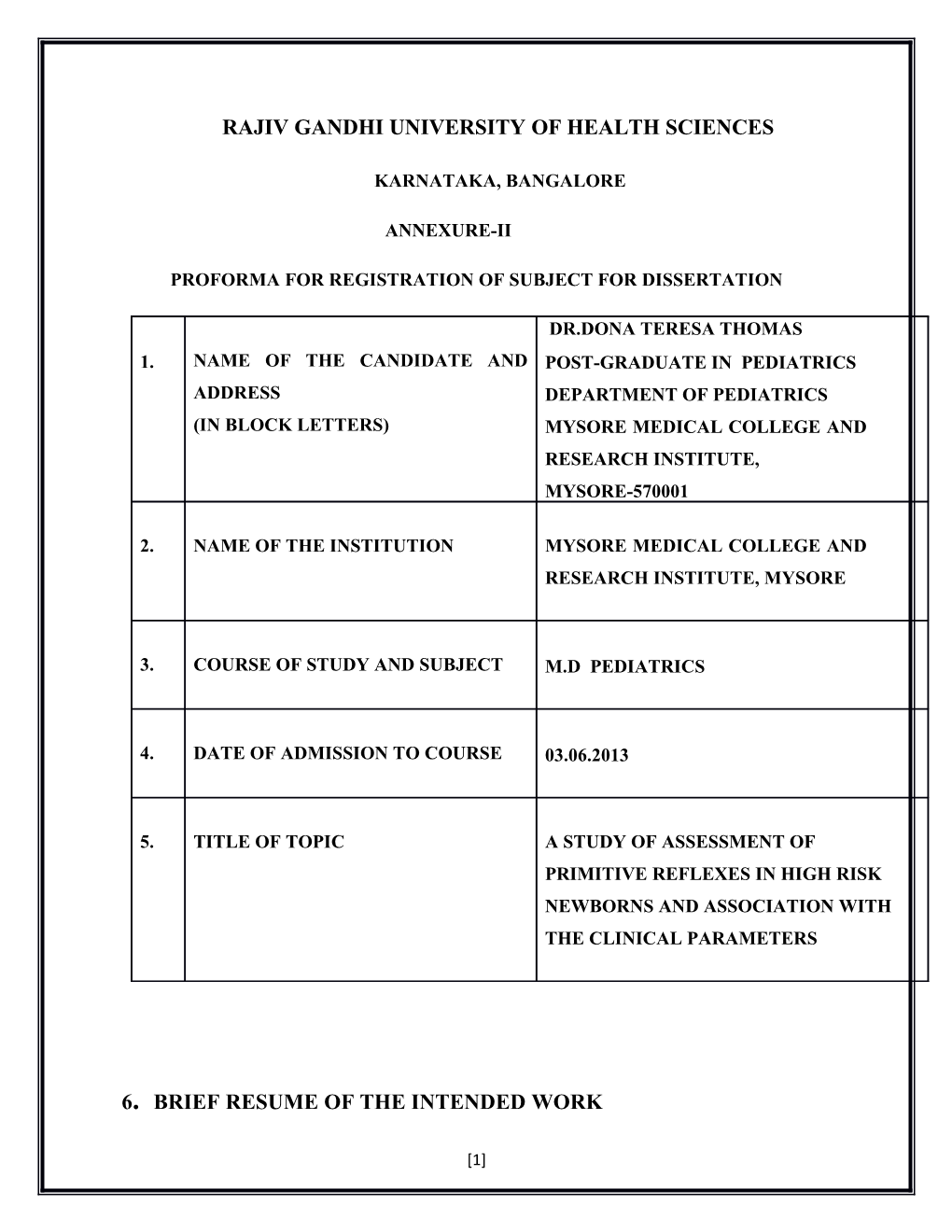
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES
KARNATAKA, BANGALORE
ANNEXURE-II
PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION
DR.DONA TERESA THOMAS 1. NAME OF THE CANDIDATE AND POST-GRADUATE IN PEDIATRICS ADDRESS DEPARTMENT OF PEDIATRICS (IN BLOCK LETTERS) MYSORE MEDICAL COLLEGE AND RESEARCH INSTITUTE, MYSORE-570001
2. NAME OF THE INSTITUTION MYSORE MEDICAL COLLEGE AND RESEARCH INSTITUTE, MYSORE
3. COURSE OF STUDY AND SUBJECT M.D PEDIATRICS
4. DATE OF ADMISSION TO COURSE 03.06.2013
5. TITLE OF TOPIC A STUDY OF ASSESSMENT OF PRIMITIVE REFLEXES IN HIGH RISK NEWBORNS AND ASSOCIATION WITH THE CLINICAL PARAMETERS
6. BRIEF RESUME OF THE INTENDED WORK
[1] 6.1 NEED FOR THE STUDY
Assessment of primitive reflexes is one of the earliest, simplest, and most frequently used assessment tools among health care providers for newborns and young infants. Primitive reflexes are brainstem-mediated, automatic movements which may begin as early gestation week 25-26,and which are fully present at birth in term newborns [1, 2]. Primitive reflexes start to disappear when the central nervous system matures and voluntary motor activities replace them [2]. The normal age-appropriate response is related to the development of normal motor function of newborns or infants.
