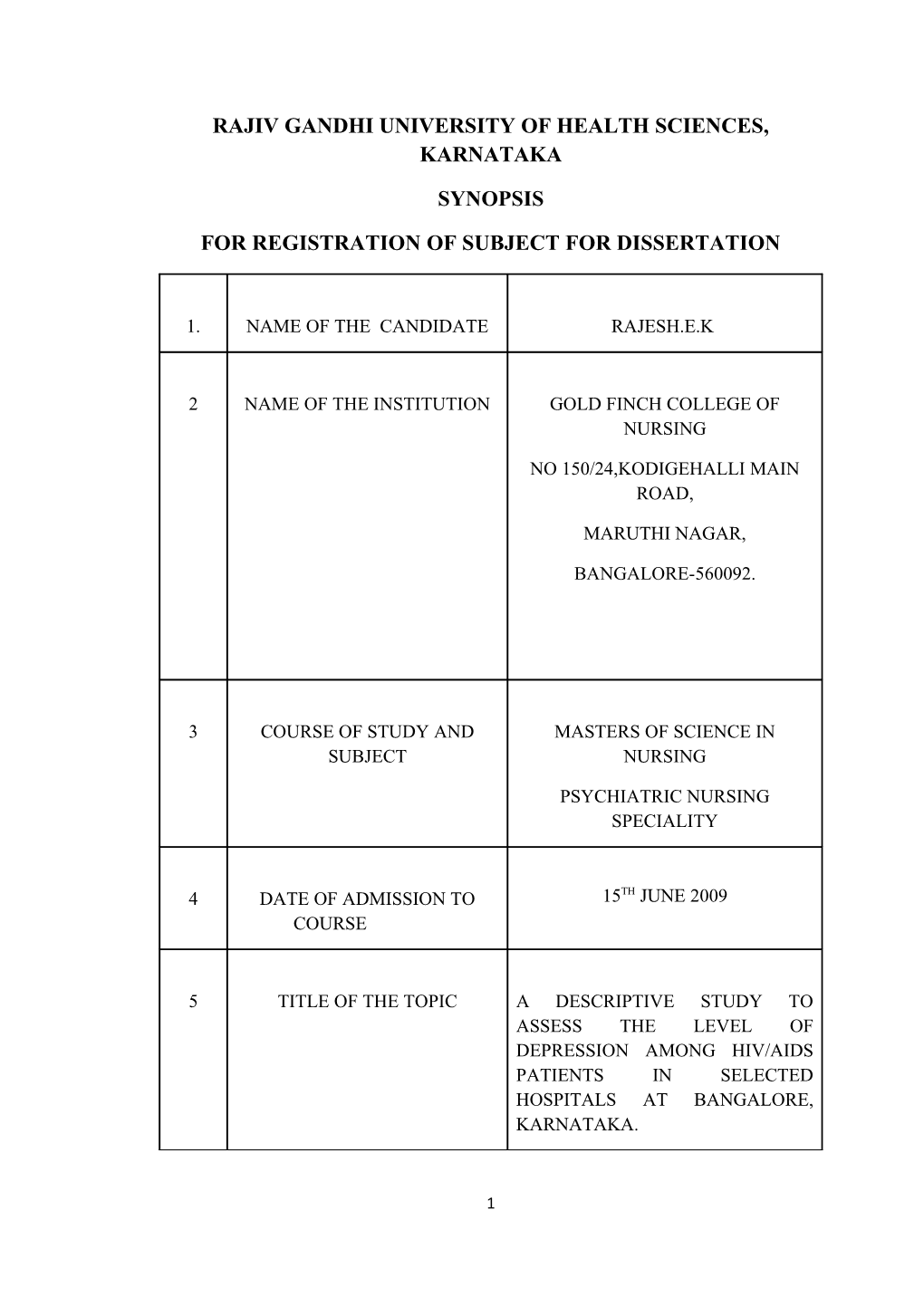
1. NAME OF THE CANDIDATE RAJESH.E.K
2 NAME OF THE INSTITUTION GOLD FINCH COLLEGE OF NURSING
NO 150/24,KODIGEHALLI MAIN ROAD,
MARUTHI NAGAR,
BANGALORE-560092.
3 COURSE OF STUDY AND MASTERS OF SCIENCE IN SUBJECT NURSING
PSYCHIATRIC NURSING SPECIALITY
4 DATE OF ADMISSION TO 15TH JUNE 2009 COURSE
5 TITLE OF THE TOPIC A DESCRIPTIVE STUDY TO ASSESS THE LEVEL OF DEPRESSION AMONG HIV/AIDS PATIENTS IN SELECTED HOSPITALS AT BANGALORE, KARNATAKA.
1 6. BRIEF RESUME OF INTENDED WORK
INTRODUCTION
"Things will happen in your life that you can’t stop, but that is no reason to shut out the world. There is a purpose for the good and for the bad ".
Acquired Immunodeficiency Syndrome (AIDS) was formally recognized in the United States in 1981. AIDS is believed to have originated in Africa but now it is a global health crisis, affecting nearly 36.8 million persons worldwide.
According to worldwide HIV/AIDS statistics(2008) , people living with HIV/AIDS in
Sub-Saharan Africa is 22 to 24 million ,North Africa and Middle East are 380000 ,
Asia is 5 million , Oceania is 74000, Latin America is 1.7 million , in Caribbean
230000 , Eastern Europe and Central Asia 1.5 million , and North America, western and Central Europe are 2.2 million . Approximately 21.8 million people have died from this disease, and nearly 14000 new cases are diagnosed daily. Though an estimated 70% of all infections occur in Sub-Saharan Africa, the United States has been 1 and 1.2 million citizen living with this disease.
According to the American Foundation for AIDS Research, AIDS deaths in the US reached an all times high in 1995. In 2005, the surveillance report showed that the greatest number of persons in US living with HIV/AIDS and depression are located in New York, Florida and Texas, with approximately 11% of total AIDS patients residing in The Lone Star States. Centres for Disease Control and prevention
(CDC) collected data from 33 states comprising approximately 63% of the epidemic in the US. The CDC has published an analysis of data from 2001 – 2005 to provide an overview of the trends and current status of HIV/AIDS in this population.29
2 Jin et al reported that 79% of HIV patients reported lifetime depression compared to only 4% of normal controls in a sample of Chinese people. In the US, the lifetime risk of developing clinical depression in someone without HIV reportedly ranges from 4.9 to 17.9%, where the risk on HIV patients has been reported to be anywhere from 20 to 37%. This and other reports, suggest that the prevalence rate of
Major Depressive Disorder (MDD) is a staggering 2 to5 times greater in HIV/AIDS patients than in the general population.
Globally, India is the second only to South Africa in terms of number of people living with the disease. As per National AIDS Control Organization, there are
5.1 million people across India suffering with HIV positive. Around 38% of these people are women. By the end of May 2008, the total number of AIDS cases reported in India was 109400 of whom 31994 were women. The UN Population Division
Project that India’s adult HIV prevalence will be peak at 1.9% in 2010.2
Karnataka is one of the six HIV/ AIDS high prevalence states in India, with over one half million adults infected with the virus. Karnataka has a population of 53 million and is a diverse state. In Karnataka 10lakhs pregnancies are estimated per year. Of these, 26000 pregnancies are expected to be HIV positive, out of which 30% vertical transmission from mother to child may result in 7800 children being born with HIV infection. AIDS prevention and control measures were initiated in the state in 1987 under the technical guidance of Indian Council of Medical Research and an
AIDS surveillance centre was established in the Department of Microbiology,
Victoria Hospital and Bangalore Medical College.1
The number of HIV/AIDS patients with depression in India is difficult to determine. Studies of the National AIDS Control Organization reported that 80% of 3 HIV positive patients suffering with lifetime depression. The lifetime risk of developing clinical depression in someone without HIV reportedly ranges from 5-
10%, where risk in HIV patients has been reported to be anywhere from 25-50%. This and other reports, suggest that the prevalence rate of Major Depressive Disorder
(MDD) is a staggering 2 to 5 times greater in HIV /AIDS patients than in the general population.2
In addition, AIDS patients often reported decreased quality of life during routine medical visits, which in some case has lead to suicidal thought and / or attempts. In one study of 149 HIV positive patients, almost half had attempted suicide, which is an alarming high rate. However, more counseling services and increased public awareness of the disease with a decrease in stigma, helps to decrease in the prevalence of depression and suicidal ideation.
6.1 NEED FOR THE STUDY
HIV/AIDS is a burning problem faced by the world today. HIV/AIDS has many physical effects, but perhaps some of its most profound effects are in the psychological, social and economic health of the HIV positive person, his or her loved ones, and the community. AIDS is the final and fatal stage of HIV infection.38.6 million people throughout the world have been infected with HIV/AIDS and almost
22 million people have died due to this dreaded disease so far.
Depression in the HIV/AIDS population is a global phenomenon. Jin et al (2008) reported that 79% of HIV patients reported lifetime depression compared to only 4%of normal controls in a sample of Chinese people. In the US, the lifetime risk of developing clinical depression in someone without HIV reportedly ranges from
4 4.9 to 17.9%,where the risk in HIV patients has been reported to be anywhere from 20 to 37%. This and other reports, suggest that the prevalence rate of Major Depressive
Disorder (MDD) is a staggering 2 to 5 times greater in HIV/AIDS patients than in the general population. It is important to note, however, that a number of patients with
HIV may have experienced depression prior to infection. However, regardless of when these patients began to experience depressive symptoms, it is essential that depression is detected so that it can be treated.9
Despite the high occurrence of depression in this population, many patients go undiagnosed or untreated. In China rates of major depression and suicidal tendency were recorded in 30 HIV patients and 25 matched controls. Lifetime major depression and suicidal tendency was determined via the Chinese composite
International Diagnostic interview (CIDI) - an internationally used structural interview for epidemiologic studies of Psychiatric disorders across cultures that was developed by the World Health Organization (WHO).
Globally, India is the second only to South Africa in terms of number of people living with the disease. As per National AIDS Control
Organization, there are 5.1 million people across India suffering with HIV positive.
Around 38% of these people are women. By the end of May 2008, the total number of
AIDS cases reported in India was 109400 of whom 31994 were women. The UN
Population Division Project that India’s adult HIV prevalence will be peak at 1.9% in
2010. The UN estimates that, there were 2.7 million AIDS deaths in India between
1980 and 2000. A report in 2002 by CIA’s National Intelligence council predicted 20 to 25 million AIDS cases in India by 2010, more than any other country in the World.
5 The number of HIV/AIDS patients with depression in India is difficult to determine. Studies of the National AIDS Control Organization reported that 80% of
HIV positive patients suffering with lifetime depression. The lifetime risk of developing clinical depression in someone without HIV reportedly ranges from 5-
10%, where risk in HIV patients has been reported to be anywhere from 25-50%. This and other reports, suggest that the prevalence rate of Major Depressive Disorder
(MDD) is a staggering 2 to 5 times greater in HIV /AIDS patients than in the general population.
In India, the social reactions to people with AIDS have been overwhelmingly negative. For example, in a study, 36% of people felt that it would be better if infected people killed themselves as they deserved their fate. At the same
34%said that they were not prefer to maintain relationships. AIDS people while one fifth of them stated that AIDS was a curse. As a result, many keep their status secret, fearing of worse response from society. Infact, the HIV positive cases are not literally
AIDS patients. Client carries a profound of physical, psychological and social burden if he/ she is told to undergo HIV test. In addition, living with the HIV/AIDS makes life more complicated and stressful.