In general clinical settings, the responses of primitive reflexes have been categorized mostly as dichotomous responses such as normal/abnormal or present/absent. However, primitive reflexes often present various degrees of response, which may be meaningful in the neurological capability to stimulus. Persistent, vigorous, weak, or unsymmetrical responses are closely-linked with neurological impairment in full term [3] and high-risk newborns [2].
While not all primitive reflexes are uniformly present in preterm newborns [2], how the diversity of responses of reflexes are related to clinical conditions and how clinicians can interpret them in a neurological context are unclear. Subtle changes of primitive reflex could be valuable indicators of current medical conditions and potential future health and developmental outcomes while newborns grow up.
Of the primitive reflexes, the sucking, Moro and Babinski reflexes are frequently documented in the literature due to their important roles. The sucking reflex plays a critical role in oral feeding in coordination with breathing and swallowing, and is essential for nutrition intake for survival and growth. The Moro reflex is an involuntary protective motor response against abrupt disruption of body balance or extremely sudden stimulations [2]. The Babinski reflex involves the extensor and flexor of the foot as a nociceptive motor responseof pyramidal tract [4]. Understanding these three reflexes might be more valuable in the neuro-behavioral examination of newborns considering their value for survival, protection, and development. The present study is undertaken to
[2] evaluate three representative primitive reflexes, the sucking, Moro and Babinski reflexes in high-risk and preterm newborns. The specific study purposes are to describe various levels of their responses and to explore relationships among the primitive reflexes and various clinical conditions in high risk newborns.
High risk newborns who are 25 weeks or older gestational age with any of the following will be included in the study
▸ 1. Preterm newborns with gestation <37 weeks.
▸ 2. Perinatal asphyxia - Apgar score 3 or less at 5 min and/or hypoxic ischemic encephalopathy
▸ 3. Seizures
▸ 4. Infections – meningitis and/or culture positive sepsis
▸ 5. Respiratory distress
.The incidence of preterm births in india is 14.5% according to nnpd 2002-2003[5]. The incidence of perinatal asphyxia is 5 % according to nnpd 2002-2003(5).The incidence of neonatal seizures in india is 1% according to national neonatal perinatal data base 2002- 2003[5]. The incidence of neonatal sepsis is 3% according to nnpd 2002-2003[5]. The incidence of respiratory distress in newborns is 1.9% according to nnpd 2002-2003[5].
6.2 REVIEW OF LITERATURE 1) In 1970s Capute A J,et al published a primitive reflex profile where seven primitive reflexes were graded on a 0 to 4+ scale. The reflexes studied were the asymmetrical tonic neck reflex, the symmetrical tonic neck reflex, the tonic labyrinthine reflex, the positive support reflex, the derotational righting reflex, the moro reflex and the gallant reflex. Moros reflex was graded as follows Grading: 0 = absent, 1 = some abduction or extension, no adduction or flexion, 2 = abduction and extension, followed by some adduction and/or flexion, 3 = complete Moro (abduction and extension, followed by strong adduction and flexion),
[3] 4 = complete Moro with arching of the back and/or opisthotonic posturing.[3]
2) In 1980 Paul J Marquis conducted a study in north carolina intensive care nursery on vlbw infants < 1501 g. Primitive reflexes and motor development were evaluated in 127 very low birth weight infants at 4 months corrected age. The asymmetric tonic neck reflex, tonic neck reflex and moros reflex were assessed for each child. The vlbw infants retained stronger primitive reflexes and exhibited a significantly higher incidence of motor delays than term infants. Significant correlations existed between the strengh of primitive reflexes and early motor development for vlbw infants. This study cofirms a higher incidence of motor delays among vlbw infants and demonstrates a clear association between retained primitive reflexes and delayed motor development in vlbw infants[6].