Research studies shows that depression is a common problem experienced by HIV/AIDS patients. The investigators have come across many patients who are depressed after they have been diagnosed as HIV/AIDS. Apparently, many of them wanted to end their life due to social stigma. They find it hard to face the family, children, parents, relatives and friends. The financial problems, as well as the future of the family make client’s copying strategy even worse. Suicidal tendency needs an immediate psychiatric remedy to control depression as well as untreated
6 depression can worsen the client’s prognosis and limits future treatment options.
Depression may make it difficult for individuals to maintain healthy interpersonal relation. The experience of the investigator in dealing with patients in the HIV/AIDS, discussion with experts and review of literature have motivated to take up this study.
6.2 REVIEW OF LITERATURE
A review of literature is an essential aspect of research. One of the major functions of review of literature is to ascertain what is already known in relation to the problem of interest and will help in developing a broad conceptual framework in to which a research problem will fit.
Literature is presented under following headings
1. Literature related to prevalence of depression among men or women living
with HIV/AIDS.
2. Literature related to impact of HIV/AIDS on the People.
3. Literature related to strategies adapted to prevent/control depression among
HIV/AIDS patients and to help cope with their illness.
I . LITERATURE RELATED TO PREVALENCE OF DEPRESSION
AMONG MEN OR WOMEN LIVING WITH HIV/AIDS.
Assessed the prevalence of depression among men living with HIV infection in Vietnam and compared the findings with those from a general population survey of Vietnamese men. Between November 2007 and April2008, 584 participants completed a structured questionnaire in Vietnamese that measured self-reported depression. They used the chi2 test to detect differences in prevalence rates within
HIV populations and between our respondents and a general Vietnamese male population. Respondents had a depression rate of 18.7% over a 1-month period, which 7 was substantially higher than that reported in the Vietnamese male population (0.9%).
Rates were highest among men reporting higher levels of stress and more HIV symptoms. Men diagnosed with depression experienced significantly more difficulty than others in accessing medical care.21
Maternal perinatal depression (PND) may interfere with effective perinatal HIV care. In order to begin examining the prevalence and characteristics of
PND in HIV-infected women, we analyzed data from the medical records of all HIV- infected women who had received perinatal care in the Maternal-Child and
Adolescent Center for Infectious Diseases and Virology at LAC/USC Medical Center from 1997 through 2006. Data from 273 individual women (328 live births) were analyzed. Demographic, medical history, psychosocial, pregnancy related, and HIV- related factors measured during the perinatal period were examined for an association with PND using multivariate logistic regression with generalized estimating equations to account for the within subject correlation due to multiple births per mother. The overall prevalence of PND was 30.8%. Multivariate analysis showed that PND was significantly associated with substance abuse during pregnancy (odds ratio [OR] =
2.81, 95% confidence interval [CI]: 1.35-5.82) and past history of psychiatric illness
(OR = 3.72, 95% CI: 2.06-6.71). Compared to mothers with CD4 nadir greater than
500 cells/mm3, mothers with a CD4 nadir during pregnancy #200 cells=mm3 were
3.1 times more likely to experience PND (OR = 3.01, 95% CI:1.32-6.88). Women who had antiretroviral (ARV) medications adherence problems during pregnancy were more likely to experience PND than women who were adherent (OR = 2.14,
95% CI: 1.08-4.23). These preliminary results suggest that rates of PND among HIV- infected women are substantial. We conclude that pregnant HIV-infected women
8 should be routinely screened for PND. Prospective studies examining the bio-psycho- social markers of PND in HIV-infected women are indicated.7
HIV/AIDS continues to be a significant public health problem. Millions of people worldwide are infected with this virus daily, and thousands die yearly of
AIDS-related illnesses. Despite rapid advances in our knowledge about HIV and its mode of transmission, we have been unable to find a cure or prevent new infections.
Psychiatric co- morbidity is associated with HIV/AIDS: as a risk factor for HIV infection, a co- morbidity of HIV infection, sequelae of HIV/AIDS, and a potential mediator for progression to AIDS. In this article, we focus on depression, which is prevalent in HIV/AIDS. We review the evidence associating depression with HIV, the challenges in recognizing depression in HIV-positive individuals, and the psychopharmacologic strategies known to be effective in the treatment of HIV- positive individuals with depression.8
Previous research has been inconsistent in documenting a strong relationship between depression and HIV/AIDS, although a recent meta-analysis of studies examining this issue indicates that rates of depression are modestly higher for this population. For the current study, conducted from 2001-2004, we sought to examine rates and types of depressive symptoms in a cohort of patients receiving HIV care at two urban medical centers. These patients were participants in an intervention study examining adherence and mental health in persons triply diagnosed with psychiatric disorders, substance use disorders, and HIV/AIDS. Nearly three quarters of these participants were people of color, two thirds described their sexual orientation as heterosexual, and the vast majority were unemployed. We sought to
9 examine the relationship of depression to patients' adherence to antiretroviral medication regimens (highly active antiretroviral therapy [HAART]). Results obtained from structured clinical interviews and self-report questionnaires indicated that study participants experienced high rates of depressive symptoms, and that 72.9% of participants met criteria for major depressive disorder (MDD). The results of this study offer a detailed view of the incidence and nature of MDDs and depressive symptoms for an urban sample of substance-abusing adults with HIV/AIDS. Given the degree to which depressive symptoms and MDD appear to be prevalent for this group, as well as the observation that these symptoms are amenable to treatment, future research should focus on identifying helpful strategies and interventions for treating these symptoms, effective ways of providing linkages to care, and ways in which standardized assessment and treatment protocols might be adapted to better suit this population.9
The aim of the study was to assess the prevalence of depression among Croatian patients infected with human immunodeficiency virus (HIV) and to make a comparison with patients with other acute and chronic infectious diseases. We assessed the depressive disorder using the Beck Depression Inventory questionnaire
(BDI), without clinical confirmation. The BDI scores were examined in 80 HIV- infected persons and compared to 80 persons with chronic viral hepatitis and 78 with acute infectious diarrhea. All examinees were treated as outpatients at the University
Hospital for Infectious Diseases in Zagreb in March and April of 2003. Prevalence of moderate and severe depression among HIV-infected was 16/80 (20%) with a 95% confidence interval 11% to 29%. Male patients with HIV or chronic viral hepatitis had a significantly higher BDI scores than males with acute infectious diarrhea (p = 0.017,
10 Kruskall-Wallis, d.f. 2). Female patients with HIV infection tended to have a lower
BDI score than females with chronic viral hepatitis or acute infectious diarrhea (p =
0.087, Kruskall-Wallis, d.f. 2). Prevalence of moderate and severe depression among
Croatian HIV-positive patients is higher than the upper estimate for general population. Croatian males with chronic infectious disease have higher rate of depression than those with acute infectious disease.10
Depression is a prevalent and interfering, yet potentially treatable illness commonly co-morbid with HIV/AIDS. In HIV, symptoms and diagnoses of depression have been associated with poor adherence to antiretroviral medication regimens and to accelerated disease progression. This article is a review of the existing literature on the treatment of depression in the context of HIV, including:
(1)psychosocial and behavioral health interventions that directly target Diagnostic and
Statistical Manual of Mental Disorders (DSM) unipolar depressive disorders,(2) psychosocial interventions that indirectly target depressive symptoms, and (3) psychopharmacologic treatment studies for DSM-IV unipolar depressive disorders.
Psychosocial and psychopharmacologic treatments of depression appear to be effective for individuals with HIV. However, additional methodologically rigorous trials are needed for definitive inferences regarding treatment efficacy. Because of the high frequency of depression co-morbid with HIV, and the association of depression with important self-care behaviors in this population, identification of efficacious treatments for depression has the potential to improve both overall quality of life and, potentially, health outcomes.11
11 Although depressive symptoms are common in people living with
HIV/AIDS, theirreported prevalence varies greatly across HIV-positive populations, ranging from 21% to 97%. Comparing these rates is complicated by the varied conceptualization of depression as a major depressive disorder (clinical depression) or depressive symptoms, and by the use of multiple methods of measurement.
Knowledge of predictors of depressive symptoms can assist health care providers in the identification of those who are most at risk. Appropriate diagnosis, treatment, and referral are critical, because depressive symptoms have been associated with poorer disease outcomes. Additionally, self-management symptoms can be used to supplement more traditional treatment methods.12
2. LITERATURE RELATED TO IMPACT OF HIV / ADIS ON THE
PEOPLE
Patients infected with human immunodeficiency virus (HIV) have a higher risk of developing major depressive disorder (MDD) than the general population.
Immunophilins FKBP51 and FKBP52 are expressed in cortical neurons shown that genetic variants in the FKBP5 gene encoding FKBP51 are linked to psychiatric disorders. We sought to determine whether immunophilins are up-regulated in HIV infection. To determine whether FKBP52 and FKBP51 are associated with MDD and/or HIV, we compared protein and gene expression in autopsy tissues from the frontal cortical gray matter. The study cases were divided into five groups: control,
MDD, MDD with psychosis, HIV(+), and HIV(+) with MDD. Gene expression and protein levels were determined by real-time PCR and Western blot analysis of fresh frozen issues. Genotyping of previously published alleles of the FKBP5 gene was also performed. We found correlation of up-regulation of both immunophilins in the HIV-
12 infected groups. In the HIV(+) population with MDD, FKBP4 expression is significantly higher while FKBP5 is more variable. After analyzing the FKBP5 gene for single nucleotide polymorphisms, we found that rs3800373 CC genotype is more frequent in the MDD and MDD/Psychosis groups. We hypothesized that the levels of
FKBP51, as modulator of the nuclear translocation of GR, would be lower in MDD instead, an increase in FKBP51 at both the transcript (FKBP5) and protein level correlated with MDD. Increased FKBP4 expression of correlated to HIV (+) MDD but not to HIV without MDD.15
To evaluate sleep impairment, symptoms of anxiety and depression, and associations with sleep characteristics of sleep in female HIV/AIDS patients.30 female patients with HIV/AIDS were evaluated along with 30 female controls with a mean age of 35.4 years in the study group and 33.1 years in the control group, with: a) the Pittsburgh Sleep Quality Index; b) the Beck Anxiety Inventory; c) the Beck
Depression Inventory. Sleep quality was more impaired in AIDS patients than in those with HIV+ or in controls. The AIDS Patients showed more symptoms of anxiety. There were associations of sleep impairment with anxiety in HIV+ patients; whereas in AIDS patients associations were found between sleep impairment and depression. There was sleep quality in the presence of symptoms of anxiety and depression. In HIV+ patients, sleep impairment was associated with anxiety, while in
AIDS patients sleep impairment was associated with depression.13
Continuing advances in antiretroviral therapy are increasing survival and longevity for people living with HIV. However, factors related to depression and
13 suicidal ideation associated with aging and HIV may mean that the synergistic effects of aging with HIV could place many adults at undue risk for these conditions. Such factors include ageism and stigma, loneliness/decreased social support, neurological changes, declining health, fatigue, changes in appearance, and financial distress.
Potential interventions that address these factors are needed to abate depression and prevent suicidal ideation. Nurses are in key positions to identify and intervene with
HIV-infected and aging patients who may be at risk for depression and suicidal ideation.14
Psychiatric disorders such as bipolar disorder, schizophrenia and depression have long been associated with risk behaviors for HIV, hepatitis C virus
(HCV) and hepatitis B virus (HBV). The US prison population is reported to have elevated rates of HIV, hepatitis and most psychiatric disorders. This study examined the association of six major psychiatric disorders with HIV mono-infection,
HIV/HCV co-infection and HIV/HBV co-infection in one of the nation’s, largest prison populations. The study population consisted of 370,511 Texas Department of
Criminal Justice inmates who were incarcerated for any duration between January 1,
2003 and July 1, 2006. Information on medical conditions and socio demographic factors was obtained from an institution-wide electronic medical information system.