3) In 1983 a longitudinal study conducted at Johns Hopkins hospital describes the pattern of appearance of eight primitive reflexes in a population of 47 viable extremely premature infants, beginning as early as 25 wk post conceptional age . Three patterns emerged: 1) the upper and lower extremity grasp reflexes were present in all premature infants, from 25 wk and beyond, 2) the Moro, asymmetric tonic neck reflex and Galant (lateral trunk incurvature reflex) were present in some premature infants as early as 25 wk PCA, and in the majority by 30 wk PCA, and 3) the lower extremity placing, positive support, and stepping were occasionally present prior to 30 wk PCA, yet were not uniformly present and/or complete even at term. In each case, the primitive reflex became stronger, more complete, more consistently elicited and more prevalent with increasing post conceptional age[7].
4) .In 2008 Sohn et al conducted a cross-sectional descriptive study from September 2008 to June 2009 at the NICU of a university hospital located in Korea on sixty seven high- risk newborns including full-term infants.
The sucking reflex presented a normal response most frequently (63.5%), followed by Babinski reflex (58.7%) and Moro reflex (42.9%). While one-third of newborns presented an abnormal Moro reflex (38.1%) or abnormal Babinski reflex (33.3%), only
[4] 11% of newborns presented an abnormal response of the sucking reflex. Absence responses were most frequent at the sucking reflex (25.4%), followed by the Moro reflex (19.0%) and Babinski reflex (7.9%). Newborns who presented normal sucking and Babinski reflex responses were more likely to have older gestational age, heavier birth and current weight, higher Apgar scores, shorter length of hospitalization, better respiratory conditions, and better mental status assessed by ICS, but not with Moro reflex. A considerably high number of high-risk newborns (36%) presented an abnormal or absent sucking reflex. The mental status as assessed by ICS also showed a statistically significant association with the sucking reflex. Particularly, the mean ICS score of the newborns presenting an abnormal or absent sucking reflex response < 9, which is a cut- off point for the normal mental status of infants . Among the three primitive reflexes, the Moro reflex presented quite different patterns with the clinical conditions of the newborns from the other two reflexes, while very similar response patterns were observed in the sucking and Babinski reflexes. Moro reflex presented as the least frequent normal response and most frequent abnormal response. In the study, morbidity-related factors such as LOH, Apgar scores, and ICS total scores were statistically associated with the sucking and Babinski reflexes, but not the Moro reflex. [8]
5) In 2013, Bijesh S, Jyoth Singh and H P Singh, conducted a study on Moro response qualitatively to determine normative values for latency interval and other components of a normal response. The study was conducted on healthy full term newborns in Gandhi memorial hospital and shyam shah medical college. The range for latency interval of Moro response was found to be 0.41-0.49 seconds. The time taken for optimal Moro response was 0.91-1.04 seconds and the total duration for Moro response was 2.34-2.59 s. Hyperexcitability (short latency) may indicate behavior problems in later life like short concentration span, mood instability and learning difficulty while delayed excitability (long latency) may indicate severe nervous system pathology.[9]
6) J van Gijn states about babinski reflex
[5] The plantar response is a reflex that involves not only the toes, but all muscles that shorten the leg. In the newborn the synergy is brisk, involving all flexor muscles of the leg; these include the toe 'extensors', which also shorten the leg on contraction and therefore are flexors in a physiological sense. As the nervous system matures and the pyramidal tract gains more control over spinal motor neurons the flexion synergy becomes less brisk, and the toe 'extensors' are no longer part of it. The toes then often go down instead of up, as a result of a segmental reflex involving the small foot muscles and the overlying skin, comparable to the abdominal reflexes. The reflex effects in the human leg on stimulation of the sole are completely analogous to those in animals. This is especially clear in neonates, provided the plantar surface is not stimulated too gently, in which case a grasp reflex occurs. [10] 6.3 OBJECTIVES OF THE STUDY
1) To assess and grade three primitive reflexes sucking, babinski and moros reflex in high risk newborns. 2) To explore relationships among primitive reflexes and clinical variables of these newborns
7. MATERIALS AND METHODS
7.1 Source of data
A. Total number of subjects = 72 High risk newborns delivered at cheluvamba hospital attached to mysore medical college and research institute with the following inclusion criteria. Sample size was calculated with the incidence of high risk newborns of 5 % at a 0.05 significance level using formula z2pq/d2 where z=1.96,p=prevalence, q=1-p,d=margin of error.