Offenders diagnosed with HIV mono-infection, HIV/HCV, HIV/HBV and all HIV combined exhibited elevated rates of major depression, bipolar disorder, schizophrenia, schizoaffective disorder, non-schizophrenic psychotic disorder and any psychiatric disorder. In comparison to offenders with HIV mono-infection, those with
HIV/HCV co-infection had an elevated prevalence of any psychiatric disorder. This cross-sectional study's finding of positive associations between psychiatric disease
14 and both HIV infection and hepatitis co-infection among Texas prison inmates holds both clinical and public health relevance. It will be important for future investigations to examine the extent to which psychiatric disorders serve as a barrier to medical care, communication with clinicians and adherence to prescribed medical regimens among both HIV-mono-infected and HIV/hepatitis-co-infected inmates.17
This study explored the role of adult attachment style in reported experiences of HIV-related stigma, stress and depression in a diverse sample of HIV+ adults.
Participants (N = 288) recruited from AIDS service organizations were administered anxiety disorder diagnosis. While BI was linked to certain anxiety disorders, we found no evidence to suggest that BI, a diagnosis of an anxiety disorder, and/or depressive symptoms were associated with CD4counts among HIV-positive adults.18
2. LITERATURE RELATED TO STRATEGIES ADAPTED TO
PREVENT / CONTROL DEPRESSION AMONG HIV / ADIS
PATIENTS AND TO HELP COPE WITH THEIR ILLNESS.
Spirituality is a resource some HIV-positive women use to cope with HIV, and it also may have positive impact on physical health. This cross-sectional study examined associations of spiritual well-being, with depressive symptoms, and CD4 cell count and percentages among a non-random sample of 129 predominantly
African-American HIV-positive women. Significant inverse associations were observed between depressive symptoms and spiritual well-being (r = -.55, p =.0001), and its components, existential well-being (r = -.62, p = .0001) and religious well- being (r = -.36, p = .0001). Significant positive associations were observed between existential well-being and CD4 cell count (r = .19, p <.05) and also between spiritual
15 well-being (r = .24, p < .05), religious well-being (r = .21, p < .05), and existential well-being (r = .22, p < .05) and CD4 cell percentages. In this sample of HIV-positive women, spiritual well-being, existential well-being, and religious well-being accounted for a significant amount of variance in depressive symptoms and CD4 cell percentages, above and beyond that explained by demographic variables, HIV medication adherence, and HIV viral load (log). Depressive symptoms were not significantly associated with CD4 cell counts or percentages. A significant relationship was observed between spiritual/religious practices (prayer/meditation and reading spiritual/religious material) and depressive symptoms. Further research is needed to examine relationships between spirituality and mental and physical health among HIV-positive women.19
This investigation examined the interaction of disengagement coping with HIV/AIDS-related stigma and mindful-based attention and awareness in regard to anxiety and depressive symptoms among people with HIV/AIDS. There was a significant interaction in regard to anxiety symptoms. Higher levels of disengagement coping paired with lower levels of mindful-based attention and awareness was related to the greatest degrees of anxiety symptoms, while lower and awareness was related to the lowest levels of anxiety symptoms. Although the interaction for depressive symptoms was not significant, a similar pattern of results was observed.20
Utilizing a heterogenous sample of adults diagnosed with HIV infection, the current study sought to explore associations among age, various dimensions of social support, and psychological and functional well-being. Cross-sectional data
16 capturing subjective and instrumental support, social interaction, behavioral health service utilization, and psychological well-being (ie, positive affect and depressive symptomatology), and physical functioning, were collected from 109 men and women living with HIV. To explore age group differences, participants were stratified by age
(<54 vs. 55+ years). Despite endorsing greater medical co morbidity, older adults reported significantly lower depressive symptomatology and greater positive affect and were less likely to report seeing a behavioral health specialist than their younger counterparts. No age group differences emerged for instrumental support or amount of social interaction. However, older adults reported higher subjective support, which in turn was associated with lower depressive symptomatology, greater positive effect, and non utilization of behavioral health services.21
Prospectively examined the effects of spiritual striving, social support, and acceptance coping on changes in depressive symptoms among adults living with
HIV/AIDS. Participants were 180 culturally diverse adults with HIV/AIDS.
Participants completed measures of spiritual striving, social support, coping styles, and depressive symptoms at baseline, three-month follow-up, and six-month follow- up. A path model showed that spiritual striving had direct and indirect inverse effects on changes in depressive symptoms. The relationship between spiritual striving and depressive symptoms was partially mediated by acceptance coping, but not by social support. Results suggest that people living with HIV/AIDS who strive for spiritual growth in the context of their illness experience less negative affect.22
The authors examined associations between psychosocial variables (coping self-efficacy, social support, and cognitive depression) and subjective health status among a large national sample (N = 3,670) of human immunodeficiency virus (HIV)- positive persons with different sexual identities. After controlling for ethnicity,
17 heterosexual men reported fewer symptoms than did either bisexual or gay men and heterosexual women reported fewer symptoms than did bisexual women.
Heterosexual and bisexual women reported greater symptom intrusiveness than did heterosexual or gay men. Coping self-efficacy and cognitive depression independently explained symptom reports and symptom intrusiveness for heterosexual, gay, and bisexual men. Coping self-efficacy and cognitive depression explained symptom intrusiveness among heterosexual women. Cognitive depression significantly contributed to the number of symptom reports for heterosexual and bisexual women and to symptom intrusiveness for lesbian and bisexual women. Individuals likely experience HIV differently on the basis of socio-cultural realities associated with sexual identity. Further, symptom intrusiveness may be a more sensitive measure of subjective health status for these groups.23
HIV patients are at increased risk for depression. However, a comprehensive set of quality of care indicators for depression in the context of HIV does not exist. We report the results of a recent expert panel convened to develop a comprehensive set of HIV depression quality indicators. We systematically reviewed the depression and HIV depression literature to provide the evidence for the quality indicators. The HIV depression quality indicators were divided into six chapters: general, bereavement, substance abuse, viral hepatitis, cognitive impairment and drug interactions. A modified Delphi expert panel method was used to evaluate the validity and feasibility of the candidate quality indicators. The expert panel included HIV physicians, psychiatrists and a pharmacist, all with experience with HIV depression.
The in-person eleven-member panel rated 80 candidate HIV-depression quality indicators. Indicators were evaluated using main and sensitivity analysis criteria for
18 validity and feasibility. Seventy-four percent (59/80) of the quality indicators met a priori main analysis criteria for validity and feasibility and 61% met sensitivity analysis criteria. Approved indicators that are more specific to HIV depression include: depression screening frequency; depression screening and treatment in the context of hepatitis, optimizing depression and HIV treatment in the context of cognitive impairment; and starting antidepressants at lower doses but advancing to doses typical for the general population. Most adverse medication interaction indicators did not meet main analysis validity criteria. The quality indicators identified in this study provide a useful tool for measuring and informing the quality of HIV-depression care.24
Highly active antiretroviral therapy (HAART) has significantly decreased the morbidity and mortality of persons infected with HIV. The extent of the benefits, however, is not uniform, and certain factors including ethnicity, gender, baseline HIV viral load and CD4+ T lymphocyte count, adherence and intravenous drug abuse are associated with different immunological, virological and clinical outcomes. Mental health illness (MHI) and specifically depression may be associated with worse outcomes, although studies exploring the impact of MHI on HIV outcomes in both the pre-HAART and post-HAART eras have shown mixed results. The objective of the current paper is to review the available literature on the impact of MHI on HIV outcomes in the HAART era.25
Psychological adjustment and coping are central to human immunodeficiency virus (HIV) management. To improve HIV-infected patients'
19 ability to cope with stress, a variety of stress management interventions have been designed and evaluated. This paper provides a review and critique of the stress management literature, including a: (1) synthesis of core components of interventions for HIV-infected people, (2) summary of stress, coping, psychological, and health outcomes, and (3) methodological critique and guidance for future research. They reviewed 21 stress management interventions designed for HIV-infected individuals that included both cognitive and behavioral skills training. Most studies noted positive changes in perceived stress, depression, anxiety, global psychological functioning, social support, and quality of life. However, results were mixed for coping and health status outcomes, and a majority of studies employed only brief follow-up periods, focused on HIV-infected MSM, and did not address HIV-specific stressors.26
Psychological adjustment and coping are central to human immune deficiency virus (HIV) management. To improve HIV-infected patients, ability to cope with stress, a variety of stress management interventions have been designed and evaluated. This paper provides a review and critique of the stress management literature, including a: (1) synthesis of core components of interventions for HIV- infected people, (2) summary of stress, coping, psychological, and health outcomes, and (3) methodological critique and guidance for future research. They reviewed 21 stress management interventions designed for HIV-infected individuals that included both cognitive and behavioral skills training. Most studies noted positive changes in perceived stress, depression, anxiety, global psychological functioning, social support, and quality of life. However, results were mixed for coping and health status outcomes, and a majority of studies employed only brief follow-up periods, focused on HIV-infected MSM, and did not address HIV-specific stressors.27
20 Older adults with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) and chronic depression constitute a growing population of individuals in need of quality nursing care management.
Although the small amounts of research currently available focus on both middle- aged and older adults living with these chronic conditions, this article offers specific suggestions for the nursing care of older adults who have been diagnosed with HIV, have experienced the progression of HIV to AIDS, and who have lived with chronic depression prior to the onset of HIV/AIDS. Given the increasingly significant role that nurses play in the lives of older adults with chronic health conditions, this article aims to provide nurses with a number of interventions associated with 10 nursing diagnoses pertinent to the care of older adults with HIV/AIDS and chronic depression.
The Experiences in Close Relationships Scale, Perceived Stress Scale, CES-D, HIV
Stigma Scale and a health information questionnaire. Adult romantic attachment style was significantly associated with perceived stress, depression and HIV-related stigma.
Results of regression analyses supported contentions that in addition to HIV symptomatology, other psychosocial risk factors such as attachment style and stigma contribute to perceived stress and depression among HIV+ men and women.28
This study examined the relationships between behavioural inhibition
(BI), anxiety disorders, depression and CD4 counts in 456 HIV-infected adults attending primary healthcare HIV clinics in South Africa. Our first hypothesis was that BI would be positively correlated with anxiety disorders and with depression. Our second hypothesis was that BI, anxiety disorders and depression would be negatively correlated with CD4 counts. Participants completed the Retrospective Self-Report of
21 Childhood Inhibition scale (RSRCI), the Center for Epidemiologic Studies Depression scale (CES-D) and the Mini-International Neuropsychiatric Interview (MINI). We found that BI was positively correlated with depression, agoraphobia, social phobia
(social anxiety disorder) and posttraumatic stress disorder (PTSD). In addition, we found that BI, anxiety disorders and depression were not associated with CD4 counts.
Finally, we found no gender effects for BI, depression, CD4 counts or any.16
6.3 STATEMENT OF THE PROBLEM
A descriptive study to assess the level of depression among HIV/AIDS patients in selected hospitals at Bangalore, Karnataka.
6.4 OBJECTIVES OF THE STUDY
1. To assess the level of depression among HIV positive patients.
2. To associate the level of depression with selected demographic variables of HIV
positive patients.