B. Inclusion criteria 1. Preterm newborns with gestational age <37 weeks
[6] 2. Perinatal asphyxia - Apgar score 3 or less at 5 min and/or hypoxic ischemic encephalopathy 3. Seizures 4. Infections – meningitis and/or culture positive sepsis 5. Respiratory distress C. Exclusion criteria 1. Newborns transferred from other hospitals. 2. Newborns with congenital, genetic or skeletal disorders. 3. Newborns who had received sedatives. 4. Maternal history of substance abuse or alcoholism.
7.2 Methods of Collection of Data The assessment of the sucking, Moro and Babinski reflexes will be performed on day 3 of life. This is to permit the newborns to become stable in the extrauterine environment after the usually necessary critical care had been provided. Newborns will be examined while they are awake and lying comfortably on their backs. Examinations will be avoided within 1 hour of feeding or direct contact with NICU staff or parents. Behavioral and mental status will be assessed as a baseline state of newborns immediately before examining primitive reflexes. The newborns’ behavioral status is assessed using the Anderson Behavioral State Scale (ABSS) by observing five areas including the extent of eye openness, patterns of respiration, body movement, muscle tension and crying . The score ranges from 1 to 12 (1= Regular quiet sleep,2=irregular quiet sleep,3=active sleep 4=very active sleep,5=drowsy,6=alert inactivity,7=quiet awake,8=active,9=very active,10=fussing, 11=crying and 12=hard crying).
The newborns’ mental status is evaluated using the Infant Coma Scale (ICS), which was developed by modification of the pediatric Glasgow Coma Scale (GCS). ICS evaluates the mental status of high-risk newborns in eye openness, verbal response and motor response. The total score of ICS can range from 3-15, and is interpreted just like GCS (i.e., higher score corresponding to a more alert state). Infant coma scale is as follows
[7] • Eye Response :1)Opening spontaneously 2)Opening to speech 3)Opening to pain 4)No response
• Verbal response:1)Smiles, oriented to sounds 2)Cries but consolable 3)Inconsistently inconsolable 4)Inconsolable, agitated 5)No verbal response
• Motor response:1)Moves spontaneously 2)Withdraws from touch 3)Withdraws from pain 4)Abnormal flexion to pain 5)Extension to pain 6)No motor response
Length of hospitalization will be determined following discharge through medical record review. Each reflex is examined up to five times if the newborn showed no response or if response was ambiguous to obtain best positive responses and each reflex graded as 0 for absence 1 for abnormal and 2 for normal. The sucking , babinski and moros reflexes are assessed and classified and analysed for relationships with the clinical parameters of newborns. The clinical parameters consist of continuous and categorical variables. Continuous variables include: 1) Gestational age 2) Birth weight 3) Current weight 4) Length of hospitalization 5) Apgar at 1 min 6) Apgar at 5 min 7) Behavioural status as assessed by ABSS 8) Mental status as assessed by ICS. Categorical variables include: 1) Respiratory condition (Self only/ Self with assist/ventilator dependent) 2) Risk group (physiological risk group for simple preterm newborns without any pathologic conditions / pathological risk group if pathological conditions were evident in addition to prematurity) 3) Preterm birth ( Yes/No). All high risk newborns included in the study will be broadly categorized into whether preterm or full term and whether physiological or pathological risk type as mentioned above.