6.5 HYPOTHESIS
H 1: There will be a significant difference between level of depression and selected demographic variables.
H 2: There will be a significant association between the level of depression and HIV patients.
22 6.6 OPERATIONAL DEFINITIONS:
1. DEPRESSION- Depression is characterised by persistent symptoms of
feelings of sadness, helplessness, loss of interest or pleasure in nearly all
activities, fatigue and irritability that continue for a period of two weeks
(Carol and Constant).
In this study depression is characterised by losing all interest in
oneself, feeling of worthlessness and fail to live or the reality of life.
2. HIV POSITIVE PATIENTS-It refers to individuals who are medically
diagnosed by the physician as having HIV by the evidence of ELISA or
Western Blot Test. They are either symptomatic or asymptomatic.
6.7 ASSUMPTIONS
1. HIV / AIDS patients those who are admitted in hospital will have interest to
participate in the study.
2. The Depression level of HIV / AIDS patients may vary according to their age,
education, sex, occupation, family income & relationship.
6.8 DELIMITATIONS
Study is delimited to
The HIV positive patients in selected hospitals at Bangalore,
Karnataka.
23 The HIV positive patients available during the time of data collection.
Those who understand Kannada, Hindi or English.
6.8 PROJECTED OUTCOME
The study will reveal the statistical prevalence of depression among HIV
/AIDS patients. The study will also reveal factors associated with the depression among HIV/AIDS patients.
7. MATERIALS AND METHODS
7.1. SOURCE OF DATA: HIV/AIDS patients who are admitted in the ward of selected hospitals at Bangalore.
7.1.1 RESEARCH DESIGN AND APPROACH: A descriptive study to assess the level of depression among HIV/AIDS patients.
7.1.2 SETTING: Selected hospitals at Bangalore.
7.1.3 POPULATION: HIV/AIDS patients who are admitted in the ward of selected hospitals at Bangalore.
7.2 METHODS OF COLLECTION OF DATA
7.2.1 SAMPLING TECHNIQUE: Convenient sample technique.
7.2.2 VARIABLES UNDER THE STUDY
ATTRIBUTE VARIABLE: Sex, age, education, religion, marital status, types of family, place of residence, habits, occupation, monthly income etc.
7.2.3 SAMPLE SIZE: 100
24 7.2.4 DURATION OF STUDY: data collection period is limited to 1 month.
7.2.5 INCLUSION CRITERIA FOR SAMPLING
HIV/AIDS patients who are in hospitals during data collection.
Patients who are diagnosed for the first time as having HIV and have not
received antidepressant drugs.
Those who are able to communicate in English, Kannada and Hindi.
7.2.6 EXCLUSION CRITERIA FOR SAMPLING
Patients those who are not willing to participate.
Patients who are on antidepressant drug.
Patients those who are not present at the time of study.
7.2.6 INSTRUMENT NEEDED TO BE USED
A structured interview schedule is selected on the basis of objectives of
the study.
7.2.8 METHOD OF DATA COLLECTION: Written permission will be taken from the selected sectors, Bangalore for conducting study. Written consent will be obtained from the study participants. Adequate care will be taken for protecting the subject from potential risk. The data will be collected by the investigator itself.
7.2.9 LIMITATIONS
Study will be limited to 25 HIV / ADIS patients available during the time of data collection.
HIV / ADIS patients those who are willing to participate in the study
7.2.10 PLAN FOR ANALYSIS
1. The collected data will be entered in a large data sheet or to the computer.
2. The mean, Mode and Meridian will be used to analyse the percentage of depression among HIV/AID patients.
7.3 DOES THE STUDY REQUIRE ANY INVESTIGATION TO BE
CONDUCTED ON PATI ENTS OR OTHER HUMAN OR ANIMALS?
Yes, study will be conducted on HIV/AIDS patients to assess the level of depression by giving structured interview schedule on the basis of the objectives of the study.
Has ethical clearance been obtained from your institution in case of 7.3?
Yes, informed consent will be obtained from the concerned subjects &
authority.
Privacy, confidentiality and anonymity will be guarded.
Scientific objectivity of the study will be maintained with honesty and
impartiality.
26 7.4 ETHICAL COMMITTEE:
A DESCRIPTIVE STUDY TO ASSESS THE LEVEL OF
DEPRESSION AMONG HIV / ADIS PATIENTS IN Title of topic SELECTED HOSPITALS AT BANGALORE,
KARNATAKA.
Name of the RAJESH.E.K
candidate
Course & the M.Sc Nursing
subject Psychiatric Nursing Speciality
Name of the Mrs. Gracy. M.Sc Nursing
guide
Ethical Approved
committee
27 8. REFERENCES:
1. HIV/AIDS- Basic facts. Karnataka state prevention society; 2000 March; 8-9.
2. Park K. Text book of preventive and social medicine.18th edition. Banarsidas
Bhanot publishers; 2007.
3. Niraj Ahuja. A short text book of psychiatry. 4th edition. New Delhi: Jaypee
Brothers medical publishers; 1999.
4. Mary C. Townsend. Psychiatric mental health nursing. 5th edition. Published by
Jaypee brothers.
5. Batiya MS. Essential of Psychiatry. 3rd edition. New Delhi: CBS publishers; 2000.
6. Nambi S. Psychiatry for nurses. 1st edition. New Delhi: Jaypee brothers medical
publishers; 1998.
7. Kapetanovic S, Christensen S, Karim R, Lin F, Mack WJ. Corerelates of perinatal
depression in HIV-infected women. AIDS patient care STDs. 2001 Feb;23(2);
101-8.
8. Benton TD. Depression and HIV/AIDS. Curr Psychiatry Rep.2008 Jan;10 (3):280-
5.
9. Berger-Greenstein JA, Cuevas CA, Brady SM, Keane TM. Major depression in
patient with HIV/AIDS and substance abuse. AIDS patient care STDs. 2007- Dec;
21(12):942-55.
28 10. Kolaric B, Tesic V, Ivankovic D, Begovoc J. Prevalence of moderate and severe
depression among Croatian PATIENTS infected with human immune deficiency
virus. Coll Antropol.2006 Dec;30 suppl 2:85-8.
11. Olatanji BO, Mimiago MJ, O’cleirigh C, Safren SA. Review of treatment studies
of depression in HIV. Top HIV med. 2006 Aug- Sep;14(3):112-24.
12. Eller LS. Depressive symptoms in HIV disease. Nurs Clin North Am.2006
Sep;41(3):437-53,
13. Tatro ET, Everall IP, Masliah E, Hult BJ, Lucero G, Chana G. Differential
expression of immunophilins FKBP51 and FKBP52 in the frontal cortex of HIV-
infected PATIENTS with major depression disorder. J Neuroimmune
Pharmacol.2009 Jan;4(2):218-26.
14. Janqueira P, Bellucci S, Rossini S, Reimao R. Women living with HIV/AIDS:
sleep impairment, anxiety and depression symptoms. Arq Neuropsiquiatr.2008
Dec;66(4):817-20.
15. Vanc DE, Moneyham L, Fordham P, Struzick TC. A model of suicidal ideation in
adults aging with HIV. J Assok Nurses AIDS care. 2008Sep-Oct;19(5):375-84.
16. Baillargeon JG, Paar DP, Giordamo TP, Murray O, Raimer VG, Diamond PM.
Psychiatric disorders, HIV infection and HIV/hepatitis co-infection in the
correctional setting. AIDS care. 2008 Jan;20(1):124-9.
17. Rigga SA, Vosvick M, Stallings S. Attachment style, stigma and psychological
distress among HI V positive adults. J Health Psychol. 2007 Nov;12(6):922-36.
29 18. Fincham D, Smit J, Carey P, Stein DJ, Seedat S. The relationship between
behavioural inhibition, anxiety disorders, depression and CD4 counts in HIV
positive adults. AIDS care.2008 Nov;20(10):1279-83.
19. Dalmida SG, Holstad MM, Diirio C, Laderman G. Spiritual well being, depressive
symptoms, and immune status among women living with HIV/AIDS. Women
Health. 2009 Mar-May; 49(2-3):119-43.
20. Gonzalez A, Solomon SE, Zvolensky MJ, Miller CT. The interaction of mindful-
based attention and awareness and disengagement coping with HIV/AIDS- related
stigma in regard to concurrent anxiety and depressive symptoms among adults
with HIV/AIDS. J Health Psychol.2009 Apr;14(3):403-13.
21. Mavandadi S, Zanjani F, Ten Have TR, Oslin DW. Psychological well-being
among individuals aging with HIV: The value of social relationship. J Aquir
immune Defic syndr.2009 May1;51(1): 91-8.
22. Perez JE,Character M,Koopman C , Vosvick M,Gore-Feiton C,Spiritual
Striving,acceptance coping,and deprseeive symptoms among adults living with
HIV/AIDS.J Health Psychol.2009 Jan;14( 10): 88-97.
23. Mosac KE, Weinhardt LS, Kelly JA, Chesney MA, Morin SF. Influence of
coping, social support, and depression on subjective health status among HIV-
positive adults with different sex identities. Behav med. 2009 winter;34(1):133-
44.
24. Pyne JM, Asch SM, Lincourt K, Kilbourne AM. Quality indicators for depression
care inHIV PATIENTS. AIDS care.2008 Oct;20(9):1075-83.
30 25. Hartzell JD, Janke IE, Weintrob AC. Impact of depression on HIV outcome in the
HAART era. J Antimicrob chemother.2008 Aug;62(2):246-55.
26. Brown JL, Vanable PA. Cognitive-behavioural stress management interventions
for persons living with HIV: a review and critique of the literature. Ann Behave
Med.2008 Feb;35(1):26-40.
27. Himelhocoh S, Medoff DR, Oyeniyi G. Efficacy of group psychotherapy to
reduce depressive symptoms among HIV-infected individuals: a systematic
review and meta –analysis. AIDS patient care STDs. 2007 Oct;21(10):732-9.
28. Petrovic K. Nursing care management of older adults with HIV/AIDS and chronic
depression. Care manag J.2006 Fall;7(3):115-20.
29. American Psychiatric Association. Diagnostic and Statistical Manual of Mental
Disorders. 4th edition. Washington. DC: Author.
30. Esposito CA, Steel Z, Gioi TM, Huyen TT, Tarantola D. The prevalence of
depression among men living with HIV infection in Vietnam. Am J Public Health
2009 Oct;99 suppl 2: S439-44.
31. Marzuck P, Tierney H, Tardiff K. Increased risk of suicide in persons with AIDS.
JAMA 1988; 259:1333-1337.
32. Catalan J, Klimest, Day A. The psychosocial impact of HIV infection in gaymen:
controlled investigation and factors associated with psychiatric morbidity. Br J
psychiatry 1992;161: 774-778.
31 9. SIGNATURE OF THE
CANDIDATE
10. REMARKS OF THE GUIDE HIV/AIDS patients committing suicide is common. In
our country depression leads to suicide. By assessing
the level of depression, the statistics can be estimated.
11. NAME AND MRS. GRACY
DESIGNATION OF M.SC NURSING IN MENTAL HEALTH NURSING
11.1 GUIDE
11.2 SIGNATURE
11.3 CO-GUIDE
11.4 SIGNATURE
11.5 HEAD OF MRS. GRACY M.SC NURSING DEPARTMENT
11.6 SIGNATURE
12.1 REMARKS OF THE
PRINCIPAL 12.
12.2 SIGNATURE
32