[8] Data analysis details Type of study: Explorative study
Sampling : Purposive sampling technique
Statistical methods used:
1. Descriptive statistics
2. One way ANOVA with post hoc test ( For continuous variables)
3. Chi-square test (For categorical variables)
4. Contigency table analysis
Using SPSS for windows (version 16)
7.3 Does the study require any investigation/intervention to be conducted on patients/ humans/animals - NO
7.4 Has ethical clearance been obtained from your institution in case of 7.3 ? Yes. Form enclosed 7.5 Duration of study: 18 months
8. LIST OF REFERENCES:
1. Gardner SL, Carter BS, Enzman-Hines MI, Hernandez JA. Merenstein & Gardener’s Handbook of Neonatal Intensive Care. New York: Mosby; 2011.
2. Zafeiriou DI. Primitive reflexes and postural reactions in the neurodevelopmental examination. Pediatr Neurol.2004;31(1):1-8.
3. Capute AJ, Accardo PJ, Vining EP, Rubenstein JE, Walcher JR, Harryman S, Ross A. Primitive reflex profile. A pilot study. Phys Ther. 1978;58(9):1061-1065.
[9] 4. Kumhar GD, Dua T, Gupta P. Plantar response in infancy. Eur J Paediatr Neurol. 2002;6(6):321-325
5)Report of the National Neonatal Perinatal data base (National Neonatology Forum) 2002-03.
6)Marquis P J, Ruiz NA, Lundy MS, Dillard RG. Retention of primitive reflexes and delayed motor development in very low birth weight infants. J Dev Behav Pediatr.1984Jun;5(3):124-6 19)
7) M. C. Allen and A. J. Capute. The evolution of primitive reflexes in extremely premature infants. Pediatric Research.1986;20(12):1284–1289
8)Sohn M., Ahn Y, & Lee, S. Assessment of Primitive Reflexes in High-risk Newborns. J Clin Med Res. 2011;3(6):285-90
9)Bijesh S, Jyothi Singh, and H P Singh. Latency Intervals of Moro Response; A Valuable neuroscreening Tool. Indian Pediatr.2013Jul;50(7):705-706
10) J van Gijn. The Babinski Reflex. Postgrad MedJ3 1995;71(841):645-648
9. SIGNATURE OF THE CANDIDATE:
Dr. DONA TERESA THOMAS
[10] 10. REMARKS OF THE GUIDE: Assessment of primitive reflexes in high risk newborns will help us to prognosticate future neurological outcome and hence plan for early interventional measures.
11. NAME AND DESIGNATION OF 11.1 GUIDE : Dr. B. KRISHNAMURTHY PROFESSOR AND HEAD DEPARTMENT OF PEDIATRICS MYSORE MEDICAL COLLEGE AND RESEARCH INSTITUTE, MYSORE
11.2 SIGNATURE: 11.3 CO-GUIDE (IF ANY): 11.4 SIGNATURE:
11.5 HEAD OF THE DEPARTMENT: Dr. B. KRISHNAMURTHY PROFESSOR AND HEAD, DEPARTMENT OF PEDIATRICS MYSORE MEDICAL COLLEGE AND RESEARCH INSTITUTE, MYSORE
11.6 SIGNATURE:
[11] 12 12.1: REMARKS OF DEAN AND DIRECTOR :
12.2: SIGNATURE:
ETHICAL COMMITTEE CLEARANCE
TITLE OF THE DISSERTATION: “A STUDY OF ASSESSMENT OF
PRIMITIVE REFLEXES IN HIGH RISK NEWBORNS AND ASSOCIATION
WITH THE CLINICAL PARAMETERS”
NAME OF THE CANDIDATE : Dr. DONA TERESA THOMAS
SUBJECT : M.D. PEDIATRICS
1. NAME OF THE GUIDE : Dr. B.KRISHNAMURTHY, M.D,DCH PROFESSOR & HEAD DEPT OF PEDIATRICS MYSORE MEDICAL COLLEGE & RESEARCH INSTITUTE, MYSORE
2. APPROVED/ NOT APPROVED : APPROVED (if not approved, suggestions)
[12] MEDICAL SUPERINTENDENT MEDICAL SUPERINTENDENT K.R. Hospital Cheluvamba Hospital Mysore Mysore
PROFESSOR& HEAD PROFESSOR& HEAD Dept of Medicine Dept of Surgery MMC&RI MMC&RI Mysore Mysore SUPERINTENDENT LAW EXPERT PKTB Hospital Mysore
DIRECTOR & DEAN
Mysore Medical College & Research Institute, Mysore
[13]